Abstract
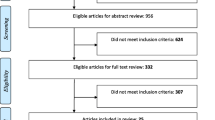
Recurrent acute otitis media (rAOM) poses a significant challenge in children aged 1 to 6 years, characterized by frequent and treatment-resistant ear infections. While existing studies predominantly focus on alterations in the nasopharyngeal microbiome associated with rAOM, our research explores the understudied association with the gut microbiome. In this cross-sectional observational prospective study, we enrolled 35 children aged 1 to 6 years during the 2021/2022 cold season. The test group comprised children with rAOM (n = 16), and the control group consisted of generally healthy children (n = 19). Samples (stool and nasopharyngeal swabs) were collected in late spring to ensure an antibiotic-free period. Detailed metadata was gathered through a questionnaire examining factors potentially influencing microbiota. Microbiota composition was assessed through amplicon sequencing of the V3–V4 region of the 16S rRNA gene. Our findings revealed limited alterations in gut microbiota composition among children with rAOM compared to healthy controls. Six bacterial taxa (Veillonella, Lachnospiraceae, Ruminococcaceae, Lachnospiraceae, Bacteroides and Blautia) were differentially represented with weak statistical significance. However, several bacterial taxa displayed correlations with multiple consecutive infections, with Turicibacter showing the most significant association. Additionally, day care centre attendance emerged as a potent gut microbiota modifier, independent of rAOM. Although our study identified limited differences in gut microbiota composition between children with rAOM and healthy controls, the observed correlations between the number of infections and specific bacterial taxa suggest a potential link between rAOM and the gut microbiota, warranting further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent otitis media (rAOM) is a prevalent condition characterized by repetitive middle ear infections, predominantly affecting young children aged between 6 months and 3 years, although it can also occur in older children. While uncomplicated otitis media is typically managed by paediatricians through medical history assessment and clinical examination, children with rAOM often require referral to otolaryngologists for further evaluation and potential surgical intervention (Goycoolea et al. 1991). The impact of rAOM extends beyond the affected individuals, imposing a significant socioeconomic burden on families. The consequences include healthcare costs, absenteeism, productivity loss, developmental delays in speech and language and reduced overall quality of life (Greenberg et al. 2003; Brouwer et al. 2005; Kujala et al. 2017).
Several well-known risk factors associated with rAOM include age (between 6 months and 2 years), genetic factors, passive smoking, allergies, craniofacial anomalies, immunodeficiency and snoring (Assiri et al. 2023). Implementing preventive measures, such as vaccinations, good hygiene practices and timely treatment of respiratory infections, can aid in reducing the risk and severity of rAOM (Dagan et al. 2016).
Probiotics have emerged as a potential intervention for rAOM, with some promising results reported in a review of 17 randomized controlled trials evaluating their efficacy in children with rAOM. However, caution is advised in interpreting these findings, as subgroup analyses highlighted the need for further research in this area (Scott et al. 2019). Dysbiosis, characterized by disruptions in gut microbiota composition and diversity, has been linked to immune dysregulation, potentially rendering individuals more susceptible to infections, including ear infections (Ihekweazu and Versalovic 2018; Willers and Viemann 2021; Zama et al. 2022).
In an observational study by Thapa et al. in 2020, the microbiota of children aged 1–6 undergoing classic otolaryngology operative procedures such as adenotonsillectomy and grommet insertion was analysed. They obtained nasopharyngeal and rectal swabs of children while under general anaesthesia. The study highlighted increase in Haemophilus spp. in nasopharyngeal microbiome of children who received antibiotics, but it lacked healthy controls (Thapa et al. 2020).
Only one study to date has investigated the gut microbiota in otitis media. The study analysed the MiBioGen consortium dataset, comparing 11 samples of acute suppurative otitis media and 16 samples of chronic suppurative otitis media against the remaining database using multiple logistic regression (Wang et al. 2023).
In our study, we aim to explore the potential association between gut microbiota alterations and rAOM in children. By investigating the composition and diversity of the gut microbiota in children with rAOM compared to healthy controls, we seek to deepen our understanding of different factors contributing to recurrent ear infections.
Methods
Sample collection
This cross-sectional observational prospective study included a total of 35 children aged between 1 and 6 years. The test group comprised children within the same age range who met the criteria for recurrent acute otitis media (rAOM). The control group consisted of healthy children without a history of otitis media within the last year and without associated chronic diseases. Recruitment of participants took place in collaboration with regional primary level paediatricians during the cold season of 2021/2022. For the test group, stool and nasopharyngeal swab samples were collected in late spring to ensure an antibiotic-free period. Control group stool samples were collected from healthy volunteers during routine check-ups. In total, 16 stool samples and 19 nasopharyngeal swabs were obtained from the test group, and 19 stool samples were collected from the control group. Additionally, detailed questionnaires were administered to the parents to gather metadata on factors that could potentially influence the microbiota composition (Supplementary file 1).
