Abstract
The Delta variant is one of the alarming variants of the SARS-CoV-2 virus that have been immensely detrimental and a significant cause of the prolonged pandemic (B.1.617.2). During the SARS-CoV-2 pandemic from December 2020 to October 2021, the Delta variant showed global dominance, and afterwards, the Omicron variant showed global dominance. Delta shows high infectivity rate which accounted for nearly 70% of the cases after December 2020. This review discusses the additional attributes that make the Delta variant so infectious and transmissible. The study also focuses on the significant mutations, namely the L452R and T478K present on the receptor-binding domain of spike (S)-glycoprotein, which confers specific alterations to the Delta variant. Considerably, we have also highlighted other notable factors such as the immune escape, infectivity and re-infectivity, vaccine escape, Ro number, S-glycoprotein stability, cleavage pattern, and its binding affinity with the host cell receptor protein. We have also emphasized clinical manifestations, symptomatology, morbidity, and mortality for the Delta variant compared with other significant SARS-CoV-2 variants. This review will help the researchers to get an elucidative view of the Delta variant to adopt some practical strategies to minimize the escalating spread of the SARS-CoV-2 Delta variant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The world has been facing a pandemic since early 2020 named COVID-19. The principal causative agent behind this pandemic is the SARS-CoV-2 virus. Like other RNA viruses, SARS-CoV-2 has also encountered many alterations in its transmissibility and infectivity, causing severe threats to the world population (Chakraborty et al. 2020; CDC 2021). By examining the pattern of infection since 2020, the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), the USA, and the European Centre for Disease Prevention (ECDC) classified the emerging SARS-CoV-2 variants into two essential categories, namely variant of concern (VOC) and variant of interest (VOI). The VOCs are causing typical threats to human life by altering several clinical manifestations of the disease, and they are much more virulent and transmissible. On the other hand, the VOIs are emerging due to amino acid replacements that alter several viral characteristics (Campbell et al. 2021; Gómez et al. 2021).
The Delta (B.1.617.2) variant was first identified in Maharashtra, India, in late 2020. According to several published medical reports, this variant is responsible for about 70% of cases in the Indian subcontinent as of May 2, 2021 (Cherian et al. 2021; Chakraborty et al. 2021b; Kunal et al. 2021). Based on massive transmission, the CDC designated this variant to the VOC category from the VOI category. The Delta variant was reported in 50 other countries within a very short tenure. By August 2021, a total of 163 countries worldwide were affected by this variant. The timeline diagram depicts a critical series of events from the first detection of the Delta variant, naming, and transmission (Fig. 1). This variant comprises 7 to 8 mutations in the spike trimeric protein complex and several characteristic mutations in ORF (1a, 1b, 3a, 7a, 8), nucleocapsid (N) protein, and membrane (M) protein (Table 1) (Farinholt et al. 2021). The mutations in the viral genome of the Delta variant account for many distinct characteristics. This variant also had an altered receptor-binding domain (RBD) conformation accounting for its strong affinity with the human ACE receptor, enhancing cleavage efficiency of the transmembrane serine protease 2 (TMPRSS2). Consequently, it demonstrates powerful and efficient viral entry by evading the membrane of the host cells (Hatmal et al. 2020; Ogawa et al. 2020). The mutations in the viral genome of this variant have exerted alterations in the antigenic properties, questioning the efficacy of the available vaccines (Zhang et al. 2021). Some of the mutations in the RBD domain of the Delta variant include P681R, D614G, T19R, T478K, G142D, L452R, R158G, D950N, and Δ156–157 (Chakraborty et al. 2021a; CDC 2021). The invasion of the ACE2 receptor of the host cell is highly dependent on the conformation of the RBD. Thus, scientists have stated that the mutations in the RBD region, namely T478K and L452R, increase the transmission rate and infectivity rate of the Delta variant (Baral et al. 2021; Chakraborty et al. 2021c).
As per WHO’s reports, out of the several VOCs, the Delta variant is the “fastest and fittest” strain that has emerged to date. It significantly impacts the transmissibility rate, which is twice that of the primitive strain isolated from Wuhan and 40–60% than the Alpha variant. The symptoms caused due to the infection of the variant are more or less similar to the other variants. Still, in some extreme cases, the disease results in hearing disability, gastrointestinal (GI) tract infections, and problems related to blood clotting (Shiehzadegan et al. 2021).
Therefore, this review is primarily focused on the leading state of the distribution of the SARS-CoV-2 Delta variant, its viral load, the cleavage pattern, binding affinity, and stability of the spike protein. Subsequently, we have highlighted the Delta variant's infectivity, re-infectivity, immune, and vaccine escape ability. Our crucial interpretations of the mutation-specific viral variant (B.1.617.2) might help and act as a practical approach for further research and development against this COVID-19 pandemic.
