Abstract
Purpose
The sterilization process for medical devices is an important step due to microbiological quality requirements of polymeric products. Irradiation and ethylene oxide sterilizations, traditional techniques, may compromise safety and efficacy of medical devices due to oxidation/alkylation or due to the presence of residues in polymeric materials. Alternatively, reactive Ion etching (RIE) and inductively coupled plasma (ICP) may be used for this purpose; however, the compatibility of polymeric materials with these processes and their lethality must be addressed.
Methods
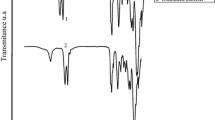
We assessed herein chemical and biological modifications in polymeric materials after an RIE and ICP sterilization process, using photoacoustic Fourier transform infrared spectroscopy (FTIR-PAS), scanning electron microscopy with energy dispersive X-ray spectroscopy (SEM/EDS), surface profilometry analysis (SPA), and in vitro agar diffusion cytotoxicity. In addition, a factorial design was adopted to study lethality in PVC catheters, evaluating the influence of sterilization mode (RIE or ICP), radio frequency power (from 100 to 300 W), hydrogen peroxide concentration (from 0 to 20%), and internal lumen diameter of PVC catheters (from 1 to 7 mm) in D-values.
Results
RIE and ICP sterilization using a mixture of O2 and H2O2 (80 and 20%, respectively) have caused chemical modifications in all polymers, however, without increasing in vitro cytotoxicity. Based on factorial design results, we proposed mathematical models to predict the D-values (time to kill 90%––or 1 log reduction––of microbial load) as a function of H2O2 concentration and internal lumen diameter of catheters.
Conclusions
Quality by design approach allow one to develop a rational sterilization process considering the required time for sterilization, concentration of H2O2, and the internal lumen diameter of catheters.






Similar content being viewed by others
References
Padoveze MC, Del Monte MCC. Coord. esterilização de artigos em unidades de saúde. 2nd ed. São Paulo: Associação Paulista de Estudos e Controle de Infecção Hospitalar; 2003. 156p
Oliveira DC, Pinto TJA. Influência da concentração gasosa sobre a efetividade esterilizante da mistura oxyfume 2002® (óxido de etileno diluído em hcfcs 22 e 124). Braz J Pharm Sci. 2001;37:203–9.
Oliveira DC, Pinto TJA. Sterilizing effectivity study of different ethylene oxide gaseous mixtures using cfcs and hcfcs (oxyfume 12® and oxyfume 2002®). PDA J Pharm Sci Technol. 2002;56:242–7.
Clough RL, Shalaby SW Irradiation of polymers: fundamentals and technological applications. Washington: American Chemical Society, 1996. 433p. (ACS Symposium Series, 620) (Developed from a Symposium Sponsored by the Division of Polymer Chemistry, INC., at the 208th. National Meeting of the American Chemical Society, Washington, DC, August 21–25, 1994).
Pruitt L, Ranganathan R. Effect of sterilization on the structure and fatigue resistance of medical grade uhmwpe. Mater Sci Eng C Biomim Supramol Syst. 1995;3:91–3.
Shen F, Yu Y, Mckellop H. Potential errors in FTIR measurement of oxidation in ultrahigh molecular weight polyethylene implants. J Biomed Mater Res. 1999;48:203–10.
Yue-e F, Jun J, Chaoxiong M. Study of radiation-induced grafting of 2-hydroxyethyl methacrylate to chloroprene rubber membrane. Radiat Phys Chem. 1999;54:159–63.
Moreira AJ, Mansano RD, Pinto TJA, Ruas R, Zambon LS, Silva MS, et al. Sterilization by oxygen plasma. Appl Surf Sci. 2004;235:151–5.
Miao H, Jierong C. Inactivation of Escherichia coli and properties of medical poly(vinyl chloride) in remote-oxygen plasma. Appl Surf Sci. 2009;255:5690–7.
Yardimci O, Setlow P. Plasma sterilization: opportunities and microbial assessment strategies in medical device manufacturing. IEEE Trans Plasma Sci. 2010;38:973–81.