The study was approved by the ethical committee of Celje general hospital (27/KS/2022–1).
Amplicon metagenomic sequencing
Total DNA was isolated from the collected samples using the QIAGEN mini kit. DNA concentrations were determined using the Quant-iT PicoGreen dsDNA Assay (Thermo Fisher Scientific, USA), and all samples were normalized to a concentration of 5 ng/µl. Libraries were prepared following the 16S Metagenomic Sequencing Library Preparation guide (Illumina, USA), targeting the V3–V4 hypervariable region of the 16S rRNA gene with broad-range primers 341F (5′–CCT ACG GGN GGC WGC AG–3′) and 805R (5′–GAC TAC HVG GGT ATC TAA TCC–3′) (Klindworth et al. 2013). Paired-end sequencing (2 × 300 bp) was performed on the MiSeq (Illumina, USA).
Data processing involved quality filtering of reads and construction of zero radius operational taxonomic units (ZOTUs) using the UNOISE3 pipeline implemented in USEARCH v.11.0.667 (Edgar 2010; Edgar et al. 2011) with default settings and the addition of -fastq-minlen 400 (fastq_filter command). Taxonomy was inferred using the RDP reference database v.18.
Results and discussion
Faecal and nasopharyngeal bacterial community characteristics
Amplicon sequencing of the V3–V4 variable region of the 16S rRNA gene resulted in an average depth of 24,069.62 reads per sample, yielding a total of 905 distinct ZOTUs. The detected bacterial taxa encompassed 10 bacterial phyla. The faecal microbiota was predominantly composed of Firmicutes, Bacteroidetes and Actinobacteria. In contrast, the nasopharyngeal microbiota exhibited a dominance of Proteobacteria, particularly the genera Moraxella and Haemophilus (Fig. 1a). Certain nasopharyngeal swab samples exhibited a high relative abundance of unclassified taxa at the phylum level, highlighting a limited understanding and the lack of comprehensive databases pertaining to nasopharyngeal microbiota.
Faecal and nasopharyngeal bacterial community characteristics. The figure illustrates the characteristics of the faecal and nasopharyngeal bacterial communities. The data is presented separately for three compared groups: faecal microbiota in the test group (green), faecal microbiota in the control group (red) and nasopharyngeal microbiota in the test group (blue). a Relative abundance of bacterial phyla: this panel shows the relative abundance of bacterial phyla that are present at a relative abundance greater than 1% in each sample. b Alpha diversity analysis: this panel presents the results of the alpha diversity analysis, including the Chao index (a measure of community richness) and the Shannon evenness index (a measure of community evenness). c Venn diagram of shared ZOTUs: this diagram illustrates the overlap of ZOTUs among the three compared groups
The richness of the nasopharyngeal microbiota was comparatively lower, with a median of approximately 100 ZOTUs per sample, contrasting with the > 250 ZOTUs observed in the faecal microbiota (Fig. 1b, Chao index). Furthermore, the nasopharyngeal microbiota exhibited significantly lower evenness compared to the faecal microbiota (Fig. 1b, Shannon evenness index). Specifically, the nasopharyngeal microbiota was frequently dominated by the genera Moraxella, Haemophilus and Streptococcus, which were also the most prevalent in the nasopharyngeal samples (prevalence 100.0%, 89.5% and 73.7% for Moraxella, Haemophilus and Streptococcus, respectively). This observation aligns with previous studies employing both metagenomic approaches (Nogues et al. 2020) and culture-based detection methods (Ngo et al. 2016).
In our study, the number of shared representatives between the faecal and nasopharyngeal microbiota was limited to 12 ZOTUs, and the number of shared representatives did not significantly differ between the test and control groups (Fisher exact test, p = 0.475; Fig. 1c). These included multiple representatives from genera Streptococcus (n = 6), Veillonella (n = 2), and a single representative from Corinebacteriaceae, Haemophilus, Granulicatella and Gemella. The mechanism of direct microbial translocation from the nasopharynx to the gut remains poorly understood, despite various established routes within the oral-gut axis, such as enteral, haematogenous and migration via immune cells (Tan et al. 2023). Although evidence regarding the successful colonization of the gut by oral microbiota is conflicting, heightened concentrations of oral microbes have been observed in several gastrointestinal disorders, including gastritis, inflammatory bowel disease, colorectal cancer and various chronic illnesses (Schmidt et al. 2019; Kitamoto et al. 2020). Recent investigations into the interplay between microbiota and COVID-19 have significantly advanced this field of research, notably by elucidating microbial networks between throat and gut microbiota (Xu et al. 2021). Studies have also highlighted disparities in the shared nasopharynx-gut microbiota between COVID-19 patients and healthy individuals (Mancabelli et al. 2023). However, it is worth noting that the study by Mancabelli et al. focused on adult patients and reported distinct shared microbiota patterns compared to our findings. Notably, no prior studies investigating nasopharynx-gut shared microbiota in paediatric populations were found.