Distribution of Delta variant
The Delta variant has been transmitted worldwide and might be one of the potential causative agents behind the detrimental second wave in India (Vaidyanathan 2021; Yadav et al. 2021). After initial detection in India, it quickly acquired a greater prevalence in the whole country until May 2021 (Campbell et al. 2021; Del Rio et al. 2021). The Delta variant reported a higher number of cases from the UK between February to May 2021 (Kunal et al. 2021). This variant was also responsible for a series of new infections in the USA. The first case was reported in February 2021. The Delta attack was detrimental in places with low vaccination coverage, for example, the Southeastern parts of the USA. Due to a very high vaccination coverage in the UK, the Delta variant infected people, but the severity was fewer and very limited of the subjects required hospitalization (Del Rio et al. 2021). The massive outbreak caused by the Delta variant was very rapid compared to the other variants that emerged from Brazil, South Africa, and Italy.
Remarkably, the Delta variant is currently distributed throughout the globe, including the USA, Europe, Latin America, South America, South Africa, different Asian countries, and Australia (Fig. 2). Previous variants were less harmful than the Delta variant (Shu and McCauley 2017). The Delta variant has been detected in more than 80 countries worldwide, and presently another similar lineage with greater virulence called Delta plus has been reported in Maharashtra, India (Press Information Bureau 2021). Delta plus variant contains additional mutation (K417N) in S-protein compared to the Delta variant (Kannan et al. 2021). The prevalence of Delta variant throughout the world and the submitted sequences of Delta variant as country-wise distributions are shown in Table 2. Furthermore, the continent-wise sequence count in the 7-day rolling average of the Delta variant is also represented in Fig. 3. Subsequently, the continent-wise sequence frequency of the B.1.617.2 lineage in a 7-day rolling average is shown in Fig. 4.
The figure shows the distribution of Delta variants in different countries. The figure illustrates the Delta variant distribution throughout the globe, such as the USA, Europe, Latin America, South America, South Africa, different Asian countries, and Australia. The Delta variant was first found in India and spread throughout the world. The figure was developed by the Nextstrain server (Nextstrain 2021)
The figure depicts continent-wise sequence counts of the Delta variant. The figure represents the 7-day rolling average of sequence counts (continent-wise). The figure was developed by the CoV-lineages server (O'Toole 2021)
The figure illustrates the continent-wise frequency of sequences of the B.1.617.2 lineage. The figure represents the seven-day rolling average. The figure was developed by the CoV -lineages server (O'Toole 2021)
Basic Ro number and viral load
The basic reproduction number (Ro) is the average number of infections transmitted by an infected human being in a completely new population without pre-exposure to vaccines and therapeutics (Katul et al. 2020). The Delta variant has a much higher Ro value than the primitive strain. The Ro value for the Delta variant is 5.08, whereas the wild strain has a value of 2.79 (Liu and Rocklöv 2021). The infections by the Delta variant elucidated that this variant has a more significant viral load and Ro number, contributing to its extraordinary transmission and virulence supremacy (Mlcochova et al. 2021; Ong et al. 2021). A high Ro value also indicates a more excellent coverage of vaccines to combat the ongoing pandemic. The vaccine coverage rate should be increased to 60–70% compared to the Wuhan strain. According to the equation q = 1–1/ Ro, Ro value above 5 needs a more excellent coverage of vaccines (approximately 80%) to combat the disease provided the vaccine administered is 100% efficient (Abu-Raddad et al. 2021). This Ro number may even be higher in the case of the Delta variant because, at the time when this value was estimated, most of the countries imposed lockdown. The vaccine coverage rate should be nearly 90% (Liu and Rocklöv 2021). Recently, a hypothesis was provided by Professor Martin Hibberd, London School of Medicine, on Ro value and stated that the Ro value for a variant is nearly 6 or 7 (Burki 2021). The several mutations in the genome of the Delta variant are mainly responsible for its higher viral loads.
Cleavage pattern, binding affinity, and stability of the spike protein in Delta variant
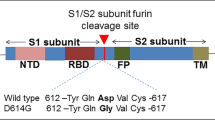
In recent days, the Delta variant has been dominating the pandemic. Most of the reported cases confirm the presence of the Delta variant of the SARS-CoV-2 virus. A more significant number of mutations in the spike glycoprotein also play a vital role in viral transmissibility, infectivity, antigenicity, etc. The L425R, D614G, and T478K mutation in the RBD of the spike proteins in the carboxy-terminal of the S1 domain increases the Delta variant’s transmissibility. These mutations also alter some critical parameters regarding the ACE2-binding capability. It brings a conformational change in the spike protein affecting its binding with the human ACE2 receptor. The extreme pathogenicity and transmissibility also depends on the cleavage efficiency. All the B.1.617 variant sublineages, including Delta, possess an additional mutation in the 618th position proximal to the furin cleavage site. It has been noted that the P618R strongly enhances the cleavage by the furin (Peacock et al. 2021). Due to the E484K mutation in the viral genome of the Delta variant, the RBD conformation gets altered. It remains in the “open-up” state, increasing the immune-evading capacity of this deadly virus. This “open-up” conformation also enhances more viruses to bind with the host ACE2 receptors (Gobeil et al. 2021).
