Summary
Human papilloma virus (HPV) is a DNA virus consisting of approximately 8000 base pairs. HPV represents the most common sexually transmitted infection worldwide. Around 200 different genotypes exist. They are distinguished into low- and high-risk genotypes, depending on the risk of such HPV-associated lesions undergoing malignant transformation. The high-risk genotypes include HPV 16 and 18, which are responsible for a variety of human cancers. The most common malignancies that are associated with HPV infection are cervical cancer, oropharyngeal cancer and anal cancer. Screening for HPV precursor lesions in women has led to a drastic reduction in cervical cancer morbidity and mortality in the last 30 years. Unfortunately no such screening tests are available for other HPV-associated malignancies. With the advent of HPV vaccination programs a marked decrease in the prevalence of HPV was reached in vaccinated individuals. However, since these programs were initiated around 2009 the full effect on the incidence of HPV-associated cancers cannot be fully estimated yet.
Similar content being viewed by others
HPV
HPV is a non-enveloped circular double-stranded DNA virus consisting of 8000 base pairs (bp). According to their tissue tropism, HPV is divided into cutaneous and mucosal types. The latter group is further divided into high- and low-risk HPVs depending on their ability to transform normal epithelial cells into premalignant and malignant lesions. Of the approximately 200 different genotypes, 15 are included into the high-risk group (HR-HPV) including HPV genotypes 16, 18, 31, 32, 35, 39 45, 51, 52, 56, 58 and 59 [1].
The HPV genome is divided into three major parts: (1) a non-coding region (upstream regulatory region or URR) which consists mainly of transcription factor binding sites and regulatory genes; (2) an early coding region which consists of 6 genes (E1, E2, E4, E5, E6, E7) that are responsible for viral replication and cell transformation; and (3) a late coding region which consists of L1 and L2 proteins which are capsid proteins that possess the ability of self assemblance to form the virion [1]. A short overview of the connection between different HPV genotypes and human disease is given in Table 1.
HPV and malignant cell transformation
HR-HPV is associated with 90% of cervical and anal carcinomas, 40–60% of vaginal and penile carcinomas and may account for up to 60% of oropharyngeal cancer (OPSCC) depending on the geographic region and sexual preferences [2].
The key elements for the malignant transformation of HPV-infected mucosal cells are the oncogenes E6 and E7 and to a lesser extent E5 [3]. In the following the exact mechanisms that the expression of these genes has on the malignant transformation of human epithelial cells will be summarised.
E6 and E7 proteins were found to be expressed in human cervical carcinoma and are frequently deregulated due to the loss of the viral transcription repressor E2 [3]. A number of crucial cellular checkpoints for cell cycle progression, proliferation and immortalization of the HPV-infected cells are influenced by these viral oncogenes [4].
E7 protein interacts with the tumour suppressor retinoblastoma protein (RB) and inhibits its function [5]. E7 binds to RB via a LXCXE amino acid motif and leads to the initiation of cell cycle progression [6]. Most interestingly is the ability of E7 to bind RB with ubiquitin ligase and therefore lead to proteasomal degradation [7]. Furthermore cellular senescence is blunted by E7 via the CDK4/CDK6 inhibitor p16, which is highly expressed in HPV-associated cancer cells [8, 9].
In healthy cells the uncontrolled proliferation leads to activation of p53, which in turn leads to the activation of apoptosis. However, E6 protein terminates p53 via ubiquitin ligases for proteasomal degradation. Furthermore this oncogene can activate telomerase expression and therefore lead to an immortalization of the infected cells [8].
In addition, the activation of the host immune system is blunted by mechanisms involving the expression of E5, which leads to a decrease in the expression of major histocompatibility class I (MHC I) proteins. Additionally E6 and E7 can inhibit interferon signalling which further abrogates the immune response [10, 11]. A short overview of the effects on cellular level of the different HPV-related proteins is given in Table 2. Overall, the malignant transformation of the host cell is a rare event. However, the genomic instability induced by HR-HPV infection facilitates the accumulation of oncogenic mutations and proliferation of these cells (Fig. 1).
