Abstract
Obesity is a civilization disease that promotes the emergence and development of many diseases, such as type II diabetes, cardiovascular, and some cancers. It directly affects the length and quality of life. The purpose of this retrospective study was to show the short- and long-term results of weight loss after laparoscopic adjustable gastric banding (LAGB) as well as to assess the results of the procedure and the percentage of reoperations. Case series analysis included 228 subsequent patients who underwent LAGB due to obesity. In the postoperative period, there was a gradual reduction in body weight, especially in the first 24 months after surgery. After 3 years, no further weight reduction was observed, and sometimes, a slight increase in weight was observed 5 years after surgery; the trend in weight reduction over the entire time period was significant. A similar result was found for percentage of BMI loss (%BMIL) and percentage of excess body weight loss (%EWL), especially in the first 36 months after surgery. Our study confirmed the good early results and low effectiveness of laparoscopic adjustable gastric banding in the long-term treatment of pathological obesity. On the other hand, the simplicity and safety of the procedure, the minimal effects of malnutrition, the low number of early complications, and the total reversibility or conversion procedure for any other bariatric surgery are the strengths of laparoscopic adjustable gastric banding for a selected group of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a civilization disease that promotes the emergence and development of many diseases, such as type II diabetes, cardiovascular and musculoskeletal disorders, and some cancers. It directly affects the length and quality of life. The percentage of populations of overweight and obesity in Poland has doubled in the last 40 years, as in other developed countries [1].
According to data from the World Health Organization (WHO) in 2016, 39.3% of adults in Poland are overweight, and 23.1% are obese.
Due to the low effectiveness and lack of lasting effects of conservative treatment for extreme obesity, according to the results of current scientific studies, bariatric surgery is the only effective treatment method [2, 3]. Bariatric surgery is no longer limited by excessive body weight, and the metabolic effects of surgical procedures leading to the disappearance of obesity complications are equally important [2, 4]. It has been proven that bariatric surgery extends the life of operated patients [5, 6] and improves its quality [7]. Laparoscopic surgery, as a minimally invasive and safe technique, has been developed for bariatric surgery and successfully included in the area of obesity [8, 9]. Adjustable gastric banding was first performed with a laparoscopic approach by Belachew et al. in 1993 and quickly became one of the most types of common bariatric surgery [10]. Historically, gastric banding was first described in 1983 by Bo and Modalsky, while in 1986, Kuzmak performed his first operation with the implantation of an adjustable band consisting of an inflatable silicon device [11]. The laparoscopic implantation of an adjustable gastric band in Poland was first performed by Wylezol et al. in 1998 [12]. The original surgical technique of LAGB was modified by Belachew. The outcomes of the surgical technique included a reduction in the volume of the pouch and abridgment of the distance of the band to the esophagogastric junction; it was also a modified technique for tissue preparation to minimize dissection maneuvers, especially posterior dissection of the bursa omentalis, to better handle the band in order to reduce the complication rate [13]. When LAGB was introduced, open surgeries, especially vertical banded gastroplasty (VBG) and Roux-en-Y gastric bypass (RYGB), were the dominant methods. The appearance of LAGB represented a safe and effective alternative that ensured permanent weight loss, with significant improvements in concomitant obesity-related diseases [2]. Due to the poor long-term weight loss results, late complications, and reinterventions, LAGB has become a less popular procedure than sleeve gastrectomy (LSG) or laparoscopic gastric bypass (LRYGB). On the other hand, recently, good long-term weight loss results have been shown in the literature, with an acceptable percentage of complications and fewer interventions [14, 15].
The aim of this retrospective study was to show the short- and long-term results of weight loss after LAGB as well as to assess the results of the procedure and the percentage of reoperations.
Patients and Methods
Case series analysis included subsequent patients who underwent laparoscopic adjustable gastric banding due to obesity in the Clinical Department of General and Bariatric Surgery. Based on the created computer database, 228 patients were included in the study, and the data analyzed were complete. Preoperative data included age, sex, body weight, BMI, and associated diseases. Postoperative data included body weight, BMI, %BMIL, and %EWL. The primary outcome was weight loss, %BMI, and %EWL during follow-up. Secondary outcomes were early and late complications resulting from the surgical procedures. Weight loss efficiency was documented as the change in body mass, BMI, and percentage of BMI lost (%BMIL) from preoperatively to 60 months postoperatively.
The assessment of surgical complications included early complications covering the hospitalization period and those 30 days after discharge from the hospital, as well as late complications noted during postoperative follow-up visits. Gastric leaks (fistulas), bleeding, infections, reoperations, complications associated with implantation of the band system, and any other complications reported in the medical records were analyzed. Significant bleeding was considered to require re-surgery or transfusion ≥ 2 red blood concentrate (RBC). Postoperative follow-up visits were divided into 9 time intervals at monthly intervals (months): 1 month, 3 months, 6 months, 12 months, 18 months, 24 months, 36 months, 48 months, and 60 months.
