Abstract
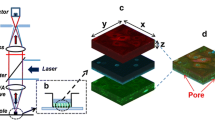
Cell culture models of epithelial barriers in the body are widely used to study the permeation of nutrients, drugs, infectious agents and pollutants into the body tissues and circulation. The NCI-H441 cell line cultured at the air-liquid interface mimics certain phenotypic and functional characteristics of the human alveolar epithelium. Here the permeability properties of the NCI-H441 model were characterised and compared against published data using experimental measurements and mathematical modelling. Cells were cultured under air-liquid interface conditions and trans-epithelial electrical resistance (TEER) and apparent permeability (Papp) to sodium fluorescein (MW 383 Da) and fluorescently labelled dextrans (MW 4000–150,000 Da) was measured. It was found that TEER was independent of cell seeding density while Papp decreased with higher seeding density and plateaued beyond a density of 500,000 cells/cm2. Using the framework of functional pore analysis, a mathematical model was fitted to Papp values measured in this work as well as previously published datasets from human cell lines and primary human and rat cells. It was found that the air-liquid interface NCI-H441 model most closely matched the primary cell line results in contrast to published data using A549 and liquid-interface NCI-H441 cell cultures, supporting the use of this model to study the permeability of the alveolar epithelium to large molecules.



Similar content being viewed by others
References
Beck, R. E., and J. S. Schultz. Hindrance of solute diffusion within membranes as measured with microporous membranes of known pore geometry. Biochim. Biophys. Acta. 255:273–280, 1972.
Cipolla, D. Will pulmonary drug delivery for systemic application ever fulfill its rich promise. Expert Opin. Drug Deliv. 13(10):1337–1340, 2016.
Cryan, S. A., N. Sivadas, and L. Garcia-Contreras. In vivo animal models for drug delivery across the lung mucosal barrier. Adv. Drug. Deliv. Rev. 59:1133–1151, 2007.
Ehrhardt, C., J. Fiegel, S. Fuchs, R. Abu-Dahab, U. F. Schaefer, J. Hanes, and C. M. Lehr. Drug absorption by the respiratory mucosa: cell culture models and particulate drug carriers. J. Aerosol. Med. 15:131–139, 2002.
Ehrhardt, C., K.-J. Kim, and M. Laue. In Vitro Models of the Alveolar Epithelial Barrier Drug Absorption Studies. New York: Springer, pp. 258–282, 2008.
Elbert, K. J., U. F. Schafer, H. J. Schafers, K. J. Kim, V. H. L. Lee, and C. M. Lehr. Monolayers of human alveolar epithelial cells in primary culture for pulmonary absorption and transport studies. Pharm. Res. 16:601–608, 1999.
Frank, J. A. Claudins and alveolar epithelial barrier function in the lung. Ann. N. Y. Acad. Sci. 1257:175–183, 2012.
Frost, T. S., L. Jiang, R. M. Lynch, and Y. Zohar. Permeability of epithelial/endothelial barriers in transwells and microfluidic bilayer devices. Micromachines. 10:533, 2019.
Ghadiri, M., P. M. Young, and D. Traini. Strategies to enhance drug absorption via nasal and pulmonary routes. Pharmaceutics. 11(13):113, 2019.
Günzel, D., and A. D. Yu. Claudins and the modulation of tight junction permeability. Physiol. Rev. 93(2):525–569, 2013.
Huh, D., B. D. Matthews, A. Mammoto, M. Montoya-Zavala, H. Y. Hsin, and D. E. Ingber. Reconstituting organ-level lung functions on a chip. Science. 328:1662–1668, 2010.
Kim, K. J., Z. Borok, and E. D. Crandall. A useful in vitro model for transport studies of alveolar epithelial barrier. Pharm. Res. 18:253–255, 2001.
Kobayashi, S., S. Kondo, and K. Juni. Permeability of peptides and proteins in human cultured alveolar A549 cell monolayer. Pharm. Res. 12:1115–1119, 1995.
Matsukawa, Y., V. H. L. Lee, E. D. Crandall, and K. J. Kim. Size dependent dextran transport across rat alveolar epithelial cell monolayers. J. Pharm. Sci. 86:305–309, 1997.
Nalayanda, D. D., C. Puleo, W. B. Fulton, L. M. Sharp, T.-H. Wang, and F. Abdullah. An open-access microfluidic model for lung-specific functional studies at an air-liquid interface. Biomed. Microdevices. 11:1081, 2009.
Overgaard, C. E., L. A. Mitchell, and M. Koval. Roles for claudins in alveolar epithelial barrier function. Ann. N. Y. Acad. Sci. 1257(1):167–174, 2012.
Patton, J. S., C. S. Fishburn, and J. G. Weers. The lungs as a portal of entry for systemic drug delivery. Proc. Am. Thorac. Soc. 1(4):338–344, 2004.
Ren, H., N. P. Birch, and V. Suresh. An optimised human cell culture model for alveolar epithelial transport. PLoS ONE. 11:e0165225, 2016.
Sakagami, M. In vivo, in vitro and ex vivo models to assess pulmonary absorption and disposition of inhaled therapeutics for systemic delivery. Adv. Drug Deliv. Rev. 58:1030–1060, 2006.
Salomon, J. J., V. E. Muchitsch, J. C. Gausterer, E. Schwagerus, H. Huwer, N. Daum, C. M. Lehr, and C. Ehrhardt. The cell line NCl-H441 is a useful in vitro model for transport studies of human distal lung epithelial barrier. Mol. Pharm. 11(3):995–1006, 2014.
Stucki, J. D., N. Hobi, A. Galimov, et al. Medium throughput breathing human primary cell alveolus-on-chip model. Sci. Rep. 8:14359, 2018.
Watson, C. J., M. Rowland, and G. Warhurst. Functional modeling of tight junctions in intestinal cell monolayers using polyethylene glycol oligomers. Am. J. Physiol. Cell Physiol. 281:C388-397, 2001.
Zamprogno, P., S. Wüthrich, S. Achenbach, et al. Second-generation lung-on-a-chip with an array of stretchable alveoli made with a biological membrane. Commun. Biol. 4:168, 2021.
Zihni, C., C. Mills, K. Matter, et al. Tight junctions: from simple barriers to multifunctional molecular gates. Nat. Rev. Mol. Cell Biol. 17:564–580, 2016.
Acknowledgments
Author VS declares that he has no conflict of interest. This work was supported by the RSNZ Marsden Fund (Grant No. UOA-1411).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael R. King oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suresh, V. Permeability Properties of an In Vitro Model of the Alveolar Epithelium. Cel. Mol. Bioeng. 14, 653–659 (2021). https://doi.org/10.1007/s12195-021-00690-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-021-00690-z