Abstract
Tirabrutinib is a Bruton’s tyrosine kinase inhibitor for treating B-cell malignancies. We report the final results of a Phase I study of tirabrutinib in 17 Japanese patients with B-cell malignancies. Patients were administered tirabrutinib at a dose of 160 mg, 320 mg, or 480 mg once daily, or 300 mg twice daily (N = 3, 3, 4, and 7, respectively). Three patients continued tirabrutinib until study completion (November 30, 2020). Adverse events (AEs) occurred in all 17 patients, with Grade 3–4 AEs in 8 (47.1%), serious AEs in 7 (41.2%), drug-related AEs in 16 (94.1%), and Grade 3–4 drug-related AEs in 6 (35.3%). Drug-related AEs reported in 3 or more patients were rash, vomiting, neutropenia, arthralgia, and malaise. One additional serious AE (benign neoplasm of the lung, unrelated to tirabrutinib) occurred after the previous data cutoff (January 4, 2018). Tirabrutinib administration and response assessment were continued for over 4 years in 4 patients. The overall response rate was 76.5% (13/17 patients). The median (range) time to response and duration of response were 0.9 (0.9–5.9) months and 2.59 (0.08–5.45) years, respectively. These findings demonstrate the long-term safety and efficacy of tirabrutinib in Japanese patients with B-cell malignancies.
Clinical trial registration: JapicCTI-142682 (http://www.clinicaltrials.jp/).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bruton’s tyrosine kinase (BTK) is a member of the Tec family of non-receptor protein tyrosine kinases [1, 2] that is highly expressed in hematopoietic cells [3], in which it plays a pivotal role in abnormal B-cell receptor signaling to regulate cell proliferation and survival. Abnormal activity of BTK is observed in a range of B-cell malignancies, including Waldenström macroglobulinemia (WM), chronic lymphocytic leukemia (CLL), and mantle cell lymphoma (MCL) [1, 2]. Therefore, BTK has attracted attention as a potential therapeutic target for these malignancies.
Tirabrutinib (ONO-4059/GS-4059) is a second-generation, highly selective, covalent, irreversible oral inhibitor of BTK that was designed to avoid some limitations of first-generation BTK inhibitors, particularly “off-target” adverse events (AEs) and therapeutic resistance. Preclinical studies provided evidence regarding the cytostatic effects of tirabrutinib in vitro and in vivo [4, 5]. Subsequent clinical trials demonstrated the tolerability and efficacy of tirabrutinib in patients with CLL, MCL, primary central nervous system lymphoma (PCNSL), and WM [6,7,8,9,10,11,12,13,14], which led to its approval in Japan and South Korea [4, 15, 16]. Tirabrutinib was the first BTK inhibitor to be approved for WM and PCNSL in Japan [15], and for PCNSL in South Korea and Taiwan [16, 17].
In clinical use, like other BTK inhibitors, the administration of tirabrutinib can be continued for as long as it shows clinical efficacy. However, some patients discontinue treatment with BTK inhibitors due to toxicities [18,19,20,21,22,23]. Second-generation BTK inhibitors, owing to their higher specificity for BTK, may show an improved toxicity profile permitting longer-term administration. However, long-term data are needed to support this possibility. Follow-up data for patients with CLL or MCL were reported in a European Phase I study [9, 11], but further data including its long-term safety profile are limited.
Several Phase I and II clinical studies have been conducted in Japan in patients with relapsed or refractory B-cell malignancies [7], relapsed or refractory PCNSL [8], and WM [10]. In the first of these studies [7], 4 patients were continuing tirabrutinib at the data cutoff (January 4, 2018). Here, we report the long-term safety and efficacy data obtained through to study completion (November 30, 2020).
Materials and methods
The design of the study (trial registration number: JapicCTI-142682), which adhered to relevant ethical guidelines, including Declaration of Helsinki, was described in more detail in our prior report [7]. The study was approved by the ethics committee/institutional review board at all participating institutions.
