Abstract
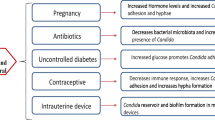
When it comes to women’s health, treating vaginal infections makes up a high proportion of the gynecological services. Among the forms of vaginitis, vulvovaginal candidiasis (VVC) is considered the second most common. Demand for new treatment alternatives is increasingly relevant, especially for therapies with fewer side effects, better tolerability, and lower cost, while still offering improved quality of life in terms of disease prevention. This study intended to investigate the alternative therapies described for the adjuvant treatment of vulvovaginitis caused by Candida species, including alternative and complementary treatment methods used by women. This literature review is based on articles written in English and Portuguese in the PubMed, Google Scholar, and SciELO databases. This study was conducted for the most part using the Brazilian Government’s Capes Periodicals Portal, which directs to Google Scholar and PubMed. Since the 1980s, there has been growing interest in alternative therapies in Brazil, a trend which also began in other Western countries in the second half of the twentieth century. Some alternative treatments include substances with antifungal activity, some substances help restore the balance of the vaginal microbiota, while others have an inhibitory activity on microbial virulence factors. The proper use of therapeutic alternatives can effectively contribute to the treatment of VVC, but it should be remembered that some chemical products, such as boric acid or vinegar, and even natural products such as propolis, garlic, and tea tree may have undesirable side effects, having not been tested by well-designed clinical studies. Even so, alternative therapies in the treatment of VVC do have support in the scientific literature.
Similar content being viewed by others
References
Abbas AM, Shaaban OM, Badran SM et al (2016) Risk factors and health hazards of vaginal infections in upper Egypt: a cross sectional study. Thai J Obstet Gynecol 24:50–56
Bahadoran P, Rokni FK, Fahami F (2010) Investigating the therapeutic effect of vaginal cream containing garlic and thyme compared to clotrimazole cream for the treatment of mycotic vaginitis. Iran J Nurs Midwifery Res 15(Suppl1):343–349
Bernardo KMR, Lima APW (2015) Candidiasis within cytological tests of patients’ at Hospital Geral de Curitiba. Rev Saúde e Desenvolvimento 8(4):198–206
Brandolt TM, Klafke GB, Gonçalves CV et al (2007) Prevalence of Candida spp. in cervical-vaginal samples and the in vitro susceptibility of isolates. Braz J Microbio 48(1):145–150
Brasil (2012). Práticas integrativas e complementares: plantas medicinais e fitoterapia na Atenção Básica. Ministério da Saúde. http://bvsms.saude.gov.br/bvs/publicacoes/praticas_integrativas_complementares_plantas_medicinais_cab31.pdf. Accessed 19 January 2018
Bunick CG, Lott JP, Warren CB, Galan A, Bolognia J, King BA (2012) Chemical burn from topical apple cider vinegar. J Am Acad Dermatol 67(4):e143–e144
Capoci IRG, Bonfim-Mendonça OS, Arita GS et al (2015) Propolis is an efficient fungicide and inhibitor of biofilm production by vaginal Candida albicans. Evid Based Complement Alternat Med 2015:1–9
Centers for Disease Control and Prevention (CDC) (2015). Sexually transmitted diseases treatment guidelines. http://www.cdc.gov/mmwr/pdf/rr/rr6403.pdf. Accessed 19 November 2017
Colombo AL, Guimarães T, Camargo LFA, Richtmann R, de Queiroz-Telles F, Salles MJC, da Cunha CA, Yasuda MAS, Moretti ML, Nucci M (2013) Brazilian guidelines for the management of candidiasis - a joint meeting report of three medical societies: Sociedade Brasileira de Infectologia, Sociedade Paulista de Infectologia and Sociedade Brasileira de Medicina Tropical. Braz J Infect Dis 17(3):283–312
Costa ACBP, Teodoro GR, Ferreira T et al (2010) Antifungal activity of Melaleuca alternifolia essential oil on yeasts isolated from HIV positive pregnant women with oral candidiasis. Rev Inst Adolfo Lutz 69(3):40–407