The viral oncogene E7 leads to an inhibition and degradation of the tumour suppressor RB. This leads to the initiation of cell proliferation. In cells with intact p53 this uncontrolled proliferation leads to activation of apoptosis. However in the presence of the HPV E6 protein p53 is inhibited and degraded, which leads to uncontrolled proliferation and instability of the genome
Screening for HPV-associated cancer
Cervical cancer is the fourth most common cancer in women. Nearly 85% of cancers occur in developing countries, where cervical cancer is still the leading cause of female cancer deaths [12, 13]. HR-HPV is responsible for approximately 90% of cervical cancer among women, of these up to 60% are due to infection with HPV genotype 16, genotype 18 accounts for up to 15% [14]. Infection is transmitted via sexual intercourse and skin to skin contact [15].
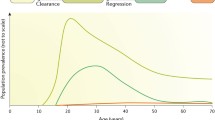
In most women the infection is self-limiting. However, if the infection persists the risk of cancer development, especially for HR-HPV, increases. According to the existing data, the risk of cervical intraepithelial neoplasia (CIN) grade 3, a precursor of cervical cancer, to become invasive cancer is around 30% in a 30 year period [16]. Cervical cancer has been the leading cause of female cancer death in developed countries. However, with the initiation of cytological screening methods, basically the papanicolaou smear, the mortality rate from cervical cancer among women has markedly decreased [17]. Early detection of non-invasive lesions led up to a 35% reduction in the risk of dying from cervical cancer. In a meta-analysis of 24 clinical trials a marked effect of cytological screening on the risk of being diagnosed with invasive cancer (relative risk [RR] 0.38; 95% CI 0.23–0.65) was evident [18].
However, incorporation of HPV DNA testing to detect infection with HR-HPV together with cytological screening was shown to lead to an increased detection rate of high-risk lesions (CIN3) [19, 20]. In 2014 a systematic review on the available literature regarding HPV DNA testing compared to only cytological testing was conducted. In total 6 randomized controlled trials (RCT) with a total of 462,096 women were included. The results showed a reduction in the cancer-specific mortality for the combined testing vs. cytology alone (RR 0.59; 95% CI 0.39–0.91) and a decrease in the incidence of cervical cancer in the second round of screening (RR 0.29; 95% CI 0.11–0.73). However, it has to be stated that the combined testing led to a higher detection rate of CIN2 lesions (RR 1.51; 95% CI 1.21–1.9), especially in patients <30 years of age [29]. Spontaneous remission may occur in 60% of CIN 1 and only 10% progress to CIN3. For CIN2 almost 40% can regress and approximately 20% progress to CIN3 [21, 22]. Therefore an increased rate of CIN2 lesions may lead to an overtreatment of women as the chance of spontaneous remission is high.
According to the German S3 guidelines an organised screening with HPV testing alone or HPV testing + cytology should not be performed on women <30 years of age. In this population the rate of false-positive results regarding CIN2 lesions was up to 20% in 2 RCTs [20].
Besides cervical cancer, no validated screening programs for other HPV-associated cancers exist. For HPV-associated OPSCC, oral fluid may present a promising way of detecting infection with HR-HPV. However, up to now, these methods lack sufficient sensitivity and specificity to be used as reliable screening methods [22].
Prevention of HPV-associated cancer
HPV is the most common sexually transmitted disease. Sexual behaviour also presents the most important risk factor for HPV-associated tumours. The factors include lifetime number of vaginal or any sex partners, oral sex, open mouth kissing and primary or secondary immunodeficiency (e.g. HIV infection) [23]. HPV infection can partly be prevented by the use of barrier methods (e.g. condoms). Nevertheless, as HPV can be transmitted via skin to skin contact, these methods do not offer full protection and their effectiveness is lessened by the number of intercourses [24].
Given the fact that prevention of HPV infection with conventional means was difficult to achieve, high effort was put into the development of anti-HPV vaccines. Currently three HPV vaccines exist: a bivalent vaccine (against HPV 16, 18), a quadrivalent vaccine (HPV 1, 11, 16, 18) and a nonavalent vaccine (HPV 6, 11, 16, 18, 31, 33, 45, 52, 58) [25].
The bivalent vaccine against HPV 16/18 has proven its high efficacy to prevent HPV related CIN in vaccinated women. The vaccine efficacy in preventing CIN1 + CIN2 was 100% at the follow-up of 9.4 years. All vaccinated individuals remained seropositive against HPV 16/18 [26]. Moreover in Scotland the bivalent vaccination led to a marked risk reduction of CIN3 lesions in vaccinated females. The highest effect was seen in women with deprived backgrounds (RR 0.29; 95% CI 0.2–0.43) [27].