Infectivity, re-infectivity by the Delta variant
One of the most alarming variants responsible for the massive outbreak during the pandemic was the Delta variant due to its infectivity and re-infectivity. Due to several mutations in the viral genome, the virus developed many significant features regarding the epidemiological characteristics compared to the Wuhan strain. The infection rate were higher compared to other variants of SARS-CoV-2. It was noted that the Delta variant demonstrated increased infection in every continent. The continent-wise estimated absolute number of cases of Delta variants is shown in Fig. 5. Due to this enhanced fitness, this variant raises the question about the efficiency of vaccines and other therapeutics. They can escape the immune system even in the presence of antibodies (Walensky et al. 2021). In several cases, several patients noted re-infection by the Delta variant. It has been pointed out that the health workers were re-infected by the Delta variant, though the patient was previously infected by the Alpha variant (Shastri et al. 2021). Since the Delta variant shares many common mutations with the other VOC, the question of re-infection cannot be ignored. A notable predominant mutation in all the variants is D614G, which enhances the transmissibility of all the significant variants of SARS-CoV-2 (Volz et al. 2021). Salehi-Vaziri et al. reported three cases from Iran where the re-infected subjects confirmed the presence of D614G mutation in the viral genome (Salehi-Vaziri et al. 2021). As this mutation is present in the Delta variant, the chances of re-infection persist.
Continent-wise estimate of the absolute number of cases of Delta variants. A Asia, B Europe, C Africa, D North America, E South America. The CoV-spectrum server developed the figure. Data were obtained from the GISAID server, which was analyzed through the web application (Elbe and Buckland‐Merrett 2017)
Moreover, the other mutations present in the variant also contribute to the re-infection of the individuals. Recent studies also proved that the Delta variant could evade the host body despite antibodies developed from prior infections or elicited by the administration of the vaccines (Mlcochova et al. 2021; Planas et al. 2021). This, in turn, raises the question of re-infectivity by the Delta variant.
Clinical manifestations, symptomatology, morbidity, and mortality of Delta variant
The Delta variant spread 50% faster than Alpha, which was 50% more contagious than the Wuhan strain of SARS-CoV-2 throughout the world. Additionally, the Delta plus mutant variant is also a cause for concern. As we know, the specific mutation in position K417N affects the spike protein, resulting in the virus infecting more cells, which is the critical target for the mRNA and other vaccine types (Katella 2021). The major clinical manifestations are high fever, headache, fatigue, dry cough, runny nose, sore throat, persistent chest pain, and shortness of breath by the infection of the Delta variant. Simultaneously, patients also suffered conjunctivitis, diarrhea, muscle or joint pain, vomiting, and loss of appetite for mild-to-severe infection cases (Menni et al. 2022; Wang et al. 2021). The chance of unvaccinated individuals contracting the disease was much higher for infection by the Delta variant. The CDC data showed that unvaccinated Americans died 11 times higher than the rate of fully vaccinated individuals after the Delta variant became dominant (Dyer 2021). Delta variant has a higher transmission and infection rate, followed by the Omicron variant compared to all other known SARS-CoV-2 variants. In terms of clinical severity, the Delta variant appears to cause significantly more severe disease than the Omicron variant (Wrenn et al. 2022). The combination of both variants caused high surges of COVID-19 symptomatic infection and more death cases (Mohapatra et al. 2022).
Delta variant mutations
The Delta variant emerged as one of the most virulent strains due to its combination of the mutations until July 2021 (Elbe and Buckland‐Merrett 2017; Singanayagam et al. 2020). This variant includes seven significant mutations in the spike trimeric protein complex (Fig. 6A). Out of the several significant mutations present in the genome of the Delta variant, the L452R and T478K mutations in the RBD region of the S-glycoprotein part of the viral genome contribute to its high infectivity rate (Fig. 6D). The 3D structural model of SARS-CoV-2 S-glycoprotein has shown significant mutational changes in the Delta variant (Fig. 6). Since the RBD part of the S-glycoprotein is responsible for interacting with the host ACE2 receptor, the mutations in the RBD will play a significant role in providing the essential characteristics of the variant from the epidemiological point of view. These two mutations are also responsible for altering the structural conformation of the Delta variant, which makes it susceptible to escaping the immune system. The residues located in the interface between 438 to 508 amino acid positions are potential target sites for the antibodies. Hence, mutations in these residues will alter the binding affinity with the antibodies and the ACE2 receptor (Baral et al. 2021). Chemmama et al. and Beck et al. highlighted that rearranging the G496 residue establishes a powerful hydrogen bond. The L452R alters the structural flexibility by reorienting the β sheets and demonstrates the interaction between R454 and D467 by forming a salt bridge. It makes the L452R mutant strain a “Variant of Concern (VOC)” by the WHO and CDC, USA (Beck et al. 2008; Chemmama et al. 2012; McCallum et al. 2021). Notably, it also enhances many structural changes in the Delta variant, making it more contagious than the other variants. These mutations alter the arrangements of the β sheets, the antibody-binding ability, the ACE2 receptor–binding affinity, and the destruction and weakening of several hydrogen bonds in the Delta variant (Baral et al. 2021).