Cruz PL, Sampaio SF (2016) The unconventional therapeutic practices in health care: integrative review. Rev APS 19(3):483–494
Darvishi M, Jahdi F, Hamzegardeshi Z, Goodarzi S, Vahedi M (2015) The comparison of vaginal cream of mixing yogurt, honey and clotrimazole on symptoms of vaginal candidiasis. Glob J Health Sci 7(6):108–116
De Rossi T, Lozovoy M, Silva R et al (2011) Interactions between Candida albicans and host. Semina: Ciências Biológicas e da Saúde 32(1):15–28
De Seta FS, Schmidt M, Vu B et al (2009) Antifungal mechanisms supporting boric acid therapy of Candida vaginitis. J Antimicrob Chemother 63:325–336
Donders G, Ruban K, Bellen G (2015) Selecting anti-microbial treatment of aerobic vaginitis. Curr Infect Dis Rep 17(5):477
Ebrahimy F, Dolatian M, Moatar F, Alavi Majd H (2015) Comparison of the therapeutic effects of Garcin® and fluconazole on Candida vaginitis. Singap Med J 56(10):567–572
Falagas ME, Betsi GI, Athanasiou S (2006) Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother 58(2):266–272
Feuerschuette OHM, Silveira SK, Feuerschuette I et al (2010) Recurrent vaginal candidiasis: clinical management. Femina 38(2):31–36
Florianópolis (2016). Protocolo de Enfermagem Volume 3. Saúde da Mulher, acolhimento às demandas da mulher nos diferentes ciclos de vida. http://www.pmf.sc.gov.br/arquivos/arquivos/pdf/02_01_2017_21.02.40.4d97f48e10218f6cfea092bae31421d0.pdf. Accessed 03 July 2018
Fonseca GM, Passos TC, Ninahuaman MFML, Caroci AS, Costa LS (2014) Evaluation of the antimicrobial activity of garlic (Liliaceae Allium sativum) and its aqueous extract. Rev Bras Pl Med 16(3):679–684
Fule SR, Das D, Fule RP (2015) Detection of phospholipase activity of Candida albicans and non-albicans isolated from women of reproductive age with vulvovaginal candidiasis in rural area. Indian J Med Microbiol 33(1):92–95
Garcia-Elorriaga G, Rey-Pineda G (2013) Nutrition and intestinal microflora. J Nutr Ther 2:112–121
Guaschino S, De Seta F, Sartore A et al (2001) Efficacy of maintenance therapy with topical boric acid in comparison with oral itraconazole in the treatment of recurrent vulvovaginal candidiasis. Am J Obstet Gynecol 184(4):598–602
Gunther LSA, Martins HPR, Gimenes F, Abreu ALP, Consolaro MEL, Svidzinski TIE (2014) Prevalence of Candida albicans and non-albicans isolates from vaginal secretions: comparative evaluation of colonization, vaginal candidiasis and recurrent vaginal candidiasis in diabetic and non-diabetic women. São Paulo Med J 132(2):116–120
Happel AU, Jaumdally SZ, Pidwell T et al (2017) Probiotics for vaginal health in South Africa: what is on retailers’ shelves? BMC Womens Health 17(7):1–10
Hoekstra M, Westgate S, Mueller S (2017) Povidone-iodine ointment demonstrates in vitro efficacy against biofilm formation. Int Wound J 14(1):172–179
Ismail AM, Abbas AM, Shams AH et al (2017) The effect of use of vaginal Lactobacillus rhamnosus for prevention of recurrence of vulvovaginal candidiasis; a randomized controlled trial. Thai J Obstet Gynaecol 25(1):62–68
Kanagalingam J, Feliciano R, Hah JH et al (2015) Practical use of povidone-iodine antiseptic in the maintenance of oral health and in the prevention and treatment of common oropharyngeal infections. Int J Clin Pract 69(11):1247–1256
Kondo S, Tabe Y, Yamada T, Misawa S, Oguri T, Ohsaka A, Miida T (2011) Comparison of antifungal activities of gentian violet and povidone-iodine against clinical isolates of Candida species and other yeasts: a frame work to establish topical disinfectant activities. Mycopathologia 173(1):21–25
Lavazzo C, Gkegkes LD, Zarkada LM et al (2011) Boric acid for recurrent vulvovaginal candidiasis: the clinical evidence. J Women’s Health (Larchmt) 20(8):1245–1255
Leão MVP, Silva CRG, Santos SSF et al (2015) Lactobacillus rhamnosus may change the virulence of Candida albicans. Rev Bras Ginecol Obstet 37(9):417–420
Leite Júnior DP, Martins ER, Hahn RC et al (2011) Species of Candida isolated from anatomically distinct sites in military personnel in Cuiabá, Mato Grosso, Brazil. An Bras Dermatol 86(4):675–6780