The study protocol was accepted by the ethical committee of the Medical University of Silesia. Written consent was not needed for this retrospective study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Surgical Procedures
LAGB was performed by the pars flaccida technique. The first step was exposing the His angle. The gastric fundus was retracted inferiorly, and the covering fat was dissected until the left crus of the diaphragm was exposed. Second, a small incision in the gastrohepatic ligament was made to open the lesser omentum, and the retrogastric space for the band was created from the right to the left branch of the crus to the angle of His. The band was implanted around the gastroesophageal junction and fixated using 4 stiches.
Statistical Analysis
The hypothesis about the compatibility of the distribution of studied variables with a normal distribution was analyzed using the Anderson–Darling test. The variables for the normal distribution are represented by the arithmetic mean and standard deviation. Variables for the distribution that differed from normal are presented using the median and quartile range (IQR—interquartile range). Qualitative variables are presented as percentages. Dependent variables at subsequent time points were compared using Friedman’s ANOVA test with acceptance of missing data (Skillings-Mack test), followed by post hoc analysis using the Dunn-Bonferroni test. Statistica 13 PL from StatSoft was used for statistical analyses. In the statistical analysis, the significance level p < 0.05 was adopted.
Results
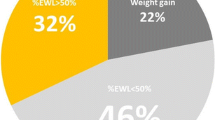
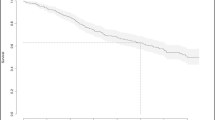
The majority of the 228 patients included in the study were women (79%). The average age was 41 years, the median BMI was 42 kg/m2, and the most common comorbidities were hypertension and diabetes (Table 1). In the postoperative period, there was a gradual reduction in body weight, especially in the first 24 months after surgery. After 3 years, no further weight reduction was observed, and sometimes, a slight increase in weight was observed 5 years after surgery; the trend in weight reduction over the entire time period was significant (Fig. 1). A similar result was found for %BMIL (p < 0.001) and %EWL (p < 0.001), especially in the first 36 months after surgery (Table 2). The percentages of BMIL and EWL were achieved systematically to 3 years postsurgery. From this time, a slight decrease in both parameters was observed, and at 60 months, %BMIL and %EWL achieved results similar to those found 18 months after surgery. There were no significant early postoperative complications in patients after gastric banding. In the late postoperative period, 16 (7.1%) patients had complications related to the introduction of the band system. Band slippage and band migration were the most common complications, which were detected in 8 (3.5%) patients and 3 (1.3%) patients, respectively. Other complications were rare: two patients experienced port malfunctions (one with port displacement and one with port leakage), two patients had high stomal obstructions and one patient experienced drain migration. All patients required re-surgery (7.1%).
Discussion
The number of bariatric procedures is still growing because of the good surgical outcomes associated with excellent weight loss outcomes, the safety of the surgical procedure, and the beneficial effects on comorbidities [16]. Recent data from national registries have demonstrated that the most commonly performed bariatric procedures include LRYGB, SG, and LAGB [17, 18]. LAGB is the most popular bariatric procedure because of its simplicity and lower rate of early complications, but due to its long-term weight loss results and high rates of complications and reinterventions, it has become a less popular procedure than LRYGB and SG. According to the IFSO Global Registry Report [17] and American Society for Metabolic and Bariatric Surgery [19], the gastric banding is still declining among the performed bariatric procedures, and the number of LAGB procedures in these registries ranges from 1.1 to 5%. At present, the number of LAGB procedures in Poland constitutes 7% of bariatric operations [20].
LAGB is not the most effective bariatric surgery for weight loss outcomes compared with other procedures, but it is associated with low mortality and morbidity in the early postoperative period, as well as shorter operative times and shorter hospital stays [21]. On the other hand, the available literature shows that LAGB is a safe procedure with acceptable weight loss; these studies have shown that the LAGB-associated percentage of excess weight loss ranges from 40 to 65% and from 35 to 68% at 3-year and 5-year follow-ups, respectively [22]. Other analyses have also shown effective results, with excess weight loss percentages of 48% and 47% after LAGB at ≥ 5 and ≥ 10 years, respectively [23].
Among the patients subjected to our observation, the largest weight reduction, %BMIL, and %EWL occurred in the first 3 years after surgery, and no further weight loss and sometimes a slight increase were observed during further follow-up. The percentage of excess weight loss at 3 and 5 years was 41% and 30%, respectively. Similar results were obtained by other authors, who showed that the 5-year mean percentage of excess weight loss during the observation period was 34% [24]. However, a recent analysis showed that this effect was not permanent with long-term observation over 7.5 years [25].
