Abstract
Purpose of Review
This review discusses the current literature regarding the use of platelet-rich plasma (PRP) in the treatment of muscle strain injuries. Case series as well as experimental trials for both human and animal models are covered.
Recent Findings
Multiple studies have examined outcomes for the use of PRP in the treatment of muscle strain injuries. PRP has been shown to promote muscle recovery via anabolic growth factors released from activated platelets, and in doing so, potentially reduces pain, swelling, and time for return to play.
Summary
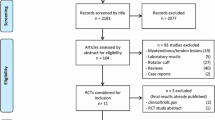
In vitro studies support the regenerative potential of PRP for acute soft tissue injuries. Multiple clinical case series for PRP injections in the setting of muscle strains demonstrate imaging evidence for faster healing, less swelling, which can decrease time for return to play. These studies, however, are retrospective in nature, and few randomized controlled studies exist to demonstrate a clear clinical benefit. Additionally, there is tremendous heterogeneity regarding the injectant preparation, optimum platelet concentration, presence of leukocytes, and volume of PRP which should be administered as well as number of and timing of treatments.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Rossi LA, Romoli ARM, Altieri BAB, Flor JAB, Scordo WE, Elizondo CM. Does Platelet-rich plasma decrease time to return to sports in acute muscle tear? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:3319–25. The authors of this study looked to report the effects of autologous PRP injections and its effect on the return to play and recurrence rate after grade 2 muscle injuries in recreational and competitive athletes. Primary outcome was the mean return to play and secondary outcomes included changes in VAS scores as well as recurrence rate. A total of 75 patients were randomized into one of two groups: PRP injection with rehabilitation and rehabilitation alone. Excluding patients lost to follow-up, a total of 72 patients were included in the study; 34 in the treatment group and 38 in the control group. Mean time to play was 21.1 days for the PRP group and 25 days for the control group which they found to be significant. Subgroup analysis revealed there was no difference in return to play as far as muscle groups between hamstrings, gastrocnemius, and quadriceps. VAS scores were lower at all time points with the treatment group compared to controls. Additionally, two of the 35 initially treated in the PRP group had recurrence of muscle strain (5.7%) versus 4 of 40 in the control group (10%) but was not found to be statistically significant. This study ultimately showed that a single injection of autologous PRP with a rehabilitation program significantly shortened time to return to sports after and acute grade 2 muscle injury when compared with control group; however, the rate of recurrence was not significant between the two groups.
Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183(4):975–84.
Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41(12):2933–47.
Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42(3):209–26.
Woods C, Hawkins R, Hulse M, Hodson A. The football association medical research program: an audit of injuries in professional football-analysis of preseason injuries. Br J Sports Med. 2002;36(6):436–41.
Verrall GM, Kalairajah Y, Slavotinek JP, Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1–2):87–90.
Hussain N, Herman J, Bhandari M. An evidence-based evaluation on the use of platelet rich plasma in orthopedics – a review of the literature. SICOT J. 2017;3:57.
Yan R, Gu Y, Ran J, Hu Y, Zheng Z, Zeng M, et al. Intratendon delivery of leukocyte-poor platelet-rich plasma improves healing compared with leukocyte-rich platelet-rich plasma in a rabbit Achilles tendinopathy model. Am J Sports Med. 2017;45(8):1909–20.
Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42:463–71.
Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610–8.
Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of high-volume injection, platelet-rich plasma, and sham treatment in chronic midportion Achilles tendinopathy: a randomized double-blinded prospective study. Am J Sports Med. 2017;45:2034–43.
Rha D, Park G-Y, Kim Y-K, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013;27:113–22.
Yang W-Y, Han Y-H, Cao X-W, Pan J-K, Zeng L-F, Lin J-T, et al. Platelet-rich plasma as a treatment for plantar fasciitis: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2017;96:e8475.
Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg. 2017;12(1):1–12.
Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med. 2016;44:792–800.
Saltzman BM, Jain A, Campbell KA, Mascarenhas R, Romeo AA, Verma NN, et al. Does the use of platelet-rich plasma at the time of surgery improve clinical outcomes in arthroscopic rotator cuff repair when compared with control cohorts? A systematic review of meta-analyses. Arthrosc J Arthrosc Relat Surg. 2016;32:906–18.
Filardo G, Di Matteo B, Kon E, Merli G, Marcacci M. Platelet-rich plasma in tendon-related disorders: results and indications. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1984–99.
De Carli A, Lanzetti RM, Ciompi A, Lupariello D, Vadala A, Argento G, et al. Can platelet-rich plasma have a role in Achilles tendon surgical repair? Knee Surg Sports Traumatol Arthrosc. 2016;24:2231–7.