Patients with a confirmed histopathological diagnosis and documented history of relapsed or refractory B-cell non-Hodgkin lymphoma [B-NHL: diffuse large B-cell lymphoma (DLBCL), MCL, follicular lymphoma (FL), marginal zone lymphoma, or WM/lymphoplasmacytic lymphoma (LPL)] or CLL/small lymphocytic lymphoma were eligible for this study. The enrollment period was January 2015 to February 2016. All patients provided informed consent. Eligibility criteria are listed in full in the ESM Materials.
Patients were enrolled into 4 dose cohorts (160 mg QD, 320 mg QD, 480 mg QD, and 300 mg BID; cohorts 1–4) in a 3 + 3 dose-escalation scheme. Tirabrutinib was to be continued until progressive disease, unacceptable AEs, or consent withdrawal. Treatment discontinuation, interruption, resumption, and dose modifications were permitted, and the criteria are described in detail in the prior report [7].
Safety was evaluated in terms of AEs and drug-related AEs, laboratory tests, vital signs, and electrocardiography. AEs were assessed using the Common Terminology Criteria for Adverse Events (version 4.0). Drug-related AEs were AEs that were considered to be definitely related, probably related or possibly related to the investigational drug, or AEs with an uncertain relationship to the investigational drug. Five categories of AEs of special interest were also defined as those related to hemorrhage, cytopenia, infection, skin eruption, and diarrhea.
Efficacy was assessed as the best clinical response in accordance with the International Workshop Criteria for NHL, WM, and CLL [24,25,26]. The overall response rate (ORR) was calculated as the sum of complete responses (CR; CR includes unconfirmed CR or CR with incomplete blood count recovery) and partial responses (PR; PR includes very good PR or PR with residual lymphocytosis). Other efficacy outcomes included the duration of response, event-free survival, progression-free survival (PFS), and overall survival (OS).
The safety analyses were conducted using all enrolled patients who received at least one dose of tirabrutinib (safety analysis set). The efficacy analyses were conducted using all enrolled patients who received at least one dose of tirabrutinib (full analysis set). Data analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Patients
As previously described, 17 patients were enrolled and treated in the study, and dose cohorts 1–4 comprised 3, 3, 4, and 7 patients, respectively [7]. There were 5 patients with FL, 4 with non-germinal center B-cell-like (non-GCB) DLBCL, 4 with MCL, 2 with WM, 1 with DLBCL (unknown cell-of-origin), and 1 with CLL (Table 1). The median follow-up through to study completion was 4.3 years, and ranged from 0.04 to 5.8 years. Three patients (MCL: 2 patients; WM: 1 patient) continued tirabrutinib through to study completion (ESM Table 1). One patient with MCL (cohort 3) requested to discontinue tirabrutinib after approximately 2 months of treatment. There were 12 patients with a performance status of 0 and five with a performance status of 1. Approximately half of the patients (9/17, 52.9%) had a history of other medical disorders. Table 1 also lists the frequencies of complications at the time of starting tirabrutinib, including gastrointestinal, cardiovascular, and renal disorders, hypertension, benign prostatic hyperplasia, and abnormal laboratory test values.
Safety
AEs occurred in all 17 patients (Table 2), which included Grade 3–4 AEs in 8 patients (47.1%) and serious AEs in 7 (41.2%). AEs led to dose reductions in 3 patients (17.6%) and treatment interruption in 6 patients (35.3%). Tirabrutinib was permanently discontinued in 2 patients due to an AE (acute myeloid leukemia, neuroendocrine carcinoma of the skin), both in patients treated at a dose of 320 mg QD. Acute myeloid leukemia was diagnosed 764 days after starting tirabrutinib; this event was classified as a drug-related AE by the investigator. Sixteen patients (94.1%) experienced a drug-related AE, of which 6 (35.3%) experienced a Grade 3–4 drug-related AE and 4 (23.5%) experienced a serious drug-related AE. Seven patients (41.2%) died during the study, 6 due to cancer progression and 1 due to graft-versus-host disease after undergoing allogeneic transplantation. None of the deaths were related to an AE.