Gut microbiota composition in children with rAOM shows limited alteration compared to healthy controls
The gut microbiota community structure did not exhibit a significant difference between the test and control groups (PERMANOVA, p = 0.210; AMOVA, p = 0.842). Additionally, there was no discernible variation in richness and diversity between the compared groups of samples (community richness, p = 0.373; Shannon index, p = 0.894).
Upon conducting a population-level analysis, we identified six bacterial taxa that demonstrated weak statistical significance in their differential representation between the test and control groups. Specifically, Veillonella (ZOTU113) and Lachnospiraceae (ZOTU122) were decreased in the test group compared to the control group, whereas Ruminococcaceae (ZOTU192), Lachnospiraceae (ZOTU289), Bacteroides (ZOTU213) and Blautia (ZOTU197) were increased (Fig. 2a).
Gut microbiota characteristics of rAOM patients. The figure displays the results of a LEfSe test, highlighting the differentially abundant bacterial taxa between the test and control groups. The taxa that showed significant differences are represented by their corresponding linear discriminant analysis (LDA) scores. Negative LDA values (shown in red) indicate taxa that were decreased in the test group compared to the healthy controls, while positive LDA values (shown in blue) indicate taxa that were increased in the test group, and b Pearson’s correlation between bacterial taxa and number of infections
Wang et al. analysed the MiBioGen consortium dataset, comparing 11 samples of acute suppurative otitis media and 16 samples of chronic suppurative otitis media against the remaining database using multiple logistic regression. In MiBioGen consortium set, the authors identified a significant reduction in the Ruminococcaceae family in otitis media, which differs from our study’s findings, where increase was observed in case group and showed positive correlation to a number of infections (Fig. 2b). However, they did report a decrease in Lachnospiraceae in acute suppurative otitis media, which partially aligns with our observations (Vacca et al. 2020).
In our study, we observed weak correlations between the abundance of certain bacterial taxa and the number of infections recorded in the previous year (Fig. 2b). Among these correlations, the most significant ones were positive associations with Turicibacter (ZOTU159) and Ruminococcaceae (ZOTU192).
Ruminococcaceae is a diverse family of commensal bacteria, and further investigation is required to discuss the biological significance of the observed increase in relative abundance in our dataset. Turicibacter is a member of the commensal gut microbiota; however, previous studies have reported its increased abundance in Helicobacter pylori infection (Kienesberger et al. 2016) and rheumatoid arthritis (Chen et al. 2016). It has also been found to be increased in mice with depleted CD8 + T cells (Presley et al. 2010) and isolated from the blood culture of an acute appendicitis patient (Bosshard et al. 2002). Nonetheless, the underlying mechanisms of involvement of Turicibacter in immune responses have not yet been discovered. It is important to note that while these associations have been observed, the specific role of Turicibacter in immune response and its implications in infection remain to be elucidated.
Host-associated features show limited correlation with faecal bacterial community structure
In total, we tested 16 features for their association with the composition of the faecal microbiota. Among these, we found that visiting kindergarten, as opposed to staying at home, was the only feature significantly associated with the bacterial community, explaining 6.9% of the interindividual variation (permutational multivariate analysis of variance (PERMANOVA) using Bray–Curtis distances, p = 0.006; Table 1). Visiting day care facilities was primarily linked to higher bacterial diversity compared to home care, as indicated by the (Shannon index, p = 0.022).
Interestingly, there is a scarcity of studies investigating differences in gut microbiota between children in day care facilities and home care. The only comprehensive study with well-defined groups of children reported findings which agree with our results (Amir et al. 2022). Specifically, children in day care facilities exhibited higher microbiota diversity. Additionally, they found that gut microbiota composition of day care children was more similar to that of adults compared to children in home care (Amir et al. 2022). In contrast, study by Gerben et al. reported no significant differences between children in day care and home care (Hermes et al. 2020). However, it is important to note that in this study, the follow-up period after children entered day care was only 4 weeks. This short duration is likely insufficient to observe significant changes in the gut microbiota.
