Abstract
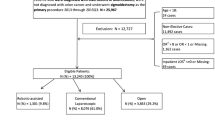
To investigate the influence of surgeon’s experience on outcome among patients undergoing colectomy for benign and malignant diseases. Using medical record folders in this single center retrospective study, we analyzed operative morbidity and mortality in patients undergoing surgery either for colon cancer or diverticulitis between January 1, 2008, and June 30, 2015. Surgeons were divided into three groups: A (surgical experience < 10 years), B (surgical experience 10–20 years), and C (surgical experience > 20 years). Logistic regression analysis was used to assess the relation between experience and outcome. Five hundred twenty-eight colonic resections were performed by group A (12.9%), group B (63.6%), and group C (23.5%), respectively. There were no differences in patient characteristics between the groups. Surgery due to colon cancer was more frequent, and sigmoid colectomy due to diverticulitis was less frequent in group A vs. groups B and C (p < 0.001). Right colectomy was more frequent in group A, whereas patients underwent a higher percentage of sigmoid colectomy in groups B and C (p < 0.001). There was no difference in morbidity, conversion rate, and mortality rate between the groups. Surgeon’s experience was not associated with morbidity and mortality. The results of our study suggest that for colectomies due to both, benign and malignant lesions, years of professional experience are not an important predictor of surgical outcome. However, large bowel resections can also be performed safely by less experienced surgeons without increase in morbidity and mortality.
Similar content being viewed by others
References
Waljee JF, Greenfield LJ, Dimick JB, Birkmeyer JD (2006) Surgeon age and operative mortality in the United States. Ann Surg 244:353–362
Xirasagar S, Lien YC, Lin HC, Lee HC, Liu TC, Tsai J (2008) Procedure volume of gastric cancer resections versus 5-year survival. Eur J Surg Oncol 34:23–29
Chai CY, Chen CH, Lin HW, Lin HC (2010) Association of increasing surgeon age with decreasing in-hospital mortality after coronary artery bypass graft surgery. World J Surg 34:3–9
O’Neill L, Lanska DJ, Hartz A (2000) Surgeon characteristics associated with mortality and morbidity following carotid endarterectomy. Neurology 55:773–781
Prystowsky JB (2005) Are young surgeons competent to perform alimentary tract surgery? Arch Surg 140:495–502
Jackson GR, Owsley C (2003) Visual dysfunction, neurodegenerative diseases, and aging. Neurol Clin 21:709–728
Peisah C, Wilhelm K (2002) The impaired ageing doctor. Intern Med J 32:457–459
Drag LL, Bieliauskas LA, Langenecker SA, Greenfield LJ (2010) Cogntive functioning, retirement status and age: results from the cognitive changes and retirement among senior surgeons study. J Am Coll Surg 211:303–307
Dindo D, Demartines N, Clavien PA (2004) Ann Surg 244:931–937
Flum DR, Dellinger EP (2004) Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg 199:543–551
Watson DI, Baigrie RJ, Jamieson GG (1996) A learning curve for laparoscopic fundoplication: definable, avoidable, or a waste of time? Ann Surg 224:198–203
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW (1997) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 132:41–44
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Kirchhoff P, Dincler S, Buchmann P (2008) A multivariate analysis of potential risk factors for intra- and postoperative complications in 1316 elective laparoscopic colorectal procedures. Ann Surg 248:259–265
Piessen G, Muscari F, Rivkine E, Sbaï-Idrissi MS, Lorimier G, Fingerhut A, Dziri C, Hay JM, FRENCH (Fédération de Recherche EN CHirurgie) (2011) Prevalence of and risk factors for morbidity after elective left colectomy: cancer vs noncomplicated diverticular disease. Arch Surg 146:1149–1155
Ko CY, Chang JT, Chaudhry S, Kominski G (2002) Are high-volume surgeons and hospitals the most important predictors of in-hospital outcome for colon cancer resection? Surgery 132:268–273
Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP, Phelan MA, Henderson WG, Daley J, Khuri SF (2000) Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 43:83–91
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Holmer, C., Sanftleben, A.E., Kreis, M.E. et al. Impact of Surgeon’s Experience on Surgical Outcomes in Colorectal Surgery. Indian J Surg 81, 248–252 (2019). https://doi.org/10.1007/s12262-018-1784-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1784-6