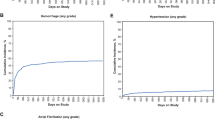
Table 3 lists the drug-related AEs that occurred in ≥ 10% of the patients and drug-related Grade 3–4 AEs during the study, and ESM Table 2 lists all of the AEs, in all patients and according to tirabrutinib dose. Drug-related AEs that occurred in 3 or more patients overall were rash [6 patients (35.3%)], vomiting [4 (23.5%)], neutropenia (neutropenia/neutrophil count decreased; 4 (23.5%)], arthralgia [3 (17.6%)], and malaise [3 (17.6%)]. The drug-related Grade 3–4 AEs were neutropenia in 4 patients (23.5%), leukopenia in 2 (11.8%), and anemia, hypophosphatemia, prothrombin time-international normalized ratio (PT-INR) increased, pneumonitis, and acute myeloid leukemia in 1 patient (5.9%) each. As indicated in Fig. 1, most of the patients experienced drug-related AEs within the first ~ 6 months of starting treatment, and one case of acute myeloid leukemia occurred approximately 2 years (diagnosed on day 764) after starting tirabrutinib. No additional drug-related Grade ≥ 3 AEs occurred more than 3 years after starting treatment.
At the previous cutoff (January 4, 2018), 9 serious AEs had been reported in 7 patients (4 were considered drug related) [7]. In the time between the earlier cutoff date and study completion, one additional serious AE (benign neoplasm of the lung) was reported at 1681 days after starting treatment in a patient treated with 300 mg BID. This serious AE was not considered related to tirabrutinib and the patient recovered.
Five AE categories of special interest were defined (Table 4), with AEs related to hemorrhage, cytopenia, infection, skin eruption, and diarrhea in 4 (23.5%), 5 (29.4%), 8 (47.1%), 10 (58.8%), and 4 (23.5%) patients, respectively. Although not defined as AEs of special interest, there were no cases of atrial fibrillation or hypertension.
Treatment exposure and response
Figure 2 shows the swimmers plot for treatment exposure and response in individual patients according to the type of malignancy and the dose of tirabrutinib. The administration of tirabrutinib and a response to treatment were continued for over 4 years in 2 patients with MCL, 1 with WM, and 1 with CLL. The ORR was 76.5% (13/17 patients), with a median time to response of 0.9 months (range 0.9–5.9 months) and the median duration of response was 2.59 years (range 0.08–5.45 years). The ORR according to the type of malignancy is summarized in ESM Table 3; values are unchanged from the previous report [7]. The median PFS was 2.82 years (95% confidence interval 0.44 years to not reached) and median OS was not reached. The PFS and OS values according to the type of malignancy are summarized in ESM Table 3.