We acknowledge that the low sample size was a major limitation of this study, particularly given the rapid changes in the microbiota of children under 4 years of age and the potential impact of external factors such as antibiotic therapy on community characteristics.
In conclusion, our study found limited differences in gut microbiota composition between children with rAOM and healthy controls. Interestingly, we observed a correlation between experiencing multiple consecutive infections and a higher relative abundance of Turicibacter in the gut. This genus has previously been reported to increase in various infection-associated conditions. Furthermore, regardless of health status, our findings confirmed previous research indicating that children in day care have higher gut microbiota diversity compared to those in home care.
Data availability
Amplicon sequencing data is available in NCBI SRA archive under BioProject accession number PRJNA1014361.
References
Amir A, Erez-Granat O, Braun T, Sosnovski K, Hadar R, BenShoshan M, Heiman S, Abbas-Egbariya H, Glick Saar E, Efroni G, Haberman Y (2022) Gut microbiome development in early childhood is affected by day care attendance. NPJ Biofilms Microbiomes 8:2. https://doi.org/10.1038/s41522-021-00265-w
Assiri K, Hudise J, Obeid A (2023) Risk factors for chronic and recurrent otitis media in children: a review article. Indian J Otolaryngol Head Neck Surg. https://doi.org/10.1007/s12070-023-04256-5
Bosshard PP, Zbinden R, Altwegg M (2002) Turicibacter sanguinis gen. nov., sp. nov., a novel anaerobic, Gram-positive bacterium. Int J Syst Evol Microbiol 52:1263–1266. https://doi.org/10.1099/00207713-52-4-1263
Brouwer CNM, Rovers MM, Maillé AR, Veenhoven RH, Grobbee DE, Sanders EAM, Schilder AGM (2005) The impact of recurrent acute otitis media on the quality of life of children and their caregivers. Clin Otolaryngol 30:258–265. https://doi.org/10.1111/j.1365-2273.2005.00995.x
Chen J, Wright K, Davis JM, Jeraldo P, Marietta EV, Murray J, Nelson H, Matteson EL, Taneja V (2016) An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Medicine 8:43. https://doi.org/10.1186/s13073-016-0299-7
Dagan R, Pelton S, Bakaletz L, Cohen R (2016) Prevention of early episodes of otitis media by pneumococcal vaccines might reduce progression to complex disease. Lancet Infect Dis 16:480–492. https://doi.org/10.1016/S1473-3099(15)00549-6
Edgar RC (2010) Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26:2460–2461. https://doi.org/10.1093/bioinformatics/btq461
Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R (2011) UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 27:2194–2200. https://doi.org/10.1093/bioinformatics/btr381
Goycoolea MV, Hueb MM, Ruah C (1991) Otitis media: the pathogenesis approach. Definitions and terminology. Otolaryngol Clin North Am 24:757–761
Greenberg D, Bilenko N, Liss Z, Shagan T, Zamir O, Dagan R (2003) The burden of acute otitis media on the patient and the family. Eur J Pediatr 162:576–581. https://doi.org/10.1007/s00431-003-1260-5
Hermes GDA, Eckermann HA, de Vos WM, de Weerth C (2020) Does entry to center-based childcare affect gut microbial colonization in young infants? Sci Rep 10:10235. https://doi.org/10.1038/s41598-020-66404-z
Ihekweazu FD, Versalovic J (2018) Development of the pediatric gut microbiome: impact on health and disease. Am J Med Sci 356:413–423. https://doi.org/10.1016/j.amjms.2018.08.005
Kienesberger S, Cox LM, Livanos A, Zhang X-S, Chung J, Perez-Perez GI, Gorkiewicz G, Zechner EL, Blaser MJ (2016) Gastric Helicobacter pylori infection affects local and distant microbial populations and host responses. Cell Rep 14:1395–1407. https://doi.org/10.1016/j.celrep.2016.01.017
Kitamoto S, Nagao-Kitamoto H, Hein R, Schmidt TM, Kamada N (2020) The bacterial connection between the oral cavity and the gut diseases. J Dent Res 99:1021–1029. https://doi.org/10.1177/0022034520924633
Klindworth A, Pruesse E, Schweer T, Peplies J, Quast C, Horn M, Glockner FO (2013) Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res 41:e1. https://doi.org/10.1093/nar/gks808
Kujala T, Alho O-P, Kristo A, Uhari M, Renko M, Pokka T, Koivunen P (2017) Recurrent acute otitis media detracts from health-related quality of life. J Laryngol Otol 131:128–137. https://doi.org/10.1017/S0022215116009944
