Abstract
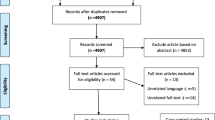
In the management of women diagnosed with endometrial hyperplasia (EH), it is crucial to determine the risk of coexistent cancer. Diabetes mellitus has been recently suggested as a significant risk factor. However, results in this regard are conflicting. Our aim was to assess the association between diabetes mellitus and coexistent cancer in women diagnosed with endometrial hyperplasia. A systematic review and meta-analysis was performed by searching electronic databases from their inception to October 2018 for studies assessing the presence of coexistent cancer after a preoperative diagnosis of endometrial hyperplasia in women stratified for diabetes mellitus. Odds ratio was calculated with 95% confidence interval; a p value <0.05 was considered significant. Twelve retrospective studies with 1579 EH were included. Diabetes mellitus showed significant association with the presence of cancer coexistent with endometrial hyperplasia (OR = 1.96; 95% CI, 1.07–3.60; p = 0.03). Heterogeneity among studies was moderate (I2 = 55%). Funnel plot showed asymmetric distribution of OR values, with the large and accurate studies showing results stronger than small and less accurate one; this finding should exclude a publication bias. In women diagnosed with endometrial hyperplasia, diabetes mellitus is a risk factor for coexistent cancer, and thus may be included in a predictive algorithm for the risk stratification. In women conservatively treated, glycemic control may be required to prevent the risk of progression. Further studies are necessary to confirm the clinical significance of diabetes mellitus in this field.




Similar content being viewed by others
References
Kurman R, Carcangiu M, Herrington C, Young R (2014) World Health Organisation classification of tumors of female reproductive organs, 4th edn. International Agency for Research on Cancer (IARC) Press, Lyon
Sanderson PA, Critchley HOD, Williams ARW, Arends MJ, Saunders PTK (2017) New concepts for an old problem: the diagnosis of endometrial hyperplasia. Hum Reprod Update 23(2):232–254
Travaglino A, Raffone A, Saccone G et al (2018) Endometrial hyperplasia and risk of coexistent cancer: WHO vs EIN criteria. Histopathology.
Baak JP, Mutter GL (2005) EIN and WHO94. J Clin Pathol 58(1):1–6
Ordi J, Bergeron C, Hardisson D, McCluggage WG, Hollema H, Felix A, Soslow RA, Oliva E, Tavassoli FA, Alvarado-Cabrero I, Wells M, Nogales FF (2014) Reproducibility of current classifications of endometrial endometrioid glandular proliferations: further evidence supporting a simplified classification. Histopathology. 64(2):284–292
McCluggage WG (2006) My approach to the interpretation of endometrial biopsies and curettings. J Clin Pathol 59(8):801–812
Travaglino A, Raffone A, Saccone G, Insabato L, Mollo A, de Placido G, Zullo F (2018) Loss of Bcl-2 immunohistochemical expression in endometrial hyperplasia: a specific marker of precancer and novel indication for treatment. A systematic review and meta-analysis. Acta Obstet Gynecol Scand 97:1415–1426
Raffone A, Travaglino A, Saccone G, Mascolo M, Insabato L, Mollo A, de Placido G, Zullo F (2019) PAX2 in endometrial carcinogenesis and in differential diagnosis of endometrial hyperplasia. A systematic review and meta-analysis of diagnostic accuracy. Acta Obstet Gynecol Scand 98(3):287–299
Raffone A, Travaglino A, Saccone G, Campanino MR, Mollo A, de Placido G, Insabato L, Zullo F (2019) Loss of PTEN expression as diagnostic marker of endometrial precancer: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 98(3):275–286
Travaglino A, Raffone A, Saccone G, de Luca C, Mollo A, Mascolo M, de Placido G, Insabato L, Zullo F (2019) Immunohistochemical nuclear expression of β-catenin as a surrogate of CTNNB1 exon 3 mutation in endometrial Cancer. Am J Clin Pathol 151:529–538. https://doi.org/10.1093/ajcp/aqy178