Schematic diagram and 3D surface structural model shows different significant mutations position in the S-glycoprotein of Delta variant of SARS-CoV-2. A Schematic diagram of significant mutations of Delta variant in S-protein. B Mutations of Delta variant S-protein surface structure in front view. C Mutations of Delta variant S-protein surface structure 90° axial rotated view. D Mutations of Delta variant S-protein surface structure 90° crosswise turned view
L452R and T478K: two significant mutations in Delta variant
Recent studies show that the L452R mutation is present in many of the recently emerged SARS-CoV-2 variants. Besides, iota, epsilon, and kappa, this mutation is also present in the Delta variant. The mutation resides very close to the interface of the RBD by which it interacts with the host ACE2 receptor (Fig. 6D). The location of the mutation enhances the attachment of more viruses to the receptors and co-receptors. It also contributes to the several characteristics that increases the viral fitness, such as pathogenicity, transmissibility, infectivity, immune escape, and other factors. Studies also show that this L452R is a natural positive selection and has emerged evolutionarily. As this mutation is favored by nature, it contributes to the virulent characteristics of this virus.
A notable example is the Delta variant, a significant damaging strain for the entire population of SARS-CoV-2 variants (Tchesnokova et al. 2021). The MD simulation study performed by Antony et al. revealed that the L452R mutation creates a robust electrostatic interaction of the viral S-glycoprotein with the ACE2 receptor, enhancing the stability of the protein. This interaction alters the conformation of the spike protein, making it difficult for the antibodies to interact, thus increasing the chances of infectivity (Antony and Vijayan 2021).
The T478K is also a very alarming mutation and is responsible for various structural changes in the Delta variant. T478K disrupts the salt bridge between the L31 of the host ACE2 receptor and the E484 of the viral spike protein. T478K also alters the RBD conformation resulting in the “open up” state, which favors the strong binding of the viral spike protein with the ACE2 receptor and leads to escape from the immune system (Gobeil et al. 2021). Interestingly, both of these two mutations reside in the RBD of the S-glycoprotein (Cherian et al. 2021). Moreover, the T478 site is an important position for the interaction of the antibodies, and mutation at this position hinders the binding of the antibodies leading to vaccine escape. Thus, it can be concluded that T478K may be a potential factor contributing to the vaccine escape by the Delta variant. T478K mutation also contributes to enhanced viral fitness of the variants (e.g., Delta, kappa) where these mutations are present compared to the isolated strain from Wuhan (Yi et al. 2020).
Delta variant and other significant SARS-CoV-2 variants
In late 2020, the emergence of SARS-CoV-2 variants increased the risk to global public health and encouraged the need to characterize the significant mutant variants specifically. It was noted that the Delta variant reached almost 90% of all viral sequences submitted on GISAID by October 2021 and had a high global prevalence out of 11 variants of SARS-CoV-2 (Chakraborty et al. 2022a). In the Delta variant, the important mutations have been observed in the RBD regions that can alter the receptor-binding interface’s structural configuration and the binding affinity with the ACE2 protein (Chakraborty et al. 2022b). The Alpha variant was first reported in the UK during September/October 2020 and circulated in several countries. This virus has caused substantial differences in severity, transmissibility, and re-infection possibility. The variant was observed with important mutations in spike protein that also differ from the Delta variant. Specific mutations are also crucially responsible for SARS-CoV-2 variants for antibody, immune, and partial vaccine escape (Chakraborty et al. 2022c). The Beta variant was first documented in May 2020 in South Africa. Studies suggested that mutations in the spike protein (E484K, K417N, and Δ242-244) of the Beta variant might permit it to escape the immune response, even in individuals having current COVID-19 vaccinations (Duong 2021).
Another significant SARS-CoV-2 variant is Omicron which holds maximum important mutations in the RBD regions (32 in coding sequence) in respect to all other variants, causing a higher potential for transmission (Kumar et al. 2022). During the SARS-CoV-2 pandemic from December 2020 to October 2021, the Delta variant showed global dominance, and afterward, the Omicron variant showed global dominance. The researcher also concluded that the Omicron variant rapidly evolved and substituted the Delta variant as the dominant strain (Wang et al. 2021; Bhattacharya et al. 2022). In Omicron, the mutations P681H, N679K, N501Y, T478K, and N655Y also overlay with the other SARS-CoV-2 variants (Gamma, Alpha, Beta, and Delta). It is also noted that the mutations in the NTD (K150 T/Q/R/E, and N148S) and RBD (V445E and K444 Q/R/N) might be the main factor for antibody escape mechanism (Bhattacharya et al. 2022; Weisblum et al. 2020). Furthermore, a unique type of recombinant variant of Delta and Omicron was also observed as “Deltacron” (Wang and Gao 2022). This special variant is designated as XD variant (AY.4/BA.1). It is considered a recombinant lineage from two VOCs, namely the Omicron BA.1 variant and Delta (AY.4) variant. The XD variant encompasses the genomic elements (ORF1a and ORF1b) obtained from the Delta variant, whereas the spike protein part is acquired from the Omicron BA.1 variant. On the other hand, another recombinant “XE” variant is also created from the recombinant genomic elements of two Omicron variants (Omicron BA.2 variant and Omicron BA.1). Likewise, the recombinant XF variant also developed from the diverse recombinant genomic aspects of the two variants. The first part of the genome comprises the Delta variant (NSP1 to NSP3), and the rest is from the Omicron BA.1 variant (Chakraborty et al. 2022d). However, the emergence of these recombinant lineages of Omicron and Delta is not too threatening. However, it needs more research to formulate reasonable control and prevention strategies to stop the recent and future pandemics.