Mirzatolooei F, Alamdari MT, Khalkhali HR. The impact of platelet-rich plasma on the prevention of tunnel widening in anterior cruciate ligament reconstruction using quadrupled autologous hamstring tendon. Bone Joint J. 2013;95-B:65–9.
Guzel Y, Karalezli N, Bilge O, Kacira BK, Esen H, Karadag H, et al. The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg Sports Traumatol Arthrosc. 2015;23:1378–83.
Cole BJ, Seroyer ST, Filardo G, Bajaj S, Fortier LA. Platelet-rich plasma: where are we now and where are we going. Sports Health. 2010;2(3):203–10.
Borrione P, Fossati C, Pereira MT, Giannini S, Davico M, Minganti C, et al. The use of platelet-rich plasma (PRP) in the treatment of gastrocnemius strains: a retrospective observational study. Platelets. 2018;29(6):596–601.
Terada S, Ota S, Kobayashi T, Mifune Y, Takayama K, Witt M, et al. Use of an antifibrotic agent improves the effect of platelet-rich plasma on muscle healing after injury. J Bone Joint Surg Am. 2013;95(11):980–8.
Tsai WC, Yu TY, Lin LP, Lin MS, Wu YC, Liao CH, et al. Platelet rich plasma releasate promoted proliferation of skeletal muscle cells in association with upregulation of PCNA, cyclins, and cyclin dependent kinases. Platelets. 2017;28(5):491–7.
Hammond JW, Hinton RY, Curl LA, Muriel JM, Loverin RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37(6):1135–42.
Wright-Carpenter T, Opolon P, Appell HJ, Meijer H, Wehling P, Mir LM. Treatment of muscle injuries by local administration of autologous conditioned serum: animal experiments using a muscle contusion model. Int J Sports Med. 2004;25(8):582–7.
Tsai WC, Yu TY, Chang GJ, Lin LP, Lin MS, Pang JS. Platelet-rich plasma releasate promotes regeneration and decreases inflammation and apoptosis of injured skeletal muscle. Am J Sports Med. 2018;46(8):1980–6.
De Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR. 2009;192(6):1701–7.
Warden SJ, Kiss ZS, Malara FA. Comparative accuracy of magnetic resonance imaging and ultrasonography in confirming clinically diagnosed patellar tendinopathy. Am J Sports Med. 2007;35(3):427–36.
Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35(2):197–206.
Koulouris G, Connell D. Imaging of hamstring injuries: therapeutic implications. Eur Radiol. 2006;16:1478–87.
Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31(6):969–73.
Bubnov R, Yevseenko V, Semeniv I. Ultrasound guided injections of platelets rich in plasma for muscle injury in professional athletes: comparative study. Med Ultrasound. 2013;15(2):101–5.
Hamilton B, Knez W, Eirale C, Chalabi H. Platelet enriched plasma for acute muscle injury. Acta Orthop Belg. 2010;76(4):443–8.
Zanon G, Combi F, Combi A, Perticarini L, Sammarchi L, Benazzo F. Platelet-rich plasma in the treatment of acute hamstring injuries in professional football players. Joints. 2016;4(1):17–23.
Wright-Carpenter T, Klein P, Schaferhoff P, Appell HK, Mir LM, Wehling P. Treatment of muscle injuries by local administration of autologous conditioned serum: a pilot study on sportsmen with muscle strains. Int J Sports Med. 2004;25:588–93.
Delos D, Maak TG, Rodeo SA. Muscle injuries in athletes: enhancing recovery through scientific understanding and novel therapies. Sports Health. 2013;5(4):346–52.
Hamid MSA, Ali MRMA, Yusof A, Lee LPC. Platelet-rich plasma injections for the treatment of hamstring injections. Am J Sports Med. 2014;42(10):2410–8.
Mejia HA, Bradley JP. The effects of platelet-rich plasma on muscle: basic science and clinical application. Oper Tech Sports Med. 2011;19:149–53.