Mancabelli L, Taurino G, Ticinesi A, Ciociola T, Vacondio F, Milani C, Fontana F, Lugli GA, Tarracchini C, Alessandri G, Viappiani A, Bianchi M, Nouvenne A, Chetta AA, Turroni F, Meschi T, Mor M, Bussolati O, Ventura M (2023) Disentangling the interactions between nasopharyngeal and gut microbiome and their involvement in the modulation of COVID-19 infection. Microbiology Spectrum 11:e02194-e2223. https://doi.org/10.1128/spectrum.02194-23
Ngo CC, Massa HM, Thornton RB, Cripps AW (2016) Predominant bacteria detected from the middle ear fluid of children experiencing otitis media: a systematic review. PLoS ONE 11:e0150949. https://doi.org/10.1371/journal.pone.0150949
Nogues JC, Pérez-Losada M, Preciado D (2020) Review of otitis media microbiome studies: what do they tell us? Laryngoscope Investig Otolaryngol 5:936–940. https://doi.org/10.1002/lio2.460
Presley LL, Wei B, Braun J, Borneman J (2010) Bacteria associated with immunoregulatory cells in mice. Appl Environ Microbiol 76:936–941. https://doi.org/10.1128/AEM.01561-09
Schmidt TS, Hayward MR, Coelho LP, Li SS, Costea PI, Voigt AY, Wirbel J, Maistrenko OM, Alves RJ, Bergsten E, de Beaufort C, Sobhani I, Heintz-Buschart A, Sunagawa S, Zeller G, Wilmes P, Bork P (2019) Extensive transmission of microbes along the gastrointestinal tract. eLife 8:e42693. https://doi.org/10.7554/eLife.42693
Scott AM, Clark J, Julien B, Islam F, Roos K, Grimwood K, Little P, Del Mar CB (2019) Probiotics for preventing acute otitis media in children. Cochrane Database Syst Rev 6:CD012941. https://doi.org/10.1002/14651858.CD012941.pub2
Tan X, Wang Y, Gong T (2023) The interplay between oral microbiota, gut microbiota and systematic diseases. J Oral Microbiol 15:2213112. https://doi.org/10.1080/20002297.2023.2213112
Thapa S, Runge JK, Venkatachalam A, Denne C, Luna RA, Anon JB (2020) The nasopharyngeal and gut microbiota in children in a pediatric otolaryngology practice. Pediatr Infect Dis J 39:e226. https://doi.org/10.1097/INF.0000000000002703
Vacca M, Celano G, Calabrese FM, Portincasa P, Gobbetti M, De Angelis M (2020) The controversial role of human gut lachnospiraceae. Microorganisms 8:573. https://doi.org/10.3390/microorganisms8040573
Wang Q, He L, Tan H, Huang G, Liu J (2023) Causal relationship between gut microbiota and otitis media: a two-sample Mendelian randomized study. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-023-08102-w
Willers M, Viemann D (2021) Role of the gut microbiota in airway immunity and host defense against respiratory infections. Biol Chem 402:1481–1491. https://doi.org/10.1515/hsz-2021-0281
Xu R, Lu R, Zhang T, Wu Q, Cai W, Han X, Wan Z, Jin X, Zhang Z, Zhang C (2021) Temporal association between human upper respiratory and gut bacterial microbiomes during the course of COVID-19 in adults. Commun Biol 4:1–11. https://doi.org/10.1038/s42003-021-01796-w
Zama D, Totaro C, Biscardi L, Rocca A, Turroni S, Brigidi P, Lanari M (2022) The relationship between gut microbiota and respiratory tract infections in childhood: a narrative review. Nutrients 14:2992. https://doi.org/10.3390/nu14142992
Funding
ARIS SF Infrastructure core activity.
Author information
Authors and Affiliations
Contributions
AF played a pivotal role in the study’s preparation and organization, overseeing the recruitment of participants and conducting the collection of samples and data from case participants. Furthermore, AF actively engaged in result discussions and contributed significantly to the manuscript’s preparation. MR also made substantial contributions to the study’s initial planning and organization and the recruitment of control participants. MR was actively involved in discussions regarding the study’s findings and participated in the preparation of the manuscript. AM performed 16S amplicon sequencing and conducted sequence data analysis. Additionally, AM prepared the statistical analysis and visualizations for the publication and contributed to the discussion of the results and writing of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Florjan, A., Rupnik, M. & Mahnic, A. Gut microbiota composition in recurrent acute otitis media: a cross-sectional observational study. Folia Microbiol (2024). https://doi.org/10.1007/s12223-024-01174-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12223-024-01174-z