Immune escape by Delta variant
The CD4+ and CD8+ T lymphocytes are responsible for providing immunity in case of the SARS-CoV-2 infection. They are also accountable for inflecting the disease’s severity on any variant’s attack (Le Bert et al. 2020; Moderbacher et al. 2020; Rao et al. 2020). The mutations in the viral genome of the Delta variant are the principal cause of the escape from the immune system. This variant can evade the immune system despite the presence of antibodies. Several structure alterations result in the difference in the receptor-binding surface to interact with the human ACE2 receptor and the antibodies elicited by vaccines or prior infection. Due to high structural flexibility, it becomes difficult for the antibodies to bind, imparting the property of “immune escape”(Baral et al. 2021). These mutations bring some conformational changes in the virus RBD and NTD region.
Moreover, these mutations sometimes change the epitopes of the spike protein, hindering the interaction of the antibodies. Besides, these nonsynonymous spike mutations also bring some changes in the structural conformation of the S1 and S2 domains, which plays a vital role in attaching the virus to the host cell and may be responsible for antibody neutralization (Finkelstein et al. 2021; Plante et al. 2021). The L452R and T478K are the two predominant mutations responsible for the immune invasion capacity of the Delta variant. Some in vitro studies also revealed that the mutation at the 478 positions reduces antibody neutralization (Liu et al. 2021).
Vaccines escape by Delta variant
COVID-19 vaccines are one of the powerful weapons that helped to combat the current pandemic. COVID-19 vaccines were developed very quickly. The world has not seen such quick development of the vaccine. Several types of vaccines were developed, such as mRNA, DNA, recombinant, and peptide (Chakraborty et al. 2021d, e) by different companies from time to time. Using these vaccines, the vaccination program was initiated by several countries. At the same time, vaccine escape phenomena were noted for the different variants (Chakraborty et al. 2022c, e).
The Delta variant was responsible for the massive infection surge in recent months. The currently designed vaccines have proven to protect against this variant, but several facts also imply the vaccine escape property of this variant. This variant neutralizes the antibodies by altering the spike protein conformation enabling it to evade the host (Planas et al. 2021). According to the study conducted by Baral et al., the Delta variant has several structural features which make them superior in escaping the immune system. Compared to the other strains, the Delta variant has a different interaction between the RBD and the antibody receptor, making it fit to evade the immune system. Besides, the L452R and T478K mutations in the RBD also contribute to this feature (Baral et al. 2021). Several reports from the UK proved that a single dose of ChAdOx1 nCoV-19 (AstraZeneca-Oxford) and BNT162b2 (Pfizer-BioNTech) does not protect the people having specific symptoms due to Delta infection. Administering two doses of these vaccines had shown greater efficacy in the Alpha variant compared to Delta. The efficacy rate of the ChAdOx1 nCoV-19 (AstraZeneca-Oxford) and BNT162b2 (Pfizer-BioNTech) for the Delta variant is 66% and 88%, respectively (Bernal et al. 2021). It was noted that the two doses of vaccines for Delta infection did not provide persuasive reports. Therefore, countries like Germany and Israel administered another dose to combat this variant (Hall et al. 2021). Table 3 represents the comparative efficacy of different vaccines against the Wuhan strain (wild-type) and Delta variant of the SARS-CoV-2 virus.
Conclusion
The Delta is a significant, harmful variant of SARS-CoV-2 that evolved during this pandemic. A devastating effect worldwide in recent months is due to the rapid spread of the Delta variant. Several mutations in the viral genome make this strain more transmissible and infectious than the other variants that emerged in a row with Delta. This virulent strain does not show desired response to developed vaccines and therapeutics. Good coverage of vaccines, however, can reduce the disease severity. The prospective of escaping the immune system and the neutralizing antibodies become a concern throughout the globe regarding the Delta variant. Scientists and doctors are worried due to the variant’s immune and vaccine escape phenomena. It is prevalent throughout the world, and the variant might have the capability to contribute to a tremendous surge in different countries within a brief period. The Ro value also suggests the superiority of the strain, indicating the need for more elaborate vaccination drives to end the pandemic in no time. In the landscape of VOCs, the Delta variant is the most transmissible and virulent compared to Alpha, Beta, and Epsilon. The rise and the decline of the prevalence of the Delta variant globally and locally force greater attention to the evolution of viral proteins and interest in understanding the constraints to viral fitness and evolution imposed by RNA properties. Such a changed pattern of the Delta variant also signifies the antigenic shift and step changes in transmissibility to humans. The different vaccines administered in various countries like (AstraZeneca-Oxford) ChAdOx1 nCoV-19, Pfizer-BioNTech BNT162b2, Johnson and Johnson, etc., confers resistance to the variant, but still, the efficacy rate is much lower. Concerning the frequency of the variant, well-prepared strategies are needed to exterminate the variant in every country. At the same time, a strategic and appropriate vaccination drive is required to end the pandemic. However, we urge the scientists to unfold the variant’s molecular, immunological, and virulent features to effectively fight against the Delta variant and eradicate the variant quickly throughout the globe.