Similar results were seen in a Japanese population of 1814 women—the vaccine effectiveness against HPV 16/18 was 95.5% in sexually naïve females. Interestingly, a cross protection against HPV 31, 45 and 52 with a vaccine effectiveness of 71.9% could be observed [28].
In Australia a 90% reduction of genital warts in a vaccinated population was reported over 4 years since the introduction of the quadrivalent vaccine. Interestingly a similar reduction for HPV infection was seen in young heterosexual males, which could point out herd immunity triggered by the vaccination program [29]. Epidemiologic data showed promising results in terms of reduced rates of HPV infection in both females and males. Additionally the prevalence of HPV in a vaccinated US population was significantly reduced (adjusted prevalence rate 0.1; 95% CI 0.1–0.3) since the introduction of the quadrivalent vaccine [30].
The efficacy of the nonavalent vaccination is high, with protection against persistent HPV infection (risk reduction [rr] 96%; 95% CI 94.4–97.2%) and HPV-related high grade cervical disease (rr 96.3%; 95% CI 79.5–99.8%) [25]. However, it has to be pointed out that also in the study populations for the quadrivalent vaccine, with a follow-up of up to 8 years, no case of HPV 6/11/16/18 related CIN has been detected so far [31,32,33].
Furthermore a meta-analysis reported a significant decrease in the infection rate with HPV 16 and 18 in countries with a vaccination coverage of at least 50% (RR 0.32; 95% CI 0.19–0.52). In addition, a reduction of genital warts was seen (RR 0.39; 95% CI 0.22–0.71) and this was also seen in boys under 20 (RR 0.66; 95% CI 0.47–0.91) and in women between 20 and 39 (RR 0.68; 95% CI 0.51–0.89). This indicates that the higher vaccination coverage induces herd immunity. Conversely in a population with less than 50% coverage the reduction in HPV 16 and 18 was only seen in girls <20 [34]. It has to be pointed out that in these populations only female subjects were vaccinated. However, nowadays vaccination of young males is also encouraged.
The total effects on cancer prevention are not yet fully established. As the development of HPV-associated malignancies can take decades from the initiating infection, a decrease in the incidence cannot be elucidated at this time point.
Conclusion
HR-HPV infection is an important risk factor for the development of different cancer types. Effective screening methods do exist for cervical cancer, which is displayed by the marked reduction in the incidence of invasive cancer and a reduction in cervical cancer mortality in recent decades. HPV vaccination has already shown promising effects in preventing persistent HPV infection. However the long-term data for the prevention of HPV-associated cancer are not available yet.
References
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology. 2004;324(1):17–27.
de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664–70.
McLaughlin-Drubin ME, Munger K. The human papillomavirus E7 oncoprotein. Virology. 2009;384(2):335–44.
Cheng S, Schmidt-Grimminger DC, Murant T, Broker TR, Chow LT. Differentiation-dependent up-regulation of the human papillomavirus E7 gene reactivates cellular DNA replication in suprabasal differentiated keratinocytes. Genes Dev. 1995;9(19):2335–49.
Dyson N, Howley PM, Munger K, Harlow E. The human papilloma virus-16 E7 oncoprotein is able to bind to the retinoblastoma gene product. Science. 1989;243(4893):934–7.
DeCaprio JA. Human papillomavirus type 16 E7 perturbs DREAM to promote cellular proliferation and mitotic gene expression. Oncogene. 2014;33(31):4036–8.
Huh K, Zhou X, Hayakawa H, Cho JY, Libermann TA, Jin J, et al. Human papillomavirus type 16 E7 oncoprotein associates with the cullin 2 ubiquitin ligase complex, which contributes to degradation of the retinoblastoma tumor suppressor. J Virol. 2007;81(18):9737–47.
McLaughlin-Drubin ME, Meyers J, Munger K. Cancer associated human papillomaviruses. Curr Opin Virol. 2012;2(4):459–66.
Mesri EA, Feitelson MA, Munger K. Human viral oncogenesis: a cancer hallmarks analysis. Cell Host Microbe. 2014;15(3):266–82.