Chen YL, Cheng WF, Lin MC, Huang CY, Hsieh CY, Chen CA (2009) Concurrent endometrial carcinoma in patients with a curettage diagnosis of endometrial hyperplasia. J Formos Med Assoc 108(6):502–507
Chen YL, Wang KL, Chen MY, Yu MH, Wu CH, Ke YM, Chen YJ, Chang YY, Hsu KF, Yen MS (2013) Risk factor analysis of coexisting endometrial carcinoma in patients with endometrial hyperplasia: a retrospective observational study of Taiwanese gynecologic oncology group. J Gynecol Oncol 24(1):14–20
Matsuo K, Ramzan AA, Gualtieri MR, Mhawech-Fauceglia P, Machida H, Moeini A, Dancz CE, Ueda Y, Roman LD (2015) Prediction of concurrent endometrial carcinoma in women with endometrial hyperplasia. Gynecol Oncol 139(2):261–267
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1)
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, QUADAS-2 Group (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Lacey JV Jr, Mutter GL, Nucci MR, Ronnett BM, Ioffe OB, Rush BB, Glass AG, Richesson DA, Chatterjee N, Langholz B, Sherman ME (2008) Risk of subsequent endometrial carcinoma associated with endometrial intraepithelial neoplasia classification of endometrial biopsies. Cancer 113(8):2073–2081
Baak JP, Mutter GL, Robboy S, van Diest PJ, Uyterlinde AM, Ørbo A, Palazzo J, Fiane B, Løvslett K, Burger C, Voorhorst F, Verheijen RH (2005) The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system. Cancer. 103(11):2304–2312
Menke A, Casagrande S, Geiss L, Cowie CC (2015) Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 314(10):1021–1029
Widra EA, Dunton CJ, McHugh M, Palazzo JP (1995 May) Endometrial hyperplasia and the risk of carcinoma. Int J Gynecol Cancer 5(3):233–235
Bilgin T, Ozuysal S, Ozan H, Atakan T (2004) Coexisting endometrial cancer in patients with a preoperative diagnosis of atypical endometrial hyperplasia. J Obstet Gynaecol Res 30(3):205–209
Merisio C, Berretta R, De Ioris A et al (2005) Endometrial cancer in patients with preoperative diagnosis of atypical endometrial hyperplasia. Eur J Obstet Gynecol Reprod Biol 122(1):107–111
Daud S, Jalil SS, Griffin M, Ewies AA (2011 Nov) Endometrial hyperplasia - the dilemma of management remains: a retrospective observational study of 280 women. Eur J Obstet Gynecol Reprod Biol 159(1):172–175
Robbe EJ, van Kuijk SM, de Boed EM et al (2012) Predicting the coexistence of an endometrial adenocarcinoma in the presence of atypical complex hyperplasia: immunohistochemical analysis of endometrial samples. Int J Gynecol Cancer 22(7):1264–1272
Touboul C, Piel B, Koskas M, Gonthier C, Ballester M, Cortez A, Daraï E (2014) Factors predictive of endometrial carcinoma in patients with atypical endometrial hyperplasia on preoperative histology. Anticancer Res 34(10):5671–5676
Zhou L, Meng Z, Wu Y, Zhu H, Wang X (2014) Prediction of endometrial carcinogenesis probability while diagnosed as atypical endometrial hyperplasia: a new risk model based on age, CA199 and CA125 assay. Eur J Obstet Gynecol Reprod Biol 183:5–9
Dolanbay M, Kutuk MS, Uludag S, Bulut A, Ozgun M, Ozcelik B, Serin I (2015) Concurrent endometrial carcinoma in hysterectomy specimens in patients with histopathological diagnosis of endometrial hyperplasia in curettage specimens. Ginekol Pol 86(10):753–758
Kadirogullari P, Atalay CR, Ozdemir O, Sari ME (2015) Prevalence of co-existing endometrial carcinoma in patients with preoperative diagnosis of endometrial hyperplasia. J Clin Diagn Res 9(10):QC10–QC14
Ferenczy A, Gelfand MM, Tzipris F (1983) The cytodynamics of endometrial hyperplasia and carcinoma. A review. Ann Pathol 3(3):189–201
Travaglino A, Raffone A, Saccone G, Mollo A, de Placido G, Mascolo M, Insabato L, Zullo F (2019) Complexity of glandular architecture should be reconsidered in the classification and management of endometrial hyperplasia. APMIS. 127:427–434. https://doi.org/10.1111/apm.12945
