Abstract
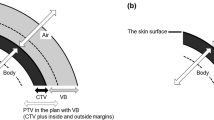
A commercially available flat bolus (commercial bolus) would not fully fit the irregular surfaces of the scalp. We developed a transparent and flexible material with good fitting properties, analyzed its physical characteristics, and evaluated the clinical feasibility of the bolus fabricated using a three-dimensional (3D) printer (3D bolus). To evaluate the physical characteristics of the new material, treatment plans with virtual, 3D, and commercial boluses were created for water-equivalent phantoms using a radiation treatment planning system (RTPS). Using a head phantom and the dose volume histogram calculated with RTPS, dose distributions for total scalp irradiation were compared between the three treatment plans. To evaluate the clinical feasibility, the fitness and reproducibility of the 3D bolus were compared with the head phantom and clinical cases using dice similarity coefficient (DSC) measurements. A good agreement was observed between the percentage depth dose (PDD) curves for the virtual, 3D, and commercial boluses. The homogeneity indexes of the planning target volume (PTV) for the 3D and commercial boluses were 0.083 and 0.153, respectively, proving that the former achieved a better dose uniformity of PTV than the latter. Good fitness and reproducibility with the 3D bolus were observed in both the head phantom and two clinical cases, with mean DSC values of 0.854, 0.829, and 0.843, respectively. These results successfully demonstrated and verified the utility of the 3D bolus for total scalp irradiation.










Similar content being viewed by others
References
Mendenhall WM, Mendenhall NP. Radiotherapy for cutaneous angiosarcoma. In Cognetta AB, Mendenhall WM (eds.), Radiation Therapy for Skin Cancer pp 189–176, Springer Science, New York 2013.
Conic RRZ, Damiani G, Frigerio A, Tsai S, Bragazzi NL, Chu TW, Mesinkovska NA, Shlomo A, Koyfman SA, Joshi NP, Budd T, Vidimos A, Gastman BR. Incidence and outcomes of cutaneous angiosarcoma: a SEER population based study. J Am Acad Dermatol. 2020;83:809–16.
Shin JY, Roh SG, Lee NH, Yang KM. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck. 2017;39:380–6.
Fujisawa Y, Yoshino K, Fujimura T, Nakamura Y, Okiyama N, Ishitsuka Y, Watanabe R, Fujimoto M. Cutaneous angiosarcoma: the possibility of new treatment options especially for patients with large primary tumor. Front Oncol. 2018;8:46.
Lozano F, Perez N, Iglesias A, Xu X, Amendola MA, Scott M, Companioni E, Amendola BE. Volumetric arc therapy for total scalp irradiation: case report for a recurrent basal cell carcinoma of the scalp. Ecancermedicalscience. 2017;11:737.
Ostheimer C, Hübsch P, Janich M, Gerlach R, Vordermark D. Dosimetric comparison of intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) in total scalp irradiation: a single institutional experience. Radiat Oncol J. 2016;34:313–21.
Kelly PJ, Mannarino E, Lewis JH, Baldini EH, Hacker FL. Total dural irradiation: Rapidarc versus static-field IMRT: a case study. Med Dosim. 2012;37:175–81.
Ko S. Evolving radiation therapy techniques for scalp angiosarcoma. Surg Oncol. 2018;27:A1–2.
Hu J, Xiao W, He Z, Kang D, Chen Al, Qi Z. Target splitting non-coplanar RapidArc radiation therapy for a diffuse sebaceous carcinoma of the scalp: a novel delivery technique. Radiat Oncol. 2014;9:204.
Mizumatsu S, Monje ML, Morhardt DR, Rola R, Palmer TD, Fike JR. Extreme sensitivity of adult neurogenesis to low doses of X-irradiation. Cancer Res. 2003;63:4021–7.
Günhan B, Kemikler G, Koca A. Determination of surface dose and the effect of bolus to surface dose in electron beams. Med Dosim. 2003;28:193–8.