Treatment exposure and duration of response: “On treatment” indicates patients were receiving tirabrutinib. “Off treatment” indicates patients had stopped administration of tirabrutinib but were being followed up in the study. Cohort 1: 160 mg QD; Cohort 2: 320 mg QD; Cohort 3: 480 mg QD; Cohort 4: 300 mg BID. BID twice daily, CLL chronic lymphocytic leukemia, CR complete response, DLBCL diffuse large B-cell lymphoma, FL follicular lymphoma, MCL mantle cell lymphoma, non-GCB DLBCL non-germinal center B-cell-like diffuse large B-cell lymphoma, PD progressive disease, PR partial response, QD once daily, WM Waldenström macroglobulinemia
Discussion
This Phase I study was performed to investigate the maximum tolerated dose of tirabrutinib, as well as its safety, efficacy, and pharmacokinetics, in Japanese patients with relapsed or refractory B-cell NHL or CLL. Results at an earlier cutoff (January 4, 2018) were reported in our previous manuscript [7]. Here, we extend these findings with a longer follow-up of patients, except for 1 patient with MCL in cohort 3 who discontinued tirabrutinib approximately 2 months after starting treatment. Four patients were treated with tirabrutinib for > 5 years, of which 3 continued treatment through to study completion (November 30, 2020). From a safety perspective, the most important findings of the current paper include the frequencies of drug-related AEs and AEs of special interest. Drug-related AEs that occurred in 3 or more patients overall were rash, vomiting, neutropenia, arthralgia, and malaise, and drug-related Grade 3–4 AEs were neutropenia, leukopenia, anemia, hypophosphatemia, PT-INR increased, pneumonitis, and acute myeloid leukemia. It is notable that the majority of drug-related AEs (any Grade, Grade 3–4) occurred within the first 6 months of treatment, and no drug-related Grade 3–4 AEs occurred > 3 years after starting treatment. By comparison, Grade ≥ 3 AEs of clinical interest were reported more than 3 years after starting ibrutinib [27]. In our study, AEs related to hemorrhage, cytopenia, infection, skin eruption, and diarrhea occurred in 4 (23.5%), 5 (29.4%), 8 (47.1%), 10 (58.8%), and 4 (23.5%) patients. From an efficacy perspective, the ORR was unchanged (76.5%) and the median duration of response was extended to 2.59 years (range 0.08–5.45 years) with the longer follow-up of patients.
The safety data in this study are generally consistent with those in prior studies of tirabrutinib. For example, in prior Japanese studies, rash, hematologic AEs, erythema multiforme, and constipation were frequent AEs in a Phase I/II study of 44 patients with PCNSL [8], and rash, hematologic AEs, and stomatitis were the most common AEs in a Phase II study of 27 patients with WM [10]. In international studies, other frequently reported AEs included hematologic AEs, diarrhea, petechiae, rash, nasopharyngitis, upper respiratory tract infection, fatigue, cough, and arthralgia [12, 13].
The Japanese product label for ibrutinib, a first-generation BTK inhibitor, lists 11 categories of adverse drug reactions (ADR) as identified/potential risks in the risk management plan (hemorrhage, bone marrow suppression, infection, arrhythmia, hypersensitivity, tumor lysis syndrome, liver failure/dysfunction, interstitial lung disease, secondary malignant tumors, leukostasis, and oculomucocutaneous syndrome) [5]. It is notable that some of these types of events, including leukostasis, progressive multifocal leukoencephalopathy, arrhythmia, tumor lysis syndrome, hypersensitivity, and oculomucocutaneous syndrome, did not occur in the present study. Atrial fibrillation has been acknowledged as a common reason for discontinuing ibrutinib [20, 28] and concern has been raised regarding hypertension in patients treated with ibrutinib [29,30,31]. Although cardiovascular disorders and hypertension were present in 4 (23.5%) and 8 (47.1%) of patients prior to starting tirabrutinib, no new cases of atrial fibrillation or hypertension were reported in our study.
Hemorrhage-related AEs are a potential class effect of BTK inhibitors. In our study, these events included ear hemorrhage, hematuria, PT-INR increased, Mallory–Weiss syndrome, and purpura, each of which occurred in one patient (5.9%) (Table 4). Of these, PT-INR increased was Grade ≥ 3 and Mallory–Weiss syndrome was classified as a serious AE. Cerebral hemorrhage and gastrointestinal hemorrhage, which are listed as ADRs associated with ibrutinib [5], were not observed in our study. Because hemorrhage-related AEs were observed in this study and some were Grade ≥ 3 or serious, special attention should be paid to the occurrence of such AEs in the future clinical studies of tirabrutinib and in clinical practice.