Moisan M, Barbeau J, Morteau S, Pelletier J, Tabrizian M, Yahia LH. Low-temperature sterilization using gas plasmas: a review of the experiments and an analysis of the inactivation mechanisms. Int J Pharm. 2001;226:1–21.
Moisan M, Barbeau J, Crevier MC, Pelletier J, Philip N, Saoudi B. Plasma sterilization: methods and mechanisms. Pure Appl Chem. 2002;74:349–58.
Levif P, Séguin J, Moisan M, Soum-Glaude A, Barbeau J. Packaging materials for plasma sterilization with the flowing afterglow of an n2–o2 discharge: damage assessment and inactivation efficiency of enclosed bacterial spores. J Phys D Appl Phys. 2011;44:1–13.
Daseco JA, Pabeliña KG, Siringan MAT, Ramos HJ. Comparative study on the use of different metal electrodes in low-pressure glow discharge plasma sterilization. Plasma Med. 2014;4:1–10.
Raguse M, Fiebrandt M, Denis B, Stapelmann K, Eichenberger P, Driks A, et al. Understanding of the importance of the spore coat structure and pigmentationin the Bacillus subtilis spore resistance to low-pressure plasma sterilization. J Phys D Appl Phys. 2016;49:1–16.
Adler S, Scherrer M, Daschner FD. Costs of low-temperature plasma sterilization compared with other sterilization methods. J Hosp Infect. 1998;40:25–134.
Rathore AS, Winkle H. Quality by design for biopharmaceuticals. Nat Biotechnol. 2009;27:26–34.
Misar SN, Ansari MH, Derle DV, Bhalerao KR. Quality by design: a paradigm for industry. Int J Pharm Sci Rev Res. 2014;13:67–74.
Yu LX, Amidon G, Khan MA, Hoag SW, Polli J, Raju GK, et al. Understanding pharmaceutical quality by design. AAPS J. 2014;16:771–83.
Lourenço FR, Francisco FL, Ferreira MRS, Pinto TJA, Löbenberg R, Bou-chacra N. Design space approach for preservative system optimization of an anti-aging eye fluid emulsion. J Pharm Pharm Sci. 2015;18:551–61.
Peres DD, Ariede MB, Cândido TM, Almeida TS, Lourenço FR, Consiglieri VO, et al. Quality by design (QbD), process analytical technology (PAT) and design of exeperiments applied to the development of multifunctional sunscreens. Drug Dev Ind Pharm. 2016;
Lerouge S, Guignot C, Tabrizian M, Ferrier D, Yagoubi N, Yahia LH. Plasma-based sterilization: effect on surface and bulk properties, and hydrolytic stability of reprocessed polyurethane electrophysiology catheters. J Biomed Mater Res. 2000;52:774–82.
Lerouge S, Tabrizian M, Wertheimer MR, Marchand R, Yahia LH. Safety of plasma-based sterilization: surface modifications of polymeric medical devices induced by Sterrad® and Plazlytetm processes. Biomed Mater Eng. 2002;12:3–13.
Goldman M, Pruitt L. Comparison of the effects of gamma radiation and low temperature peroxide gas plasma sterilization on the molecular structure, fatigue resistance, and wear behaviour of UHMWPE. J Biomed Mater Res. 1998;40:378–84.
Gogolewski S, Mainil-Varlet P, Dillon JG. Sterility, mechanical properties, and molecular stability of polylactide internal –fixation devices treated with low-temperature plasmas. J Biomed Mater Res. 1996;32:227–35.
Canevarolo SV Jr. Ciência dos polímeros: um texto básico para tecnólogos e engenheiros. Artliber: São Paulo; 2004. 183p.
Klapperich C, Pruitt L, Komvopoulos K. Chemical and biological characteristics of low-temperature plasma treated ultra-high molecular weight polyethylene for biomedical applications. J Mater Sci Mater Med. 2001;12:549–56.
Sidouni FZ, Nurdin N, Chabrecek P, Lohmann D, Vogt J, Xanthopoulos N, et al. Surface properties of a specifically modified high-grade medical polyurethane. Surf Sci. 2001;491:355–69.