Lima CF, Bernuci KZ, Moreschi ARC (2013) Atividade antifúngica do óleo essencial de Melaleuca Alternifolia (tea tree) sobre leveduras do gênero Candida da cavidade bucal. In: Encontro Internacional de Produção Cientifica, 8; 2013, Maringá. Anais Eletrônico, Maringá: Cesumar, p. 1–5. http://www.cesumar.br/prppge/pesquisa/epcc2013/oit_mostra/Camila_de_Fatima_Lima.pdf. Accessed 14 February 2018
Lopes NS, Conde BE, Fonseca AS et al (2016) Medicina complementar e alternativa no contexto da ayurveda e da medicina popular no Brasil. Persp Online: Biol &Saúde 20(6):30–44
Lupion GCA, Camacho DP, Negri M (2013) In vitro evaluation of excerpt from propolis as possible source of treatment for vulvovaginal candidiasis. Braz J Surg Clin Res 4(2):11–16
Matsubara VH, Bandaram HMHN, Mayer MP et al (2016) Probiotics as antifungals in mucosal candidiasis. Clin Infect Dis 62(9):1143–1153
Martins N, Ferreira ICFR, Barros L et al (2010) Candidiasis: predisposing factors, prevention, diagnosis and alternative treatment. Mycopathologia 177(5):223–240
Mertas A, Garbusinska A, Szliszka E et al (2015) The influence of tea tree oil (Melaleuca alternifolia) on fluconazole activity against fluconazole-resistant Candida albicans strains. Biomed Res Int 2015:1–9
Miró MS, Rodríguez E, Vigezzi C, Icely PA, Gonzaga de Freitas Araújo M, Riera FO, Vargas L, Abiega C, Caeiro JP, Sotomayor CE (2017) Vulvovaginal candidiasis: an old disease with new challenges. Rev Iberoam Micol 34(2):65–71
Mullins MZ, Trouton KM (2015) BASIC study: is intravaginal boric acid non-inferior to metronidazole in symptomatic bacterial vaginosis? Study protocol for a randomized controlled trial. Trials 16(315):1–7
Nascimento MS, Silva N, Catanozi MPLM et al (2003) Effects of different disinfection treatments on the natural microbiota of lettuce. J Food Prot 66(9):1697–1700
Naud P, Matos JC, Stuczynski JV et al (2007) Doenças sexualmente transmissíveis. In: Ramos JGL, Martins-Costa SH, Barros E, Machado A (eds) Antimicrobianos em Ginecologia e Obstetrícia: Consulta Rápida. Porto Alegre, Artmed, pp 95–118
Ninomiya K, Maruyama N, Inoue S, Ishibashi H, Takizawa T, Oshima H, Abe S (2012) The essential oil of Melaleuca alternifolia (tea tree oil) and its main component, terpinen-4-ol protect mice from experimental oral candidiasis. Biol Pharm Bull 35(6):861–865
Nyirjesy P, Robinson J, Mathew L, Lev-Sagie A, Reyes I, Culhane JF (2011) Alternative therapies in women with chronic vaginitis. Obstet Gynecol 117(4):856–861
Nyirjesy P, Weitz MV, Grody MH et al (1999) Over-the-counter and alternative medicines in the treatment of chronic vaginal symptoms. Obstet Gynecol 90(1):50–53
Oliveira-Júnior JK, Vieira LEM, Barnabé LEG et al (2017) Analysis of antifungal effect of propolis on species of Candida albicans and non-albicans. Revista Uningá 30(3):45–51
Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, Filler SG, Fisher JF, Kullberg BJ, Ostrosky-Zeichner L, Reboli AC, Rex JH, Walsh TJ, Sobel JD, Infectious Diseases Society of America (2009) Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 48(5):503–535
Papa R, Troncone MG, Altruda F, Rullo V, Saponati G (2017) Clinical evaluation of the efficacy and safety of a medical vaginal device containing Rigenase® for the treatment of vaginosis: a randomized study. J Clin Gynecol Obstet 6(1):6–11
Petersen EE, Weissenbacher ER, Hengst P, Spitzbart H, Weise W, Wolff F, Dreher E, Ernst U, Della Casa V, Pohlig G, Graf F, Kaiser RR (2002) Local treatment of vaginal infections of varying etiology with dequalinium chloride or povidone iodine. A randomised, double-blind, active-controlled, multicentric clinical study. Arzneimittelforschung 52(9):706–715
Pinto TMS, Neves ACC, Leão MVP, Jorge AOC (2008) Vinegar as an antimicrobial agent for control of Candida spp. in complete denture wearers. J Appl Oral Sci 16(6):385–390
Pirotta MV, Gunn JM, Chondros P (2003) “Not thrush again!” Women’s experience of post-antibiotic vulvovaginitis. Med J Aust 179(1):43–46
Pointer BR, Bover MP, Schmidt M (2015) Boric acid destabilizes the hyphal cytoskeleton and inhibits invasive growth of Candida albicans. Yeast 32(4):389–398