Infections were also evaluated as AEs of specific interest, and included cystitis, nasopharyngitis, pharyngitis, and sinusitis in 2 patients each (11.8%) (Table 4). There was one Grade ≥ 3 infection-related AE (pneumonia bacterial). All of the infection-related AEs were classified as recovered, with the exception of one case of sinusitis. None of the AEs required treatment interruption and none were considered related to tirabrutinib, except for one case of cystitis. Although the infection-related AEs were manageable in most patients with prophylactic use or treatment with antibacterial agents, some caution may be necessary, especially in patients with serious infections.
Myelosuppression-related AEs included neutropenia/neutrophil count decreased in 4 patients (23.5%), anemia in 3 patients (17.6%), thrombocytopenia/platelet count decreased in 2 patients (11.8%), and leukopenia/white blood cell count decreased in 2 patients (11.8%). These values are generally similar to those reported in the package insert for ibrutinib (anemia, 9.6%; neutropenia, 12.5%; thrombocytopenia, 9.8%) [5].
Rash, diarrhea, headache, nausea, fatigue, and myalgia have been reported for other second-generation BTK inhibitors [32,33,34]. In earlier studies, rash, diarrhea, headache, nausea, fatigue, and myalgia were reported in up to 33%, 58%, 69%, 27%, 21%, and 38% of patients in clinical trials of acalabrutinib [35, 36]. Rash and diarrhea were reported in up to 34% and up to 21% of patients in clinical trials of zanubrutinib [22, 37]. In other studies of tirabrutinib, rash and diarrhea both occurred in up to 44% of the patients [9, 10]. In the present study, rash, diarrhea, headache, nausea, fatigue, and myalgia occurred in 35.3%, 17.6%, 11.8%, 17.6%, 0%, and 5.9% of the patients, respectively. Based on these data, there is a need to pay special attention to these types of AEs in patients treated with tirabrutinib, as with other BTK inhibitors.
From an efficacy perspective, although this was a Phase I study with a limited number of patients, the study enrolled several patients with MCL, WM, and CLL who were treated with tirabrutinib for a long period of time with long responses. These data suggest that tirabrutinib may be effective in patients with MCL, WM, and CLL.
Limitations of this Phase I study include its small sample, dose-escalation design, and the inclusion of multiple subtypes of B-NHL and CLL. These factors may limit the generalizability of the results to broader clinical practice. However, these limitations must be considered in relation to the primary objective of this Phase I study, which was to evaluate the safety and detect potential dose-limiting toxicities, and hence the recommended dose in Japanese patients. Larger studies may be necessary to confirm our results.
With a median follow-up of 4.3 years, this study comprises the longest data set of any tirabrutinib study published to date and 4 patients were continuing treatment for ≥ 5 years. This allowed us to evaluate the long-term safety of tirabrutinib. We observed no additional risks or emergence of Grade ≥ 3 drug-related AEs since the prior cutoff at which time the median follow-up was 2.3 years. The current results, as well as those from the prior report, demonstrate the long-term tolerability of tirabrutinib at doses of 480 mg QD or 300 mg BID in patients with relapsed or refractory B-NHL or CLL, with a low rate of discontinuation due to AEs/drug-related AEs.
Data availability
Qualified researchers may request Ono Pharma to disclose individual patient-level data from clinical studies through the following website: https://www.clinicalstudydatarequest.com/. For more information on Ono Pharma’s Policy for the Disclosure of Clinical Study Data, please see the following website: https://www.ono.co.jp/eng/rd/policy.html.
References
Kurosaki T, Hikida M. Tyrosine kinases and their substrates in B lymphocytes. Immunol Rev. 2009;228:132–48.
Qiu Y, Kung HJ. Signaling network of the BTK family kinases. Oncogene. 2000;19:5651–61.
Genevier HC, Hinshelwood S, Gaspar HB, Rigley KP, Brown D, Saeland S, et al. Expression of Bruton’s tyrosine kinase protein within the B cell lineage. Eur J Immunol. 1994;24:3100–5.
