Abstract
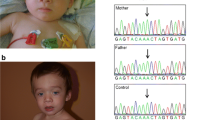
Shwachman–Diamond syndrome (SDS) is an autosomal recessive inherited disorder characterized by bone marrow failure, exocrine pancreatic dysfunction, and skeletal abnormalities. SDS is typically caused by a pathogenic mutation in the Shwachman–Bodian–Diamond Syndrome (SBDS) gene. Patients with SDS have an increased risk of developing acute myeloid leukemia (AML) and myelodysplastic syndromes. We identified germline biallelic SBDS mutations (p.K62X and p.I167M) in a 50-year-old AML patient who had never experienced the typical symptoms of SDS. The K62X mutation is one of the most common pathogenic mutations, whereas the significance of the I167M mutation was unclear. Based on cellular experiments, we concluded that the I167M mutation contributed to the development of AML, and chemotherapy including topoisomerase inhibitors, which induce DNA double-strand breaks, may have been toxic to this patient. Our experience indicates that some asymptomatic Shwachman–Bodian–Diamond syndrome mutations contribute to the development of leukemia, and that careful treatment selection may be warranted for patients harboring these mutations.



Similar content being viewed by others
References
Burroughs L, Woolfrey A, Shimamura A. Shwachman–Diamond syndrome: a review of the clinical presentation, molecular pathogenesis, diagnosis, and treatment. Hematol Oncol Clin North Am. 2009;23:233–48.
Ohtake S, Miyawaki S, Fujita H, Kiyoi H, Shinagawa K, Usui N, et al. Randomized study of induction therapy comparing standard-dose idarubicin with high-dose daunorubicin in adult patients with previously untreated acute myeloid leukemia: the JALSG AML201 Study. Blood. 2011;117:2358–65.
Kohrt HE, Patel S, Ho M, Owen T, Pollyea DA, Majeti R, et al. Second-line mitoxantrone, etoposide, and cytarabine for acute myeloid leukemia: a single-center experience. Am J Hematol. 2010;85:877–81.
Yamamoto H, Uchida N, Yuasa M, Kageyama K, Ota H, Kaji D, et al. A Novel reduced-toxicity myeloablative conditioning regimen using full-dose busulfan, fludarabine, and melphalan for single cord blood transplantation provides durable engraftment and remission in nonremission myeloid malignancies. Biol Blood Marrow Transplant. 2016;22:1844–50.
Szmit Z, Gorczynska E, Król A, Ussowicz M, Mielcarek-Siedziuk M, Olejnik I, et al. Introduction of new pediatric EBMT criteria for VOD diagnosis: is it time-saving or money-wasting?: prospective evaluation of pediatric EBMT criteria for VOD. Bone Marrow Transplant. 2020;55:2138–46.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28:241–7.
Elghetany MT, Alter BP. p53 protein overexpression in bone marrow biopsies of patients with Shwachman–Diamond syndrome has a prevalence similar to that of patients with refractory anemia. Arch Pathol Lab Med. 2002;126:452–5.
Tourlakis ME, Zhang S, Ball HL, Gandhi R, Liu H, Zhong J, et al. In vivo senescence in the Sbds-deficient murine pancreas: cell-type specific consequences of translation insufficiency. PLoS Genet. 2015;11:e1005288.
Lindsley RC, Saber W, Mar BG, Redd R, Wang T, Haagenson MD, et al. Prognostic mutations in myelodysplastic syndrome after stem-cell transplantation. N Engl J Med. 2017;376:536–47.
Xia J, Miller CA, Baty J, Ramesh A, Jotte MRM, Fulton RS, et al. Somatic mutations and clonal hematopoiesis in congenital neutropenia. Blood. 2018;131:408–16.
Shammas C, Menne TF, Hilcenko C, Michell SR, Goyenechea B, Boocock GR, et al. Structural and mutational analysis of the SBDS protein family. Insight into the leukemia-associated Shwachman–Diamond syndrome. J Biol Chem. 2005;280:19221–9.
Boocock GR, Morrison JA, Popovic M, Richards N, Ellis L, Durie PR, et al. Mutations in SBDS are associated with Shwachman–Diamond syndrome. Nat Genet. 2003;33:97–101.
Nakashima E, Mabuchi A, Makita Y, Masuno M, Ohashi H, Nishimura G, et al. Novel SBDS mutations caused by gene conversion in Japanese patients with Shwachman–Diamond syndrome. Hum Genet. 2004;114:345–8.
Myers K, Hebert K, Antin J, Boulad F, Burroughs L, Hofmann I, et al. Hematopoietic stem cell transplantation for Shwachman–Diamond syndrome. Biol Blood Marrow Transplant. 2020;26:1446–51.
Myers KC, Furutani E, Weller E, Siegele B, Galvin A, Arsenault V, et al. Clinical features and outcomes of patients with Shwachman–Diamond syndrome and myelodysplastic syndrome or acute myeloid leukaemia: a multicentre, retrospective, cohort study. Lancet Haematol. 2020;7:e238–46.
Asik E, Chatterjee N, Bertuch AA. Homologous recombination defects in Shwachman–Diamond syndrome and Diamond-Blackfan anemia. Biorxiv. 2020. https://doi.org/10.1101/2020.08.13.250068.
Anno K, Hayashi A, Takahashi T, Mitsui Y, Ide T, Tahara H, et al. Telomerase activation induces elongation of the telomeric single-stranded overhang, but does not prevent chromosome aberrations in human vascular endothelial cells. Biochem Biophys Res Commun. 2007;353:926–32.
Yoon JH, Min GJ, Park SS, Park S, Lee SE, Cho BS, et al. Incidence and risk factors of hepatic veno-occlusive disease/sinusoidal obstruction syndrome after allogeneic hematopoietic cell transplantation in adults with prophylactic ursodiol and intravenous heparin or prostaglandin E1. Bone Marrow Transplant. 2021;56:1603–13.
Acknowledgements
The authors are grateful to Y. Katsuki and M. Takata in Radiation Biology Center of Kyoto University for their help in experiments requiring γ-ray irradiation.
Funding
This work was supported by Ministry of Education, Culture, Sports, Science and Technology under Grant Number hp160219 and JP20cm0106501h0005 to SO.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shibata, S., Inano, S., Watanabe, M. et al. Identification of an asymptomatic Shwachman–Bodian–Diamond syndrome mutation in a patient with acute myeloid leukemia. Int J Hematol 115, 428–434 (2022). https://doi.org/10.1007/s12185-021-03251-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-021-03251-2