Recent meta-analyses showed that short- and medium-term weight loss outcomes after LAGB were poor compared with other bariatric procedures, but the number of RCT studies for the comparison in these analyses was low: only 2 RCT studies compared RYGB vs LAGB, and 1 RCT compared LAGB vs SG [18, 26]. The mean 1-year %EWL for RYGB, SG, and LAGB was 67.3%, 71.2%, and 40.6%, respectively [25]. Other authors presented a case series analysis of long-term outcomes among 208 patients with LAGB [27]. They showed that LAGB was associated with poor long-term weight loss outcomes and a high failure rate. The %EWL at 5 and 10 years was 30% and 16.9%, respectively, while LAGB failure occurred in 57% of patients, and a higher baseline BMI was the only independently associated factor. In a recent prospective study comparing 5-year results between superobese and non-superobese patients after LAGB, the authors demonstrated that LAGB could lead to long-lasting weight loss after 5 years, but superobese patients had significantly inferior weight loss results than patients with a BMI ≤ 50 [28].
During follow-up visits, 7% of patients had complications related to the introduction of the band system, and all required re-surgery. Band slippage and band migration were the most common complications, which were detected in 3.5% and 1.3% of patients, respectively. Our results support the complications in the existing literature on LAGB, indicating that band slippage is one of the most common late complications, with an incidence frequently below 5% [29], while erosion, as summarized in the results of studies that included estimates at the 5-year follow-up, had an incidence of 0.9–3.1% [13]. We know that long-term LAGB is ineffective and has a high rate of reoperation. The follow-up data, including studies with minimal 10-year follow-up data for LAGB patients, indicated that the median complication rate, reoperation rate, and band removal rate due to insufficient weight loss or complications were 42.7% (5.9–52.9%), 36.5% (7.2–66.1%), and 22.9% (5.4–54.0%), respectively [30]. Another study with a mean follow-up of over 10 years showed that approximately 60% of patients had their bands removed after LAGB, and 30% had another bariatric surgery [31]. There are also results of long-term observations in which only 5.6% of bands were removed during 16 years of follow-up in a cohort of 3227 patients [32]. However, careful analysis of the data showed that 46% of patients in the 10-year follow-up period and 76% of patients in the 15-year follow-up underwent surgical revision with band replacement [32]. Another recent study obtained the best results in young patients with a high BMI, but the results in elderly patients and in people with a low BMI were satisfactory [14]. At the same time, they put forward the idea of using completely reversible LAGB as a first-line method in bariatric surgery, unlike the authors of another analysis [27], who suggested that LAGB may be an option only for patients with a low BMI who do not meet the current criteria for other bariatric surgery techniques and who are not suitable candidates for endoscopic treatment.
There is a limitation to the study that needs to be acknowledged. During the last few years, LAGB has become a less popular procedure than LRYGB and SG. The prevalence of LAGB has declined due to the literature showing weight regain and high late complication and reintervention rates. In this context, a group of over 200 patients who underwent LAGB is relatively large. However, with the low percentage of follow-up patients (less than 50%), the results concerning anthropometric parameters were comparable to a previously published study. Of course, 28 patients at 5-year follow-up is a significant limitation to the study. Its long-term results cannot be extrapolated to a general obese population after LAGB because of a small number of patients.
Conclusions
Our study confirmed the good early results and low effectiveness of laparoscopic adjustable gastric banding in the long-term treatment of pathological obesity. On the other hand, the simplicity and safety of the procedure, the minimal effects of malnutrition, the low number of early complications, and the total reversibility or conversion procedure for any other bariatric surgery are the strengths of laparoscopic adjustable gastric banding for a selected group of patients.