Munakata W, Tobinai K. Tirabrutinib hydrochloride for B-cell lymphomas. Drugs Today (Barc). 2021;57:277–89.
Janssen/Pharmacyclics LLC. IMBRUVICA® (ibrutinib) capsules 140 mg. Interview form, Sep 2021, 10th Edition. Available at: https://mc-e2ce8b00-afab-4ff9-ae22-349570-cdn-endpoint.azureedge.net/-/media/Project/Janssen/Japan/Product/ibr/pdf/ibr_if.pdf?rev=5ec3a5e966354607a1e0042785112f2c&download=1. Accessed Mar 1, 2022 (in Japanese).
Danilov AV, Herbaux C, Walter HS, Hillmen P, Rule SA, Kio EA, et al. Phase Ib study of tirabrutinib in combination with idelalisib or entospletinib in previously treated chronic lymphocytic leukemia. Clin Cancer Res. 2020;26:2810–8.
Munakata W, Ando K, Hatake K, Fukuhara N, Kinoshita T, Fukuhara S, et al. Phase I study of tirabrutinib (ONO-4059/GS-4059) in patients with relapsed or refractory B-cell malignancies in Japan. Cancer Sci. 2019;110:1686–94.
Narita Y, Nagane M, Mishima K, Terui Y, Arakawa Y, Yonezawa H, et al. Phase I/II study of tirabrutinib, a second-generation Bruton’s tyrosine kinase inhibitor, in relapsed/refractory primary central nervous system lymphoma. Neuro Oncol. 2021;23:122–33.
Rule SA, Cartron G, Fegan C, Morschhauser F, Han L, Mitra S, et al. Long-term follow-up of patients with mantle cell lymphoma (MCL) treated with the selective Bruton’s tyrosine kinase inhibitor tirabrutinib (GS/ONO-4059). Leukemia. 2020;34:1458–61.
Sekiguchi N, Rai S, Munakata W, Suzuki K, Handa H, Shibayama H, et al. A multicenter, open-label, phase II study of tirabrutinib (ONO/GS-4059) in patients with Waldenström’s macroglobulinemia. Cancer Sci. 2020;111:3327–37.
Walter HS, Jayne S, Rule SA, Cartron G, Morschhauser F, Macip S, et al. Long-term follow-up of patients with CLL treated with the selective Bruton’s tyrosine kinase inhibitor ONO/GS-4059. Blood. 2017;129:2808–10.
Walter HS, Rule SA, Dyer MJ, Karlin L, Jones C, Cazin B, et al. A phase 1 clinical trial of the selective BTK inhibitor ONO/GS-4059 in relapsed and refractory mature B-cell malignancies. Blood. 2016;127:411–9.
Byrd JC, Furman RR, Coutre SE, Flinn IW, Burger JA, Blum KA, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369:32–42.
Wang ML, Rule S, Martin P, Goy A, Auer R, Kahl BS, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2013;369:507–16.
ONO Pharmaceutical Co., Ltd. VELEXBRU® (tirabrutinib) tablets 80 mg. Interview form, revised Feb 2022, 5th Edition. Available at: https://www.ono-oncology.jp/medical/products/velexbru/drug-info. Accessed Mar 1, 2021 (in Japanese).
ONO Pharmaceutical Co., Ltd. Velexbru® Tablet 80 mg, a BTK inhibitor, approved in South Korea for treatment of recurrent or refractory B-cell primary central nervous system lymphoma. Press release, Nov 8, 2021. Available at: https://www.ono-pharma.com/news/20211108.html. Accessed Mar 1, 2021.
Velexbru® Tablet 80 mg, a BTK inhibitor, approved in Taiwan for the treatment of recurrent or refractory B-cell primary central nervous system lymphoma. Press release, Feb 21, 2022. Available at: https://www.ono-pharma.com/news/20220221.html. Accessed Mar 1, 2022.
