Abstract
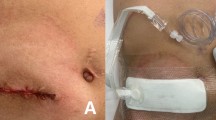
This study aimed to evaluate ostomy closure applications and outcomes and determine the effect of personal differences among surgeons on patient postoperative course. Ninety-eight patients who underwent elective ostomy (ileostomy and colostomy) closure for 8 years at a pediatric surgery training department were investigated. Postoperative complications included superficial surgical site infection (SSI; 9.4 %), organ/cavity infection (1 %), small bowel adhesions (8.2 %), and incisional hernia (1 %). SSI and postoperative complications were not affected by the preoperative antibiotic regimen used. Operation duration, pre- and postoperative antibiotic use durations, postoperative inpatient period, ostomy type, primary diagnosis, performance of abdominal exploration, SSI, and postoperative complications were not significantly different. However, the time of nasogastric (NG) tube withdrawal, time to oral feeding initiation, abdominal closure method used, and preoperative antibiotic regimen were significantly different among different surgeons. We conclude that while surgeons used different preoperative antibiotic regimens and abdominal closure methods and stipulated different times for NG tube withdrawal and oral feeding initiation, the postoperative course and prognosis were unaffected Thus, the pre- and postoperative inpatient period and antibiotic use duration can be decreased in children by procedure standardization using practice guidelines; the procedures can also be performed with a more aesthetic, acceptable incision.
Similar content being viewed by others
References
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 20(4):250–278. doi:10.1086/501620, quiz 279–280
Menzies D, Parker M, Hoare R, Knight A (2001) Small bowel obstruction due to postoperative adhesions: treatment patterns and associated costs in 110 hospital admissions. Ann R Coll Surg Engl 83(1):40–46
Sangkhathat S, Patrapinyokul S, Tadyathikom K (2003) Early enteral feeding after closure of colostomy in pediatric patients. J Pediatr Surg 38(10):1516–1519
Kaiser AM, Israelit S, Klaristenfeld D, Selvindoss P, Vukasin P, Ault G, Beart RW (2008) Morbidity of ostomy takedown. J Gastrointest Surg 12(3):437–441. doi:10.1007/s11605-007-0457-8
Parks SE, Hastings PR (1985) Complications of colostomy closure. Am J Surg 149(5):672–675
Leong G, Wilson J, Charlett A (2006) Duration of operation as a risk factor for surgical site infection: comparison of English and US data. J Hosp Infect 63(3):255–262. doi:10.1016/j.jhin.2006.02.007
Boland E, Hsu A, Brand MI, Saclarides TJ (2007) Hartmann’s colostomy reversal: outcome of patients undergoing surgery with the intention of eliminating fecal diversion. Am Surg 73(7):664–667, discussion 668
Guenaga KF, Matos D, Wille-Jorgensen P (2011) Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev 9, CD001544. doi:10.1002/14651858.CD001544.pub4
Wille-Jorgensen P, Guenaga KF, Matos D, Castro AA (2005) Pre-operative mechanical bowel cleansing or not? An updated meta-analysis. Color Dis 7(4):304–310. doi:10.1111/j.1463-1318.2005.00804.x
Breckler FD, Rescorla FJ, Billmire DF (2010) Wound infection after colostomy closure for imperforate anus in children: utility of preoperative oral antibiotics. J Pediatr Surg 45(7):1509–1513. doi:10.1016/j.jpedsurg.2009.10.054
Verma R, Nelson R (2007) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database of Syst Rev 3. doi:10.1002/14651858.CD004929.pub3
Dinsmore JE, Maxson RT, Johnson DD, Jackson RJ, Wagner CW, Smith SD (1997) Is nasogastric tube decompression necessary after major abdominal surgery in children? J Pediatr Surg 32(7):982–984, discussion 984–985
Vermulst N, Vermeulen J, Hazebroek EJ, Coene PP, van der Harst E (2006) Primary closure of the skin after stoma closure. Management of wound infections is easy without (long-term) complications. Dig Surg 23(4):255–258. doi:10.1159/000095399
Bischoff A, Levitt MA, Lawal TA, Pena A (2010) Colostomy closure: how to avoid complications. Pediatr Surg Int 26(11):1087–1092. doi:10.1007/s00383-010-2690-6
Chandramouli B, Srinivasan K, Jagdish S, Ananthakrishnan N (2004) Morbidity and mortality of colostomy and its closure in children. J Pediatr Surg 39(4):596–599
Kiely EM, Spitz L (1985) Layered versus mass closure of abdominal wounds in infants and children. Br J Surg 72(9):739–740
Ortqvist L, Almstrom M, Ojmyr-Joelsson M, Wigander H, Wahrner A, Wester T (2011) Cosmetic and functional outcome after stoma site skin closure in children. Pediatr Surg Int 27(10):1123–1126. doi:10.1007/s00383-011-2933-1
Lewis SJ, Egger M, Sylvester PA, Thomas S (2001) Early enteral feeding versus “nil by mouth” after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ 323(7316):773–776
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Çavuşoğlu, Y.H., Karaman, A., Afşarlar, Ç.E. et al. Ostomy Closures in Children: Variations in Perioperative Care Do Not Change the Outcome. Indian J Surg 77 (Suppl 3), 1131–1136 (2015). https://doi.org/10.1007/s12262-015-1212-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-015-1212-0