Abstract
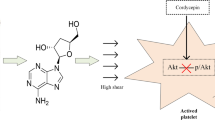
Endothelial cell derived nitric oxide (NO) inhibits the activation and aggregation of platelets. NO inhibition occurs through the intracellular receptor soluble guanylyl cyclase (sGC)-dependent pathways, but there is also evidence of sGC-independent pathways at high NO concentrations. In this study, we integrated a NO-releasing polymer into a microfluidic vascular injury model to measure the relative roles of sGC-dependent and sGC-independent pathways as a function of NO flux and shear rate. Whole blood was perfused at 200–1000 s−1 over collagen with NO wall fluxes of 0.4 and 6.8 × 10−10 mol cm−2 min−1, and 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ) was used to inhibit sGC. A sGC-independent pathway dominated inhibition of platelet aggregation at high NO flux, while the sGC-dependent pathway dominated at low NO flux independent of shear rate. Experiments performed with inhibitors of thrombin or an antagonist of the ADP receptor P2Y12 showed that platelet aggregation was primarily driven by ADP, but that the sGC-independent pathway dominated in both cases at high NO flux. These data suggest that a sGC-independent pathway may play an important role under conditions where NO flux is elevated such as inducible nitric oxide mediated NO production at the site of a vascular injury.







Similar content being viewed by others
References
Antl, M., et al. IRAG mediates NO/cGMP-dependent inhibition of platelet aggregation and thrombus formation. Blood 109:552–559, 2007.
Ballou, D. P., Y. Zhao, P. E. Brandish, and M. A. Marletta. Revisiting the kinetics of nitric oxide (NO) binding to soluble guanylate cyclase: the simple NO-binding model is incorrect. Proc. Natl. Acad. Sci. USA 99:12097–12101, 2002.
Batchelor, M. M., et al. More lipophilic dialkyldiamine-based diazeniumdiolates: synthesis, characterization, and application in preparing thromboresistant nitric oxide release polymeric coatings. J. Med. Chem. 46:5153–5161, 2003.
Bolte, S., and F. P. Cordelières. A guided tour into subcellular colocalization analysis in light microscopy. J. Microsc. 224:213–232, 2006.
Chatterjee, M. S., J. E. Purvis, L. F. Brass, and S. L. Diamond. Pairwise agonist scanning predicts cellular signaling responses to combinatorial stimuli. Nat. Biotechnol. 28:727–732, 2010.
Condorelli, P., and S. C. George. In vivo control of soluble guanylate cyclase activation by nitric oxide: a kinetic analysis. Biophys. J. 80:2110–2119, 2001.
Dangel, O., E. Mergia, K. Karlisch, D. Groneberg, D. Koesling, and A. Friebe. Nitric oxide-sensitive guanylyl cyclase is the only nitric oxide receptor mediating platelet inhibition. J. Thromb. Haemost. 8:1343–1352, 2010.
Doni, M. G., L. Cavallini, and A. Alexandre. Ca2+ influx in platelets: activation by thrombin and by the depletion of the stores. Effect of cyclic nucleotides. Biochem. J. 303:599–605, 1994.
Folie, B. J., and L. V. McIntire. Mathematical analysis of mural thrombogenesis. Concentration profiles of platelet-activating agents and effects of viscous shear flow. Biophys. J. 56:1121–1141, 2005.
Garthwaite, J., E. Southam, C. L. Boulton, E. B. Nielsen, K. Schmidt, and B. Mayer. Potent and selective inhibition of nitric oxide-sensitive guanylyl cyclase by 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one. Mol. Pharmacol. 48:184–188, 1995.
Hansen, R. R., A. A. Tipnis, T. C. White-Adams, J. A. Di Paola, and K. B. Neeves. Characterization of collagen thin films for von Willebrand factor binding and platelet adhesion. Langmuir 27:13648–13658, 2011.
Hansen, R. R., A. R. Wufsus, S. T. Barton, A. A. Onasoga, R. M. Johnson-Paben, and K. B. Neeves. High content evaluation of shear dependent platelet function in a Microfluidic flow assay. Ann. Biomed. Eng. 41:250–263, 2012.
Heemskerk, J., K. S. Sakariassen, J. J. Zwaginga, L. F. Brass, S. P. Jackson, and R. W. Farndale. Collagen surfaces to measure thrombus formation under flow: possibilities for standardization. J. Thromb. Haemost. 9:856–858, 2011.
Homer, K. L., and J. C. Wanstall. Cyclic GMP-independent relaxation of rat pulmonary artery by spermine NONOate, a diazeniumdiolate nitric oxide donor. Br. J. Pharmacol. 131:673–682, 2000.
Homer, K. L., and J. C. Wanstall. Inhibition of rat platelet aggregation by the diazeniumdiolate nitric oxide donor MAHMA NONOate. Br. J. Pharmacol. 137:1071–1081, 2002.
Kibbe, M. Inducible nitric oxide synthase and vascular injury. Cardiovasc. Res. 43:650–657, 1999.
Lies, B., D. Groneberg, S. Gambaryan, and A. Friebe. Lack of effect of ODQ does not exclude cGMP signalling via NO-sensitive guanylyl cyclase. Br. J. Pharmacol. 170:317–327, 2013.
Marcondes, S., et al. Cyclic GMP-independent mechanisms contribute to the inhibition of platelet adhesion by nitric oxide donor: a role for α-actinin nitration. Proc. Natl. Acad. Sci. USA 103:3434–3439, 2006.
Marjanovic, J. A., Z. Li, A. Stojanovic, and X. Du. Stimulatory roles of nitric-oxide synthase 3 and guanylyl cyclase in platelet activation. J. Biol. Chem. 280:37430–37438, 2005.