Kudchadker RJ, Antolak JA, Morrison WH, Wong PF, Hogstrom KR. Utilization of custom electron bolus in head and neck radiotherapy. J Appl Clin Med Phys. 2003;4:321–33.
Dias AG, Pinto DFS, Borges MF, Pereira MH, Santos JAM, Cunha LT, Lencart J. Optimization of skin dose using in-vivo MOSFET dose measurements in bolus/non-bolus fraction ratio: a VMAT and a 3DCRT study. J Appl Clin Med Phys. 2019;20:63–70.
Bedford JL, Childs PJ, Hansen VN, Warrington AP, Mendes RL, Glees JP. Treatment of extensive scalp lesions with segmental intensity-modulated photon therapy. Int J Radiat Oncol Biol Phys. 2005;62:1549–58.
Butson MJ, Cheung T, Yu P, Metcalfe P. Effects on skin dose from unwanted air gaps under bolus in photon beam radiotherapy. Radiat Meas. 2000;32:201–4.
Khan Y, Villarreal-Barajas JE, Udowicz M, Sinha R, Muhammad W, Abbasi AN, Hussain A. Clinical and dosimetric implications of air gaps between bolus and skin surface during radiation therapy. J Cancer Ther. 2013;4:1251–5.
Benoit J, Pruitt Amy F, Thrall DE. Effect of wetness level on the suitability of wet gauze as a substitute for Superflab as a bolus material for use with 6 mv photons. Vet Radiol Ultrasound. 2009;50:555–9.
Park S-Y, Choi CH, Park JM, Chun M, Han JH, Kim J. A patient-specific polylactic acid bolus made by a 3D printer for breast cancer radiation therapy. PLoS ONE. 2016;11:e0168063.
Burleson S, Baker J, Hsia AT, Xu Z. Use of 3D printers to create a patient-specific 3D bolus for external beam therapy. J Appl Clin Med Phys. 2015;16:166–78.
Chiu T, Tan J, Brenner M, Gu X, Yang M, Westover K, Strom T, Sher D, Jiang S, Zhao B. Three-dimensional printer-aided casting of soft, custom silicone boluses (SCSBs) for head and neck radiation therapy. Pract Radiat Oncol. 2018;8:e167–74.
Su S, Moran K, Robar JL. Design and production of 3D printed bolus for electron radiation therapy. J Appl Clin Med Phys. 2014;15:194–211.
Canters RA, Lips IM, Wendling M, Kusters M, van Zeeland M, Gerritsen RM, Poortmans P, Verhoef CG. Clinical implementation of 3D printing in the construction of patient specific bolus for electron beam radiotherapy for non-melanoma skin cancer. Radiother Oncol. 2016;121:148–53.
Prescribing, Recording, and Reporting Photon-Beam Intensity-Modulated Radiation Therapy (IMRT): Contents. J ICRU. 2010;10.
Dice LR. Measures of the amount of ecologic association between species. Ecology. 1945;26:297–302.
Lin SH, Latronico D, Teslow T, Bajaj GK. A highly reproducible bolus immobilization technique for the treatment of scalp malignancies. Med Dosim. 2008;33:30–5.
Baltz GC, Chi PM, Wong PF, Wang C, Craft DF, Kry SF, Lin SSH, Garden AS, Smith SA, Howell RM. Development and validation of a 3D-printed bolus cap for total scalp irradiation. J Appl Clin Med Phys. 2019;20:89–96.
Kim S-W, Shin H-J, Kay CS, Son SH. A customized bolus produced using a 3-dimensional printer for radiotherapy. PLoS ONE. 2014;9:e110746.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors were provided with 3D boluses by A Just Polymer Corporation.
Research involving human participants
All procedures performed in this study, including those involving human participants, were performed in accordance with the ethical standards of our Institutional Review Board.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board (IRB) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all subjects who participated in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Muramatsu, N., Ito, S., Hanmura, M. et al. Development of a transparent and flexible patient-specific bolus for total scalp irradiation. Radiol Phys Technol 14, 82–92 (2021). https://doi.org/10.1007/s12194-021-00606-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-021-00606-6