Kaczmarek H, Kowalonek J, Szalla A, Sionkowska A. Surface modification of thin polymeric films by air-plasma or UV irradiation. Surf Sci. 2002;507(510):883–8.
Aouinti M, Bertrand P, Poncin-Epaillard F. Characterization of polypropylene surface treated in a CO2 plasma. Plasmas Polym. 2003;8:225–36.
Borcia G, Anderson CA, Brown NMD. The surface oxidation of selected polymers using an atmospheric pressure air dielectric barrier discharge. Appl Surf Sci. 2004;221(Part I):203–14.
Borcia G, Anderson CA, Brown NMD. The surface oxidation of selected polymers using an atmospheric pressure air dielectric barrier discharge. Appl Surf Sci. 2004;225(Part II):2186–97.
Tajima S, Komvopoulos K. Effect of ion energy fluence on the topography and wettability of low-density polyethylene exposed to inductively coupled argon plasma. J Phys D Appl Phys. 2006;39:1084–94.
Svorcik V, Kolarova K, Slepicka P, Mackova A, Novotna M, Hnatowicz V. Modification of surface properties of high and low density polyethylene by ar plasma discharge. Polym Degrad Stab. 2006;91:1219–25.
Cahen D. Photoacoustic in life sciences. J Biochem Biophys Methods. 1980;3:293–310.
Ciurczak EW. Aplicações da espectroscopia por infravermelho fotoacústica. Pharm Technol: Edição Brasileira. 1999;3:11–2.
Kawano Y. Espectroscopia vibracional de absorção no infravermelho/espectroscopia fotoacústica no infravermelho. In: Canevarolo Jr SV, editor. Coord. Técnicas de Caracterização de Polímeros. Artliber: São Paulo; 2004. 448p.
Yang CQ, Bresee RR, Fateley WG. Near-surface analysis and depth profiling by FT-IR photoacoustic spectroscopy. Appl Spectrosc. 1987;41:889–96.
Sowa MG, Dahlia F, Eysel HH, Mantsch HH. FT-IR PAS depth profiling investigation of polyethylene surface sulfonation. J Mol Struct. 1996;379:77–85.
Yang H, Yaraj JJ, Sakhamuri S. Characterization of edible coatings and microorganisms on food surfaces using Fourier transform infrared photoacoustic spectroscopy. Appl Spectrosc. 2001;55:571–82.
Wang J, Pan CJ, Huang N, Sun H, Yang P, Leng YX, et al. Surface characterization and blood compatibility of poly(ethylene tetraphthalate) modified by plasma surface grafting. Surf Coat Technol. 2005;196:307–11.
Clode PL. Charge contrast imaging of biomaterials in a variable pressure scanning electron microscope. J Struct Biol. 2006;155:505–11.
Strobel M, Walzak MJ, Hill JM, Lin A, Karbashewski E, Lyons CS. A comparison of gas-phase methods of modifying polymer surfaces. J Adhes Sci Technol. 1995;9(9):365–83. https://doi.org/10.1163/156856195X00554.
Vinogradov I, Lunk A. Spectrocopic diagnostics of DBD in ar/fluorocarbon mixtures—correlation between plasma parameters and properties of deposited polymer films. Plasma Process Polym. 2005;2:201–8.
Zreiqat H, Evans P, Howlett CR. Effect of surface chemical modification of bioceramic on phenotype of human bone-derived cells. J Biomed Mater Res. 1999;44:389–96.
Gorna K, Gogolewski S. Molecular stability, mechanical properties, surface characteristics and sterility of biodegradable polyurethanes treated with low-temperature plasma. Polym Degrad Stab. 2003;79:475–85.
Pinto TJA, Azevedo JC, Cruz AS. Comparative study of epithelial and fibroblastic cell lines as an alternative cytotoxicity test to the draize method. J AOAC Int. 2000;83:665–8.
Rogero SO, Malmonge SM, Lugão AB, Ikeda TI, Miyamaru LL, Cruz AS. Biocompatibility study of polymeric biomaterials. Artif Organs. 2003;27:424–7.