References
WHO, Global Health Observatory data repository, Overweight/ Obesity: http://apps.who.int/gho/data/node.main.A896?lang=en
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, Aminian A, Pothier CE, Kim ES, Nissen SE, Kashyap SR, Investigators STAMPEDE (2014) Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med 370(21):2002–2013
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP (2009) Sledge I (2009) Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 122(3):248–256
Pontiroli AE, Morabito A (2011) Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg 253(3):484–7
Cardoso L, Rodrigues D, Gomes L, Carrilho F (2017) Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab 19(9):1223–1232
Raaijmakers LC, Pouwels S, Thomassen SE, Nienhuijs SW (2017) Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr 71(4):441–449
Deitel M (2003) Overweight and obesity worldwide now estimated to involve 1.7 billion people. Obes Surg 13(3):329–30
O’Brien PE (2010) Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol 25(8):1358–1365
Belachew M, Legrand MJ, Defechereux TH, Burtheret MP, Jacquet N (1994) Laparoscopic adjustable silicone gastric banding in the treatment of morbid obesity. A preliminary report. Surg Endosc 8(11):1354–1356
Pardela M, Wiewióra M, Sitkiewicz T, Wylezol M (2005) The progress in bariatric surgery. J Physiol Pharmacol 56(Suppl 6):35–44
Wylezoł M, Pardela M, Gluck M, Puzio J, Czapla J (2000) Swedish adjustable gastric band (SAGB) implanted laparoscopically in the treatment of morbid obesity-the first experience in Poland. Med Sci Monit 6(3):441–445
Furbetta N, Cervelli R, Furbetta F (2020) Laparoscopic adjustable gastric banding, the past, the present and the future. Ann Transl Med 8(Suppl 1):S4
Furbetta N, Gragnani F, Flauti G, Guidi F, Furbetta F (2019) Laparoscopic adjustable gastric banding on 3566 patients up to 20-year follow-up: long-term results of a standardized technique. Surg Obes Relat Dis 15(3):409–416
Giet L, Baker J, Favretti F, Segato G, Super P, Singhal R, Ashton D (2018) Medium and long-term results of gastric banding: outcomes from a large private clinic in UK. BMC Obes 5:12
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N (2018) IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28(12):3783–3794
Welbourn R, Hollyman M, Kinsman R, Kinsman R, Dixon J, Liem R, Ottosson J, Ramos A, Våge V, Al-Sabah S, Brown W, Cohen R, Walton P, Himpens J (2018) Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg 29(3):782–795
English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM (2018) American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14(3):259–263
English WJ, DeMaria EJ, Hutter MM, Guo Y, Peng S, Luo Y, Wang J (2020) American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 16(4):457–463
Walędziak M, Różańska-Walędziak AM, Kowalewski PK, Kothari SN, Mattar SG, Brethauer SA, Morton JM (2019) Present trends in bariatric surgery in Poland. Wideochir Inne Tech Maloinwazyjne 14(1):86–89
Li L, Yu H, Liang J, Guo Y, Peng S, Luo Y, Wang J (2019) Meta-analysis of the effectiveness of laparoscopic adjustable gastric banding versus laparoscopic sleeve gastrectomy for obesity. Medicine 98(9):e14735
Dogan K, Gadiot RP, Aarts EO, Janik MR, Brągoszewski J, Paśnik K, Bednarczyk G, Wallner G, Matłok M (2016) Effectiveness and safety of sleeve gastrectomy, gastric bypass, and adjustable gastric banding in morbidly obese patients: a multicenter, retrospective, matched cohort study. Obes Surg 25:1110–1118
Golzarand M, Toolabi K, Farid R (2017) The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc 31(11):4331–4345
Michalik M, Lech P, Bobowicz M, Orlowski M, Lehmann A (2011) A 5-year experience with laparoscopic adjustable gastric banding-focus on outcomes, complications, and their management. Obes Surg 21(11):1682–1686
Orłowski M, Janik M, Franczak P, Franczak P, Frask A, Michalik M (2020) Is it possible to improve long-term results of laparoscopic adjustable gastric banding with appropriate patient selection? Wideochir Inn tech Maloinwazyjne 15(1):166–170
Kang JH, Le QA (2017) Effectiveness of bariatric surgical procedures: a systematic review and network meta-analysise of randomized controlled trials. Medicine (Baltimore) 96(46):e8632
Khoraki J, Moraes MG, Neto A, Funk LM, Greenberg JA, Campos GM (2018) Long-term outcomes of laparoscopic adjustable gastric banding. Am J Surg 215(1):97–103
Juodeikis Z, Brimienė V, Brimas G (2019) A prospective study comparing 5-year results between superobese and non-superobese patients after laparoscopic adjustable gastric banding. Wideochir Inne Tech Maloinwazyjne 14(1):79–85
Kodner C, Hartman DR (2014) Complications of adjustable gastric banding surgery for obesity. Am Fam Phys 89(10):813–818
Shen X, Zhang X, Bi J, Yin K (2015) Long-term complications requiring reoperations after laparoscopic adjustable gastric banding: a systematic review. Surg Obes and Relat Dis 11(4):956–964
Froylich D, Abramovich-Segal T, Pascal G, Haskins I, Appel B, Kafri N, Hazzan D (2018) Long-term (over 10 years) retrospective follow-up of laparoscopic adjustable gastric banding. Obes Surg 28(4):976–980
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257(1):87–94
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zurawel, R., Gluck, M., Piecuch, J. et al. Effectiveness and Safety of Adjustable Gastric Banding in Morbidly Obese Patients After 5 Years of Follow-up. Indian J Surg (2021). https://doi.org/10.1007/s12262-021-03174-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-021-03174-6