Reid G, Jass J, Sebulsky MT, McCormick JK (2003) Potential uses of probiotics in clinical practice. Clin Microbiol Ver 16(4):658–672
Rodrigues MT, Simões LZ, Diniz CG (2009) Clinical, microbiological and therapeutic aspects of vulvovaginal candidiasis and recurrent vulvovaginal candidiasis: importance of regional surveys. HU Rev 35(3):175–181
Santos CMA, Pires MCV, Leão TL et al (2016) Selection of Lactobacillus strains as potential probiotics for vaginitis treatment. Microbiology 126(7):1195–1207
Santos CMA, Pires MCV, Leão TL, Silva AKS, Miranda LS, Martins FS, Silva AM, Nicoli JR (2018) Anti-inflammatory effect of two Lactobacillus strains during infection with Gardnerella vaginalis and Candida albicans in a HeLa cell culture model. Microbiology 164(3):349–358
Secor WE (2010) Trichomonas vaginalis: treatment questions and challenges. Expert Rev Anti-Infect Ther 10(2):107–109
Sexual Health Medicine (2018) Treatment of vulvovaginal candidiasis. http://sexualhealthmedicine.com/vaginal-diseases/treatment-of-vulvovaginal-candidiasis. Accessed on 26 January 2018
Shaaban OM, Abbas AM, Moharram AM, Farhan MM, Hassanen IH (2015) Does vaginal douching affect the type of candidal vulvovaginal infection? Med Mycol 53:817–827
Soares R, Vieira-Baptista P, Tavares S (2017) Cytolytic vaginosis: an underdiagnosed pathology that mimics vulvovaginal candidiasis. Acta Obstet Ginecol Port 11(2):106–112
Sobel JD, Chaim W, Nagappan V, Leaman D (2003) Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol 189(5):1297–1300
Sobel JD, Chaim W (1997) Treatment of Torulopsis glabrata vaginitis: retrospective review of boric acid therapy. Clin Infect Dis 24(4):649–652
Sociedade Portuguesa de Ginecologia (2012). Revisão dos consensos em infecções vulvovaginais. http://www.spginecologia.pt/uploads/revisao_dos_consensos_em_infeccoes_vulgovaginais.pdf. Accessed 06 November 2017
Streicher, LF, Zar FA (1993) Chronic Vaginites. In: Knaus V, Isaacs JH, (ed) Office gynecology: advanced management concepts. Springer-Verlag; pp 30–48
Van der Meijden WI, Piot P, Schmitz PIM et al (1987) Treatment of clue cell-positive discharge with 200 mg povidone-iodine pessaries. A double-blind and placebo-controlled trial. Eur J Obstet Gynecol Reprod Biol 24(4):299–307
Wagner RD, Johnson SJ (2012) Probiotic lactobacillus and estrogen effects on vaginal epithelial gene expression responses to Candida albicans. J Biomed Sci 19(1):84
Watson C, Calabretto H (2007) Comprehensive review of conventional and non-conventional methods of management of recurrent vulvovaginal candidiasis. Aust N Z J Obstet Gynaecol 47(4):262–272
Watson CJ, Grando D, Fairley CK, Chondros P, Garland SM, Myers SP, Pirotta M (2014) The effects of oral garlic on vaginal candida colony counts: a randomised placebo controlled double-blind trial. BJOG 121(4):498–506
Wewalka G, Stary A, Bosse B, Duerr HE, Reimer K (2002) Efficacy of povidone-iodine vaginal suppositories in the treatment of bacterial vaginosis. Dermatology 204(suppl.1):79–85
Wong R, Wong V, Hung E et al (2011) Topical application of povidone-iodine before wound closure is associated with significant increase in serum iodine levels. Surg Pract 15(3):79–82
Zahedi N, Abedian KS, Mohseni S et al (2016) Is human Dectin-1 Y238X gene polymorphism related to susceptibility to recurrent vulvovaginal candidiasis? Curr Med Mycol 2(3):15–19
Acknowledgments
The authors are grateful to FAPEMIG (Fundação de Amparo a Pesquisa do Estado de Minas Gerais, Brazil), call announcement 001/2017, for the award of a master’s degree scholarship to TC Felix.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflicts of interests.
Rights and permissions
About this article
Cite this article
Felix, T.C., de Brito Röder, D.V.D. & dos Santos Pedroso, R. Alternative and complementary therapies for vulvovaginal candidiasis. Folia Microbiol 64, 133–141 (2019). https://doi.org/10.1007/s12223-018-0652-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-018-0652-x