Pinto TJA, Ikeda TI, Miyamaru LL, Santa MC, Santos BRP, Cruz AS. Cosmetic safety: proposal for the replacement of in vivo (draize) by in vitro test. Open Toxicol J. 2009;3:1–7.
Mccarthy SJ, Gordon FM, Mitchell N, Gunatillake PA, Heath G, Brandwood A, et al. In vivo degradation of polyurethanes: Transmission-FTIR microscopic characterization of polyurethanes sectioned by cryomicrotomy. Biomaterials. 1997;18:1387–409.
Hury S, Vidal DR, Desor F, Pelletier J, Lagarde T. A parametric study of the destruction efficiency of bacillus spores in low pressure oxygen-based plasmas. Lett Appl Microbiol. 1998;26(26):417–21. https://doi.org/10.1046/j.1472-765X.1998.00365.x.
Soloshenko LA, Tsiolko VV, Khomich VA, Bazhenov VY, Ryabtsev AV, Shehedrin AI, et al. Features of sterilization using low pressure DC discharge hydrogen peroxide plasma. IEEE Trans Plasma Sci. 2002;30:1440–4.
Akitsu T, Ohkawa H, Tsuji M, Kimura H, Kogoma M. Plasma sterilization using glow discharge at atmospheric pressure. Surf Coat Technol. 2005;193:29–34.
Lerouge S, Wertheimer MR, Marchand R, Tabrizian M, Yahia LH. Effect of gas composition on spore mortality during low-pressure plasma sterilization. J Biomed Mater Res. 2000;51:128–35.
De Nardo I, Alberti R, Cigada A, Yahia L, Tanzi MC, Fare S. Shape memory polymer foams for cerebral aneurysm reparation: effects of plasma sterilization on physical properties and cytocompatibility. Acta Biomater. 2009;5:1508–18.
Oliveira DC, Kikuchi IS, Moreira AJ, Silva JMF, Mansano RD, Pinto TJA. Evaluation of microbicidal activity of oxygen-containing plasmas using biological monitors with different lumen calibers. Acta Farm Bonaer. 2012;31:257–64.
Hayashi N, Guan W, Tsutsui S, Tomari T, Hanada Y. Sterilization of medical equipment using radicals produced by oxygen/water vapor RF plasma. Jpn J Appl Phys. 2006;45:8358–63.
Khomich VA, Soloshenko IA, Tsiolko VV, Mikhno IL (1998) Investigation of principal factors of the sterilization by plasma DC glow discharge. In: International Congress on Plasma Physics, Prague, 1998. Proceedings. Prague 22c. 2745–2748.
Rutala WA, Gergen MF, Weber DJ. Comparative evaluation of the sporicidal activity of new low-temperature sterilization technologies: ethylene oxide, 2 plasma sterilization systems, and liquid peracetic acid. Am J Infect Control. 1998;26:393–8.
Lerouge S, Wertheimer MR, Yahia LH. Plasma sterilization: a review of parameters, mechanisms and limitations. Plasmas Polym. 2001;6:175–88.
Boudam MK, Moisan M, Saoudi B, Popovici C, Gherardi N, Massines F. Bacterial spore inactivation by atmospheric-pressure plasmas in the presence or absence of UV photons as obtained with the same gas mixture. J Phys D Appl Phys. 2006;39:3494–507.
Acknowledgements
We thank Nelson Ordonez, Alexandre Camponucci, José Antônio R Porto, Elisio José de Lima, Áurea Silveira da Cruz, Fernanda de Sá Teixeira, Cleide Amaral, Aline Morais de Oliveira, and Fernando Adas Pereira Vitalli. Jim Hesson of AcademicEnglishSolutions.com revised the English.
Funding
This work was supported by CNPq (Brazil).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declared that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Oliveira, D.C., Calixto, L.A., Fukuda, I.M. et al. Compatibility of Polyvinyl Chloride (PVC) Medical Devices and Other Polymeric Materials with Reactive Ion Etching (RIE) and Inductively Couple Plasma (ICP) Sterilization Using a Quality by Design (QbD) Approach. J Pharm Innov 13, 110–120 (2018). https://doi.org/10.1007/s12247-018-9309-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-018-9309-1