Raffone A, Travaglino A, Saccone G, Insabato L, Mollo A, de Placido G, Zullo F (2019) Endometrial hyperplasia and progression to cancer: which classification system stratifies the risk better? A systematic review and meta-analysis. Arch Gynecol Obstet 299:1233–1242. https://doi.org/10.1007/s00404-019-05103-1
Travaglino A, Raffone A, Saccone G, et al (2019) PTEN immunohistochemistry in endometrial hyperplasia: which are the optimal criteria for the diagnosis of precancer? APMIS. https://doi.org/10.1111/apm.12938
Raglan O, Kalliala I, Markozannes G, Cividini S, Gunter MJ, Nautiyal J, Gabra H, Paraskevaidis E, Martin-Hirsch P, Tsilidis KK, Kyrgiou M (2018) Risk factors for endometrial Cancer: an umbrella review of the literature. Int J Cancer. https://doi.org/10.1002/ijc.31961
Fader AN, Arriba LN, Frasure HE, von Gruenigen VE (2009) Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol 114(1):121–127
Pollak M (2008) Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer 8:915–928
Sasaki LMP, Andrade KRC, Figueiredo ACMG, Wanderley MDS, Pereira MG (2018) Factors associated with malignancy in Hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol 25(5):777–785
Management of Endometrial Hyperplasia Green-top Guideline No. 67 RCOG/BSGE joint guideline | February 2016
Zhang Q, Qi G, Kanis MJ, Dong R, Cui B, Yang X, Kong B (2017 May 3) Comparison among fertility-sparing therapies for well differentiated early-stage endometrial carcinoma and complex atypical hyperplasia. Oncotarget. 8(34):57642–57653
Giampaolino P, Di Spiezio Sardo A, Mollo A et al (2018) Hysteroscopic endometrial focal resection followed by Levonorgestrel intrauterine device insertion as a fertility-sparing treatment of atypical endometrial hyperplasia and early endometrial Cancer: a retrospective study. J Minim Invasive Gynecol
Raffone A, Travaglino A, Saccone G, Alviggi C, Mascolo M, de Placido G, Insabato L, Mollo A, Zullo F (2019) Management of women with atypical polypoid adenomyoma of the uterus: a quantitative systematic review. Acta Obstet Gynecol Scand. https://doi.org/10.1111/aogs.13553
Meireles CG, Pereira SA, Valadares LP, Rêgo DF, Simeoni LA, Guerra ENS, Lofrano-Porto A (2017) Effects of metformin on endometrial cancer: systematic review and meta-analysis. Gynecol Oncol 147(1):167–180
Raffone A, Travaglino A, Saccone G, Mollo A, de Placido G, Insabato L, Zullo F (2019) Should progesterone and estrogens receptors be assessed for predicting the response to conservative treatment of endometrial hyperplasia and cancer? A systematic review and meta-analysis. Acta Obstet Gynecol Scand. https://doi.org/10.1111/aogs.13586
Travaglino A, Raffone A, Saccone G, Insabato L, Mollo A, de Placido G, Zullo F (2018) PTEN as a predictive marker of response to conservative treatment in endometrial hyperplasia and early endometrial cancer. A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 231:104–110
Travaglino A, Raffone A, Saccone G, Insabato L, Mollo A, de Placido G, Zullo F (2019) Immunohistochemical predictive markers of response to conservative treatment of endometrial hyperplasia and early endometrial cancer: a systematic review. Acta Obstet Gynecol Scand. https://doi.org/10.1111/aogs.13587
Raffone A, Travaglino A, Saccone G, Di Maio A, Mollo A, Mascolo M, De Rosa R, De Placido G, Insabato L, Zullo F, (2019) Diabetes mellitus and responsiveness of endometrial hyperplasia and early endometrial cancer to conservative treatment. Gynecological Endocrinology:1-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raffone, A., Travaglino, A., Saccone, G. et al. Diabetes Mellitus Is Associated with Occult Cancer in Endometrial Hyperplasia. Pathol. Oncol. Res. 26, 1377–1384 (2020). https://doi.org/10.1007/s12253-019-00684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-019-00684-3