Roman A, Munger K. The papillomavirus E7 proteins. Virology. 2013;445(1–2):138–68.
Vande Pol SB, Klingelhutz AJ. Papillomavirus E6 oncoproteins. Virology. 2013;445(1–2):115–37.
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24(14):2137–50.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11(11):1048–56.
Mosher WD, Deang LP, Bramlett MD. Community environment and women’s health outcomes: contextual data. Vital Health Stat 23. 2003;23:1–72.
McCredie MR, Sharples KJ, Paul C, Baranyai J, Medley G, Jones RW, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 2008;9(5):425–34.
Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin. 2012;62(5):283–98.
Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev. 2013;2:35.
Naucler P, Ryd W, Tornberg S, Strand A, Wadell G, Elfgren K, et al. Human papillomavirus and Papanicolaou tests to screen for cervical cancer. N Engl J Med. 2007;357(16):1589–97.
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla PP, Del Mistro A, et al. Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol. 2010;11(3):249–57.
Ostor AG. Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol. 1993;12(2):186–92.
Chai RC, Lambie D, Verma M, Punyadeera C. Current trends in the etiology and diagnosis of HPV-related head and neck cancers. Cancer Med. 2015;4(4):596–607.
Pickard RK, Xiao W, Broutian TR, He X, Gillison ML. The prevalence and incidence of oral human papillomavirus infection among young men and women, aged 18–30 years. Sex Transm Dis. 2012;39(7):559–66.
Burchell AN, Winer RL, de Sanjose S, Franco EL. Chapter 6: Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24(Suppl 3):52–61.
Joura EA, Giuliano AR, Iversen OE, Bouchard C, Mao C, Mehlsen J, et al. A 9‑valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med. 2015;372(8):711–23.
Naud PS, Roteli-Martins CM, De Carvalho NS, Teixeira JC, de Borba PC, Sanchez N, et al. Sustained efficacy, immunogenicity, and safety of the HPV-16/18 AS04-adjuvanted vaccine: final analysis of a long-term follow-up study up to 9.4 years post-vaccination. Hum Vaccin Immunother. 2014;10(8):2147–62.
Cameron RL, Kavanagh K, Cameron Watt D, Robertson C, Cuschieri K, Ahmed S, et al. The impact of bivalent HPV vaccine on cervical intraepithelial neoplasia by deprivation in Scotland: reducing the gap. J Epidemiol Community Health. 2017;71(10):954–60.
Kudo R, Yamaguchi M, Sekine M, Adachi S, Ueda Y, Miyagi E, et al. Bivalent human papillomavirus vaccine effectiveness in a Japanese population: high vaccine-type-specific effectiveness and evidence of cross-protection. J Infect Dis. 2019;219(3):382–90.
Ali H, Guy RJ, Wand H, Read TR, Regan DG, Grulich AE, et al. Decline in in-patient treatments of genital warts among young Australians following the national HPV vaccination program. BMC Infect Dis. 2013;13:140.
Dunne EF, Naleway A, Smith N, Crane B, Weinmann S, Braxton J, et al. Reduction in human papillomavirus vaccine type prevalence among young women screened for cervical cancer in an integrated US Healthcare Delivery System in 2007 and 2012–2013. J Infect Dis. 2015;212(12):1970–5.
Iversen OE. The HPV vaccine ten years—what’s the status? Tidsskr Nor Laegeforen. 2017;137(6):430–1.
Nygard M, Saah A, Munk C, Tryggvadottir L, Enerly E, Hortlund M, et al. Evaluation of the long-term anti-human papillomavirus 6 (HPV6), 11, 16, and 18 immune responses generated by the quadrivalent HPV vaccine. Clin Vaccine Immunol. 2015;22(8):943–8.
Villa LL. Overview of the clinical development and results of a quadrivalent HPV (types 6, 11, 16, 18) vaccine. Int J Infect Dis. 2007;11(Suppl 2):S17–S25.
Drolet M, Benard E, Boily MC, Ali H, Baandrup L, Bauer H, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2015;15(5):565–80.
Acknowledgements
Many thanks to Rachel Dale, PhD, for language and grammar review.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Minichsdorfer declares that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Minichsdorfer, C. HPV-associated cancers. memo 12, 352–356 (2019). https://doi.org/10.1007/s12254-019-00551-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-019-00551-6