References
Abu-Raddad LJ, Chemaitelly H, Yassine HM et al (2021) Pfizer-BioNTech mRNA BNT162b2 Covid-19 vaccine protection against variants of concern after one versus two doses. J Travel Med 28:taab083
Antony P, Vijayan R (2021) Molecular dynamics simulation study of the interaction between human angiotensin converting enzyme 2 and spike protein receptor binding domain of the SARS-CoV-2 B. 1.617 Variant. Biomolecules 11:1244
Shiehzadegan S, Alaghemand N, Fox M et al (2021) Analysis of the Delta variant B. 1.617. 2 COVID-19. Clin Pract 11:778–784
Baral P, Bhattarai N, Hossen ML et al (2021) Mutation-induced changes in the receptor-binding interface of the SARS-CoV-2 Delta variant B. 1.617. 2 and implications for immune evasion. Biochem Biophys Res Commun 574:14–19
Beck DA, Alonso DO, Inoyama D et al (2008) The intrinsic conformational propensities of the 20 naturally occurring amino acids and reflection of these propensities in proteins. Proc Natl Acad Sci USA 105:12259–12264
Bernal JL et al (2021) Effectiveness of Covid-19 vaccines against the B. 1.617. 2 (Delta) variant. N Engl J Med 385:585–594
Bhattacharya M, Sharma AR, Dhama K et al (2022) Omicron variant (B. 1.1. 529) of SARS-CoV-2: understanding mutations in the genome, S-glycoprotein, and antibody-binding regions. GeroScience 44:619–637
Bruxvoort KJ, Sy LS, Qian L, Ackerson BK et al (2021) Effectiveness of mRNA-1273 against Delta, mu, and other emerging variants of SARS-CoV-2: test negative case-control study. bmj 375:e068848
Burki TK (2021) Lifting of COVID-19 restrictions in the UK and the Delta variant. Lancet Respir Med 9:e85. https://doi.org/10.1016/S2213-2600(21)00328-3
Campbell F, Archer B, Laurenson-Schafer H et al (2021) Increased transmissibility and global spread of SARS-CoV-2 variants of concern as at June 2021. Euro Surveill 26:2100509
Chakraborty C, Bhattacharya M, Sharma AR (2021a) Present variants of concern and variants of interest of severe acute respiratory syndrome coronavirus 2: their significant mutations in S-glycoprotein, infectivity, re-infectivity, immune escape and vaccines activity. Rev Med Virol 32:e2270. https://doi.org/10.1002/rmv.2270
Chakraborty C, Sharma A, Sharma G et al (2020) SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options. Eur Rev Med Pharmacol Sci 24:4016–4026
Chakraborty C, Sharma AR, Bhattacharya M et al (2021b) The current second wave and COVID-19 vaccination status in India. Brain Behav Immun 96:1–4
Chakraborty C, Sharma AR, Bhattacharya M et al (2021c) Evolution, mode of transmission, and mutational landscape of newly emerging SARS-CoV-2 variants. Mbio 12:e01140-e11121
Chakraborty C, Sharma AR, Bhattacharya M et al (2021d) Asian-origin approved COVID-19 vaccines and current status of COVID-19 vaccination program in Asia: a critical analysis. Vaccines 9:600. https://doi.org/10.3390/vaccines9060600
Chakraborty C, Sharma AR, Bhattacharya M et al (2021e) Ongoing clinical trials of vaccines to fight against COVID-19 pandemic. Immune Netw 21:e5. https://doi.org/10.4110/in.2021.21.e5
Chakraborty C, Sharma AR, Bhattacharya M et al (2022a) A paradigm shift in the combination changes of SARS-CoV-2 variants and increased spread of Delta variant (B. 1.617. 2) across the world. Aging Dis 13:927–942
Chakraborty C, Sharma AR, Bhattacharya M et al (2022b) Comparative genomics, evolutionary epidemiology, and RBD-hACE2 receptor binding pattern in B. 1.1. 7 (Alpha) and B. 1.617. 2 (Delta) related to their pandemic response in UK and India. Infect Genet Evol 101:105282
Chakraborty C, Bhattacharya M, Sharma AR (2022c) Emerging mutations in the SARS-CoV-2 variants and their role in antibody escape to small molecule-based therapeutic resistance. Curr Opin Pharmacol 62:64–73
Chakraborty C, Bhattacharya M, Sharma AR et al (2022d) Recombinant SARS-CoV-2 variants XD, XE, and XF: the emergence of recombinant variants requires an urgent call for research–Correspondence. Int J Surg 102:106670
Chakraborty C, Sharma AR, Bhattacharya M et al (2022e) A detailed overview of immune escape, antibody escape, partial vaccine escape of SARS-CoV-2 and their emerging variants with escape mutations. Front Immunol 13:801522
Chemmama IE, Pelea AC, Bhandari YR et al (2012) Structural propensities and entropy effects in peptide helix-coil transitions. Phys Rev E 86:031915
Cherian S, Potdar V, Jadhav S et al (2021) SARS-CoV-2 spike mutations, L452R, E484Q and P681R, in the second wave of COVID-19 in Maharashtra, India. Microorganisms 9:1542
CDC (2021) SARS-CoV-2 variant classifications and definitions. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html (Acession date 12 Nov 2021)
Del Rio C, Malani PN, Omer SB (2021) Confronting the Delta variant of SARS-CoV-2, summer 2021. JAMA 326:1001–1002