Morrell, C. N. Regulation of platelet granule exocytosis by S-nitrosylation. Proc. Natl. Acad. Sci. USA 102:3782–3787, 2005.
Naseem, K. M., and W. Roberts. Nitric oxide at a glance. Platelets 22:148–152, 2011.
Neeves, K. B., O. J. T. McCarty, A. J. Reininger, M. Sugimoto, M. R. King, and The Biorheology Subcommittee of the SSC of the ISTH. Flow-dependent thrombin and fibrin generation in vitro: opportunities for standardization: communication from SSC of the ISTH. J. Thromb. Haemost. 12:418–420, 2014.
Onasoga-Jarvis, A. A., T. J. Puls, S. K. O’Brien, L. Kuang, H. J. Liang, and K. B. Neeves. Thrombin generation and fibrin formation under flow on biomimetic tissue factor rich surfaces. J. Thromb. Haemost. 12:373–382, 2014.
Plata, A. M., S. J. Sherwin, and R. Krams. Endothelial nitric oxide production and transport in flow chambers: the importance of convection. Ann. Biomed. Eng. 38:2805–2816, 2010.
Pugh, N., A. M. C. Simpson, P. A. Smethurst, P. G. de Groot, N. Raynal, and R. W. Farndale. Synergism between platelet collagen receptors defined using receptor-specific collagen-mimetic peptide substrata in flowing blood. Blood 115:5069–5079, 2010.
Roberts, W., R. Riba, S. Homer-Vanniasinkam, R. W. Farndale, and K. M. Naseem. Nitric oxide specifically inhibits integrin-mediated platelet adhesion and spreading on collagen. J. Thromb. Haemost. 6:2175–2185, 2008.
Roest, M., A. Reininger, J. J. Zwaginga, M. R. King, and J. W. M. Heemskerk. Flow chamber-based assays to measure thrombus formation in vitro: requirements for standardization. J. Thromb. Haemost. 9:2322–2324, 2011.
Ruggeri, Z. M., and G. L. Mendolicchio. Adhesion mechanisms in platelet function. Circ. Res. 100:1673–1685, 2007.
Schrammel, A., S. Behrends, K. Schmidt, D. Koesling, and B. Mayer. Characterization of 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one as a heme-site inhibitor of nitric oxide-sensitive guanylyl cyclase. Mol. Pharmacol. 50:1–5, 1996.
Sylman, J. L., S. M. Lantvit, M. C. VeDepo, M. M. Reynolds, and K. B. Neeves. Transport limitations of nitric oxide inhibition of platelet aggregation under flow. Ann. Biomed. Eng. 274:2193–2205, 2013.
Trepakova, E. S., R. A. Cohen, and V. M. Bolotina. Nitric oxide inhibits capacitative cation influx in human platelets by promoting sarcoplasmic/endoplasmic reticulum Ca2+-ATPase dependent refilling of Ca2+ stores. Circ. Res. 84:201–209, 1999.
Tsai, M., et al. In vitro modeling of the microvascular occlusion and thrombosis that occur in hematologic diseases using microfluidic technology. J. Clin. Investig. 122:408–418, 2012.
van Gestel, M. A. In vivo blockade of platelet ADP receptor P2Y12 reduces embolus and thrombus formation but not thrombus stability. Arterioscler. Thromb. Vasc. Biol. 23:518–523, 2003.
Van Kruchten, R., J. M. Cosemans, and J. W. Heemskerk. Measurement of whole blood thrombus formation using parallel-plate flow chambers—a practical guide. Platelets 23:229–242, 2012.
Vaughn, M. W., L. Kuo, and J. C. Liao. Estimation of nitric oxide production and reaction rates in tissue by use of a mathematical model. Am. J. Physiol. Heart Circ. Physiol. 274:H2163–H2176, 1998.
Wanstall, J. C., K. L. Homer, and S. A. Doggrell. Evidence for, and importance of, cGMP-independent mechanisms with NO and NO donors on blood vessels and platelets. Curr. Vasc. Pharmacol. 3:41–53, 2005.
Zhang, G., et al. Biphasic roles for soluble guanylyl cyclase (sGC) in platelet activation. Blood 118:3670–3679, 2011.
Acknowledgments
This material is based upon work supported by the National Science Foundation under Grant No. CBET-1351672, the American Heart Association (10SDG2610066, K.B.N.) and Boettcher Foundation Webb-Waring Biomedical Research Awards (K.B.N., M.M.R.).
Conflict of interest
JL.S., S.M.L, M.M.R. and K.B.N declare that they have no conflicts of interest.
Ethical Standards
All human subjects research was carried out in accordance with the Declaration of Helsinki and under the University of Colorado, Boulder Institutional Review Board approval. No animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael R. King oversaw the review of this article.
This paper is part of the 2014 Young Innovators Issue.
Keith B. Neeves is an assistant professor in Chemical and Biological Engineering at the Colorado School of Mines. He obtained his B.S. in chemical engineering from the University of Colorado, Boulder and a Ph.D. in chemical and biomolecular engineering at Cornell University. He was an NIH NRSA postdoctoral fellow at the University of Pennsylvania. His laboratory focuses on transport phenomena in biological tissues. His research has been recognized with a NSF CAREER award, a Scientist Development Grant from the American Heart Association, and Early Career Investigator Awards from the Boettcher Foundation Waring-Webb Biomedical Research Foundation and the Bayer Hemophilia Awards Program.

Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sylman, J.L., Lantvit, S.M., Reynolds, M.M. et al. The Relative Role of Soluble Guanylyl Cylase Dependent and Independent Pathways in Nitric Oxide Inhibition of Platelet Aggregation Under Flow. Cel. Mol. Bioeng. 7, 421–431 (2014). https://doi.org/10.1007/s12195-014-0331-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-014-0331-1