Lasica M, Tam CS. Management of ibrutinib toxicities: a practical guide. Curr Hematol Malig Rep. 2020;15:177–86.
Maddocks KJ, Ruppert AS, Lozanski G, Heerema NA, Zhao W, Abruzzo L, et al. Etiology of ibrutinib therapy discontinuation and outcomes in patients with chronic lymphocytic leukemia. JAMA Oncol. 2015;1:80–7.
Mato AR, Nabhan C, Thompson MC, Lamanna N, Brander DM, Hill B, et al. Toxicities and outcomes of 616 ibrutinib-treated patients in the United States: a real-world analysis. Haematologica. 2018;103:874–9.
Owen C, Berinstein NL, Christofides A, Sehn LH. Review of Bruton tyrosine kinase inhibitors for the treatment of relapsed or refractory mantle cell lymphoma. Curr Oncol. 2019;26:e233–40.
Tam CSL, Opat S, D’Sa S, Jurczak W, Lee H-P, Cull G, et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenström macroglobulinemia: the ASPEN study. Blood. 2020;136:2038–50.
Wang ML, Blum KA, Martin P, Goy A, Auer R, Kahl BS, et al. Long-term follow-up of MCL patients treated with single-agent ibrutinib: updated safety and efficacy results. Blood. 2015;126:739–45.
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI sponsored international working group. J Clin Oncol. 1999;17:1244.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the international workshop on chronic lymphocytic leukemia updating the National Cancer Institute-working group 1996 guidelines. Blood. 2008;111:5446–56.
Owen RG, Kyle RA, Stone MJ, Rawstron AC, Leblond V, Merlini G, et al. Response assessment in Waldenström macroglobulinaemia: update from the 6th international workshop. Br J Haematol. 2013;160:171–6.
Byrd JC, Hillmen P, O’Brien S, Flinn IW, Burger JA, Blum KA, et al. Long-term follow-up of the RESONATE phase 3 trial of ibrutinib vs ofatumumab. Blood. 2019;133:2031–42.
Archibald WJ, Rabe KG, Kabat BF, Herrmann J, Ding W, Kay NE, et al. Atrial fibrillation in patients with chronic lymphocytic leukemia (CLL) treated with ibrutinib: risk prediction, management, and clinical outcomes. Ann Hematol. 2021;100:143–55.
Caldeira D, Alves D, Costa J, Ferreira JJ, Pinto FJ. Ibrutinib increases the risk of hypertension and atrial fibrillation: Systematic review and meta-analysis. PLoS ONE. 2019;14:e0211228.
Roeker LE, Sarraf Yazdy M, Rhodes J, Goodfriend J, Narkhede M, Carver J, et al. Hypertension in patients treated with ibrutinib for chronic lymphocytic leukemia. JAMA Netw Open. 2019;2:e1916326.
Salem JE, Manouchehri A, Bretagne M, Lebrun-Vignes B, Groarke JD, Johnson DB, et al. Cardiovascular toxicities associated with ibrutinib. J Am Coll Cardiol. 2019;74:1667–78.
Abbas HA, Wierda WG. Acalabrutinib: a selective Bruton tyrosine kinase inhibitor for the treatment of B-cell malignancies. Front Oncol. 2021;11:668162.
Estupiñán HY, Berglöf A, Zain R, Smith CIE. Comparative analysis of BTK inhibitors and mechanisms underlying adverse effects. Front Cell Dev Biol. 2021;9:630942.
Izutsu K, Ando K, Ennishi D, Shibayama H, Suzumiya J, Yamamoto K, et al. Safety and antitumor activity of acalabrutinib for relapsed/refractory B-cell malignancies: a Japanese phase I study. Cancer Sci. 2021;112:2405–15.