Dolzhikova I, Gushchin V, Shcheblyakov D et al (2021) One-shot immunization with Sputnik Light (the first component of Sputnik V vaccine) is effective against SARS-CoV-2 Delta variant: efficacy data on the use of the vaccine in civil circulation in Moscow. medRxiv. https://doi.org/10.1101/2021.10.08.21264715
Duong D (2021) Alpha, Beta, Delta, Gamma: what’s important to know about SARS-CoV-2 variants of concern? CMAJ 193:E1059–E1060
Dyer O (2021) Covid-19: unvaccinated face 11 times risk of death from Delta variant. CDC Data Show BMJ 2021(374):n2282
Ella R, Reddy S, Blackwelder W et al (2021) Efficacy, safety, and lot-to-lot immunogenicity of an inactivated SARS-CoV-2 vaccine (BBV152): interim results of a randomised, double-blind, controlled, phase 3 trial. Lancet 398:2173–2184
Elbe S, Buckland-Merrett G (2017) Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob Chall 1:33–46
Farinholt T, Doddapaneni H, Qin X et al (2021) Transmission event of SARS-CoV-2 Delta variant reveals multiple vaccine breakthrough infections. BMC Med 19:1–6
Finkelstein MT, Mermelstein AG, Parker Miller E et al (2021) Structural analysis of neutralizing epitopes of the SARS-CoV-2 spike to guide therapy and vaccine design strategies. Viruses 13:134
Gobeil SM, Janowska K, McDowell S et al (2021) Effect of natural mutations of SARS-CoV-2 on spike structure, conformation and antigenicity. Science 373(6555):eabi622
Gómez CE, Perdiguero B, Esteban M (2021) Emerging SARS-CoV-2 variants and impact in global vaccination programs against SARS-CoV-2/COVID-19. Vaccines 9:243
Hall VG, Ferreira VH, Ku T, Ierullo M et al (2021) Randomized trial of a third dose of mRNA-1273 vaccine in transplant recipients. N Engl J Med 385:1244–1246
Harder T, Külper-Schiek W, Reda S et al (2021) Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B. 1.617. 2) variant: second interim results of a living systematic review and meta-analysis, January 1 to August 25 2021. Euro Surveill 14(26):2100920
Hatmal MM, Alshaer W, Al-Hatamleh MA et al (2020) Comprehensive structural and molecular comparison of spike proteins of SARS-CoV-2, SARS-CoV and MERS-CoV, and their interactions with ACE2. Cells 9:2638
Kannan SR, Spratt AN, Cohen AR et al (2021) Evolutionary analysis of the Delta and Delta Plus variants of the SARS-CoV-2 viruses. J Autoimmun 124:102715. https://doi.org/10.1016/j.jaut.2021.102715
Katella K (2021) Things to know about the Delta variant. Yale Medicine News. https://www.yalemedicine.org/news/5-things-to-know-delta-variant-covid (Acessed on 12 Jun 2022)
Katul GG, Mrad A, Bonetti S et al (2020) Global convergence of COVID-19 basic reproduction number and estimation from early-time SIR dynamics. PLoS ONE 15:e0239800
Kumar S, Thambiraja TS, Karuppanan K et al (2022) Omicron and Delta variant of SARS-CoV-2: a comparative computational study of spike protein. J Med Virol 94:1641–1619
Kunal S, Gupta K, Ish P (2021) COVID-19 variants in India: potential role in second wave and impact on vaccination. Heart Lung 50:784–787. https://doi.org/10.1016/j.hrtlng.2021.05.008
Le Bert N, Tan AT, Kunasegaran K et al (2020) SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 584:457–462
Li XN, Huang Y, Wang W et al (2021) Effectiveness of inactivated SARS-CoV-2 vaccines against the Delta variant infection in Guangzhou: a test-negative case–control real-world study. Emerg Microbes Infect 10:1751–1759
Liu Y, Rocklöv J (2021) The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J Travel Med 28:taab124
Liu Z, VanBlargan LA, Bloyet LM et al (2021) Identification of SARS-CoV-2 spike mutations that attenuate monoclonal and serum antibody neutralization. Cell Host Microbe 29(477–488):e474
McCallum M, Bassi J, De Marco A et al (2021) SARS-CoV-2 immune evasion by variant B. 1.427/B. 1.429 variant of concern. Science 373:648–654
Menni C, Valdes AM, Polidori L et al (2022) Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of Omicron and Delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet 399:1618–1624
Mlcochova P, Kemp S, Dhar MS et al (2021) SARS-CoV-2 B. 1.617. 2 Delta variant emergence and vaccine breakthrough. biorxiv. https://doi.org/10.1101/2021.05.08.443253
Moderbacher CR, Ramirez SI, Dan JM et al (2020) Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell 183(996–1012):e1019
Mohapatra RK, Tiwari R, Sarangi AK et al (2022) Twin combination of Omicron and Delta variant triggering a Tsunami wave of ever high surges in COVID-19 cases: a challenging global threat with a special focus on Indian sub-continent. J Med Virol 94:1761–1765
Nextstrain (2021) Nextstrain SARS-CoV-2 resources, on Nextstrain. https://nextstrain.org/sars-cov-2/ (Acessed on 27 Oct 2021)