• Sheth U, Dwyer T, Smith I, Wasserstein D, Theodoropoulos J, Takhar S, et al. Does platelet-rich plasma lead to earlier return to sport when compared with conservative treatment in acute muscle injuries? a systematic review and meta-analysis. Arthroscopy. 2018;34(1):281–8. This study aimed to compare the time to return to sport and reinjury rate after PRP injection versus control in patients with acute grade I or II muscle strains. The primary outcome was time to return to play while the secondary outcome was the rate of reinjury at a minimum of 6 months. Subgroup analysis was performed to examine efficacy of PRP in hamstring muscle strain individually. Five randomized controlled trials which included a total of 268 patients with grade I and II acute muscle injuries were eligible review. Two-hundred twenty-two of 268 patients were reported to be competitive athletes. Two studies described PRP usage with the GPSIII system (Biomet Biologics), whereas one study used the autologous conditioned plasma (Arthrex), and the remaining two studies did not report which system was used. Platelet concentration ranged from 443 to 1297 × 10 3 /μL and there was considerable variability in injection protocols, ranging from a single 3-mL injection to 5-mL injection to a multiple 3-mL injection protocol. Control groups were treated with a daily home exercise program with progressive agility and trunk stabilization in conjunction with 1, 2, or 3 physiotherapy sessions, while one study had a control group with blinded placebo (normal saline) injection. The pooled results demonstrated a significantly earlier return to sport for the PRP group when compared to control with a mean difference of 5.57 days earlier return to play with PRP. Subgroup analysis showed no difference in time to return to sport when comparing PRP and control for treatment of grade I and II hamstring muscle strains alone. No significant reinjury rate was found between two groups at a 6-month follow-up. The study suggested that the use of PRP for acute grade I and II muscle strains may result in faster return to sport without increasing the rate of reinjury; however, no difference was noted in time to return to sport looking at acute grade I and II hamstring strains specifically.
Mosca M, Rodeo S. Platelet rich plasma for muscle injuries: game over or time out? Curr Rev Musculoskelet Med. 2015;8:145–53.
• Hamilton B, Tol JL, Almusa E, Boukarroum S, Eirale C, Farooq A, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomized controlled trial. Br J Sports Med. 2015;49:943–50. This study looked at the efficacy of a single PRP injection in reducing the return to sport duration in male athletes after acute hamstring injury. The study is a randomized, three-arm, double-blind, parallel-group trial including 90 professional athletes with hamstring injuries confirmed on MRI. Patients were randomized to PRP, PPP (platelet-poor plasma) or control (no injection) groups. All patients received intensive standardized rehabilitation and the primary outcome measure was return to play, with secondary outcome measures including reinjury rate after 2 and 6 months. The adjusted time to return to sport was − 5.7 days between PRP and PPP which was significant ( p = 0.01); however, the adjusted time to return to sport between PRP and control was − 2.9 days, which was not significant ( p = 0.189). The time to return to sport between PPP and control was 2.8 days, which was not significant ( p = 0.210). There was no difference in reinjury rate between any groups. In conclusion, this study found that there was no benefit of a single PRP injection over rehabilitation program in athletes who have sustained acute MRI positive hamstring injuries.
Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):1–5.
• Grassi A, Napoli F, Romandini I, Samuelsson K, Zaffagnini S, Candrian C, et al. Platelet-rich plasma (PRP) effective in the treatment of acute muscle injuries? a systematic review and meta-analysis. Sports Med. 2018;48(4):971–89. This study was a meta-analysis of randomized controlled trials looking to evaluate the effect of PRP injections on outcomes following acute muscle injuries. They included randomized controlled trials which investigated the effect of PRP for the treatment of acute muscle injuries against at least one control group, encompassing placebo injection or physical therapy. The outcomes evaluated were time to return to sport, reinjuries, complications, pain, muscle strength, range of motion and flexibility, muscle function, and imaging. Six studies were included with a total of 374 patients. Time to return to sport was significantly shorter in patients treated with PRP (mean difference − 7.17 days), but if only double-blind studies or studies or studies involving only hamstring injuries were analyzed, non-significant differences were found. The rate of reinjury and complications was similar between the two groups ( p > 0.05), nor was any differences in pain, muscle strength, flexibility muscle function, and imaging. The authors did note that the performance bias was a high risk due to lack of blinding in four studies. Due to the bias in the studies, heterogeneity of the findings, and limited sample size, the authors found that the evidence should be considered a low quality despite promising biological rationale, positive preclinical findings, and early successful clinical experience of PRP.
Reurink G, Goudswaard GJ, Moen MH, Weir A, Verhaar JAN, Bierma-Zeinstra SMA, et al. Platelet-rich plasma injections in acute muscle injury. N Engl J Med. 2014;370(26):2546–7.
Loo W, Lee D, Soon M. Plasma rich in growth factors to treat adductor longus tear. Ann Acad Med. 2009;38:733–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Protein-Rich Plasma: From Bench to Treatment of Arthritis
Rights and permissions
About this article
Cite this article
Setayesh, K., Villarreal, A., Gottschalk, A. et al. Treatment of Muscle Injuries with Platelet-Rich Plasma: a Review of the Literature. Curr Rev Musculoskelet Med 11, 635–642 (2018). https://doi.org/10.1007/s12178-018-9526-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-018-9526-8