Awan FT, Schuh A, Brown JR, Furman RR, Pagel JM, Hillmen P, et al. Acalabrutinib monotherapy in patients with chronic lymphocytic leukemia who are intolerant to ibrutinib. Blood Adv. 2019;3:1553–62.
Sun C, Nierman P, Kendall EK, Cheung J, Gulrajani M, Herman SEM, et al. Clinical and biological implications of target occupancy in CLL treated with the BTK inhibitor acalabrutinib. Blood. 2020;136:93–105.
Song Y, Zhou K, Zou D, Zhou J, Hu J, Yang H, et al. Treatment of patients with relapsed or refractory mantle-cell lymphoma with zanubrutinib, a selective inhibitor of Bruton’s tyrosine kinase. Clin Cancer Res. 2020;26:4216–24.
Acknowledgements
This study was funded by Ono Pharmaceutical Co., Ltd. The authors are grateful for the patients, investigators, and staff at Tohoku University Graduate School of Medicine, Cancer Institute Hospital, National Cancer Center Hospital, Tokai University, and Aichi Cancer Center for the contributions to this study. The authors thank the members of the Efficacy and Safety Monitoring Committee: Kazuo Tamura (General Medical Research Center, Fukuoka University, Fukuoka), Kunihiro Tsukasaki (International Medical Center, Saitama Medical University, Saitama), and Hirokazu Nagai (Nagoya Medical Center, Nagoya). The authors also thank Nicholas D. Smith (EMC K.K.) for medical writing support, which was funded by Ono Pharmaceutical Co., Ltd.
Funding
This study was funded by Ono Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Wataru Munakata reports research funds from Ono Pharmaceutical Co., Ltd. Kiyoshi Ando reports research funds from Celgene K.K., Novartis Pharma K.K., and Astellas Pharma Inc.; and scholarship endowments from Chugai Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Kyowa Kirin Co., Ltd. Masahiro Yokoyama reports acting as a medical adviser for Chugai Pharmaceutical Co., Ltd. Noriko Fukuhara reports lecture fees, honoraria, or other personal fees from SymBio Pharmaceuticals Ltd., Chugai Pharmaceutical Co., Ltd., and HUYA Bioscience International LLC; and research funds from Incyte Japan, Genmab K.K., Celgene K.K., Chugai Pharmaceutical Co., Ltd., and Bayer Yakuhin, Ltd. Kazuhito Yamamoto reports lecture fees, honoraria, or other personal fees from AbbVie GK, Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Meiji Seika Pharma Co., Ltd., Micron Inc., and Takeda Pharmaceutical Co., Ltd.; and research funds from Symbio Pharmaceuticals Ltd. and Yakult Honsha Co., Ltd. Suguru Fukuhara reports research funds from Chugai Pharmaceutical Co., Ltd. Ken Ohmachi has nothing to report. Yuko Mishima reports holding shares or share options in Chugai Pharmaceutical Co., Ltd.; and research funds from Takeda Pharmaceutical Co., Ltd., Bristol-Myers Squibb K.K., Eisai Co., Ltd., Kyowa Kirin Co., Ltd., and Taiho Pharmaceutical Co., Ltd. Satoshi Ichikawa reports research funds from AstraZeneca K.K. and BeiGene Japan. Daisuke Ogiya has nothing to report. Arata Aoi is an employee of Ono Pharma USA, Inc. Masahiro Hatsumichi is an employee of Ono Pharmaceutical Co., Ltd. Kensei Tobinai reports lecture fees, honoraria, or other personal fees from Zenyaku Kogyo Co., Ltd., HUYA Bioscience International LLC, Daiichi Sankyo Co., Ltd., and SymBio Pharmaceutical Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Munakata, W., Ando, K., Yokoyama, M. et al. Long-term safety profile of tirabrutinib: final results of a Japanese Phase I study in patients with relapsed or refractory B-cell malignancies. Int J Hematol 117, 553–562 (2023). https://doi.org/10.1007/s12185-022-03514-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03514-6