O'Toole A (2021) cov-lineages. org website. Zenodo. https://cov-lineages.org/ (Acessed on 27 Oct 2021)
Ogawa J, Zhu W, Tonnu N et al (2020) The D614G mutation in the SARS-CoV2 Spike protein increases infectivity in an ACE2 receptor dependent manner. Biorxiv. https://doi.org/10.1101/2020.07.21.214932
Ong SW, Chiew CJ, Ang LW et al (2021) Clinical and virological features of SARS-CoV-2 variants of concern: a retrospective cohort study comparing B. 1.1. 7 (Alpha), B. 1.315 (Beta), and B. 1.617. 2 (Delta). Clin Infect Dis. https://doi.org/10.1093/cid/ciab721
Peacock TP, Sheppard CM, Brown JC et al (2021) The SARS-CoV-2 variants associated with infections in India, B. 1.617, show enhanced spike cleavage by furin. Biorxiv. https://doi.org/10.1101/2021.05.28.446163
Planas D, Veyer D, Baidaliuk A et al (2021) Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature 596:276–280
Plante JA, Mitchell BM, Plante KS et al (2021) The variant gambit: COVID’s next move. Cell Host Microbe 29:508–515
Polinski JM, Weckstein AR, Batech Met al (2021) Effectiveness of the single-dose Ad26. COV2. S COVID vaccine. MedRxiv. https://doi.org/10.1101/2021.09.10.21263385
Press Information Bureau (PIB) GoI (2021) Union Health Ministry advises Maharashtra, Kerala and Madhya Pradesh on Delta Plus Variant, currently a Variant of Concern (VOC). https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1729467 (Acessed on 20 Oct 2021)
Rao VU, Arakeri G, Subash A et al (2020) COVID-19: loss of bridging between innate and adaptive immunity? Med Hypotheses 144:109861
Salehi-Vaziri M, Jalali T, Farahmand B et al (2021) Clinical characteristics of SARS-CoV-2 by re-infection vs. reactivation: a case series from Iran. Eur J Clin Microbiol Infect Dis 40:1713–1719
Shastri J, Parikh S, Aggarwal V et al (2021) Severe SARS-CoV-2 breakthrough reinfection with Delta variant after recovery from breakthrough infection by Alpha variant in a fully vaccinated health worker. Front Med 1379
Shu Y, McCauley J (2017) GISAID: Global initiative on sharing all influenza data–from vision to reality. Euro Surveill 22:30494
Singanayagam A, Patel M, Charlett A et al (2020) Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill 25:2001483
Tchesnokova V, Kulasekara H, Larson L et al (2021) Acquisition of the L452R mutation in the ACE2-binding interface of Spike protein triggers recent massive expansion of SARS-Cov-2 variants. J Clin Microbiol 59:e00921-e1021
Vaidyanathan G (2021) Coronavirus variants are spreading in India—what scientists know so far. Nature 593:321–322
Volz E, Hill V, McCrone JT et al (2021) Evaluating the effects of SARS-CoV-2 spike mutation D614G on transmissibility and pathogenicity. Cell 184(64–75):e11
Walensky RP, Walke HT, Fauci AS (2021) SARS-CoV-2 variants of concern in the United States—challenges and opportunities. JAMA 325:1037–1038
Wang L, Gao GF (2022) The “Wolf” is indeed coming: recombinant “Deltacron” SARS-CoV-2 detected. China CDC Weekly 4:285
Wang Y, Chen R, Hu F et al (2021) Transmission, viral kinetics and clinical characteristics of the emergent SARS-CoV-2 Delta VOC in Guangzhou, China. Eclinicalmedicine 40:101129
Weisblum Y, Schmidt F, Zhang F et al (2020) Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. Elife 9:e61312
Wrenn JO, Pakala SB, Vestal G et al (2022) COVID-19 severity from Omicron and Delta SARS-CoV-2 variants. Viruses, Influenza and Other Respiratory. https://doi.org/10.1111/irv.12982
Yadav PD, Sapkal GN, Abraham P et al (2021) Neutralization of variant under investigation B. 1.617 with sera of BBV152 vaccinees. Clin Infect Dis 72:366–368
Yi C, Sun X, Ye J et al (2020) Key residues of the receptor binding motif in the spike protein of SARS-CoV-2 that interact with ACE2 and neutralizing antibodies. Cell Mol Immunol 17:621–630
Zhang J, Xiao T, Cai Y et al (2021) Membrane fusion and immune evasion by the spike protein of SARS-CoV-2 Delta variant. Science 374:1353–1360
Author information
Authors and Affiliations
Contributions
MB, SC, and CC performed the data collection, formal analysis, and manuscript draft writing; MB and SC, and CC developed the figures and tables; ARS reviewed and edited the final manuscript. SSL and CC supervised the whole work. All authors contributed substantially to the manuscript, and approved the final manuscript for submission. All authors are responsible for the integrity, accuracy, and presentation of the data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhattacharya, M., Chatterjee, S., Sharma, A.R. et al. Delta variant (B.1.617.2) of SARS-CoV-2: current understanding of infection, transmission, immune escape, and mutational landscape. Folia Microbiol 68, 17–28 (2023). https://doi.org/10.1007/s12223-022-01001-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-022-01001-3