Abstract
Objective
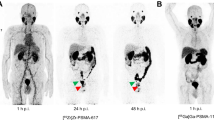
The aims of this study were to investigate the utility of [18F]F-Florastamin, a novel prostate-specific membrane antigen (PSMA)-targeted PET radiotracer with facile radiochemistry, relative to the conventional imaging for the detection of sties of disease and evaluate the effect of multi-timepoint imaging with [18F]F-Florastamin PET on lesion detectability.
Methods
Eight prostate cancer patients with known or suspected recurrence who underwent [18F]F-Florastamin PET/CT at 1-h and 2-h imaging time-points were included in this prospective pilot study. [18F]F-Florastamin PET images were interpreted visually and quantitatively at both time points and compared with CIM.
Results
[18F]F-Florastamin PET was superior to CT in the detection of active osseous metastases and small-sized metastatic lymph nodes that do not fall under the anatomic imaging size criteria for metastasis. Multi-timepoint imaging showed a significant reduction in the blood pool, bone marrow and muscular uptake, and increase in liver uptake over time. There is a significant improvement in tumor-to-background ratio (TBR) at the 2-h imaging time-point (P = 0.04). The mean percentage change in TBR at 2-h was 21% (SD = 0.31).
Conclusions
[18F]F-Florastamin is a promising new radioligand for PSMA-targeted PET with suitable lesion detectability and high TBR at both time points.



Similar content being viewed by others
References
Rowe SP, Gorin MA, Pomper MG. Imaging of prostate-specific membrane antigen with small-molecule PET radiotracers: from the bench to advanced clinical applications. Annu Rev Med. 2019;70:461–77. https://doi.org/10.1146/annurev-med-062117-073027.
Rowe SP, Buck A, Bundschuh RA, Lapa C, Serfling SE, Derlin T, et al. [18F]DCFPyL PET/CT for imaging of prostate cancer. Nuklearmedizin. 2022;61:240–6. https://doi.org/10.1055/a-1659-0010.
Afshar-Oromieh A, Haberkorn U, Eder M, Eisenhut M, Zechmann CM. [68Ga]Gallium-labelled PSMA ligand as superior PET tracer for the diagnosis of prostate cancer: comparison with 18F-FECH. Eur J Nucl Med Mol Imaging. 2012;39:1085–6. https://doi.org/10.1007/s00259-012-2069-0.
Sanchez-Crespo A. Comparison of Gallium-68 and Fluorine-18 imaging characteristics in positron emission tomography. Appl Radiat Isot. 2013;76:55–62. https://doi.org/10.1016/j.apradiso.2012.06.034.
Gorin MA, Pomper MG, Rowe SP. PSMA-targeted imaging of prostate cancer: the best is yet to come. BJU Int. 2016;117:715–6. https://doi.org/10.1111/bju.13435.
Dietlein M, Kobe C, Kuhnert G, Stockter S, Fischer T, Schomacker K, et al. Comparison of [(18)F]DCFPyL and [(68)Ga]Ga-PSMA-HBED-CC for PSMA-PET imaging in patients with relapsed prostate cancer. Mol Imaging Biol. 2015;17:575–84. https://doi.org/10.1007/s11307-015-0866-0.
Kuten J, Fahoum I, Savin Z, Shamni O, Gitstein G, Hershkovitz D, et al. Head-to-head comparison of (68)Ga-PSMA-11 with (18)F-PSMA-1007 PET/CT in staging prostate cancer using histopathology and immunohistochemical analysis as a reference standard. J Nucl Med. 2020;61:527–32. https://doi.org/10.2967/jnumed.119.234187.
Werner RA, Derlin T, Lapa C, Sheikbahaei S, Higuchi T, Giesel FL, et al. (18)F-Labeled, PSMA-targeted radiotracers: leveraging the advantages of radiofluorination for prostate cancer molecular imaging. Theranostics. 2020;10:1–16. https://doi.org/10.7150/thno.37894.
Giesel FL, Cardinale J, Schafer M, Neels O, Benesova M, Mier W, et al. (18)F-Labelled PSMA-1007 shows similarity in structure, biodistribution and tumour uptake to the theragnostic compound PSMA-617. Eur J Nucl Med Mol Imaging. 2016;43:1929–30. https://doi.org/10.1007/s00259-016-3447-9.
Dietlein F, Kobe C, Hohberg M, Zlatopolskiy BD, Krapf P, Endepols H, et al. Intraindividual comparison of (18)F-PSMA-1007 with renally excreted PSMA ligands for PSMA PET imaging in patients with relapsed prostate cancer. J Nucl Med. 2020;61:729–34. https://doi.org/10.2967/jnumed.119.234898.
Lee I, Lim I, Byun BH, Kim BI, Choi CW, Woo SK, et al. A microdose clinical trial to evaluate [(18)F]Florastamin as a positron emission tomography imaging agent in patients with prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48:95–102. https://doi.org/10.1007/s00259-020-04883-y.
Sahakyan K, Li X, Lodge MA, Werner RA, Bundschuh RA, Bundschuh L, et al. Semiquantitative parameters in PSMA-targeted PET imaging with [(18)F]DCFPyL: intrapatient and interpatient variability of normal organ uptake. Mol Imaging Biol. 2020;22:181–9. https://doi.org/10.1007/s11307-019-01376-9.
Hoffmann MA, Buchholz HG, Wieler HJ, Rosar F, Miederer M, Fischer N, et al. Dual-time point [(68)Ga]Ga-PSMA-11 PET/CT hybrid imaging for staging and restaging of prostate cancer. Cancers (Basel). 2020. https://doi.org/10.3390/cancers12102788.
Rowe SP, Macura KJ, Mena E, Blackford AL, Nadal R, Antonarakis ES, et al. PSMA-based [(18)F]DCFPyL PET/CT is superior to conventional imaging for lesion detection in patients with metastatic prostate cancer. Mol Imaging Biol. 2016;18:411–9. https://doi.org/10.1007/s11307-016-0957-6.
Alberts I, Prenosil G, Mingels C, Bohn KP, Viscione M, Sari H, et al. Feasibility of late acquisition [68Ga]Ga-PSMA-11 PET/CT using a long axial field-of-view PET/CT scanner for the diagnosis of recurrent prostate cancer-first clinical experiences. Eur J Nucl Med Mol Imaging. 2021;48:4456–62. https://doi.org/10.1007/s00259-021-05438-5.
Hohberg M, Kobe C, Tager P, Hammes J, Schmidt M, Dietlein F, et al. Combined early and late [(68)Ga]PSMA-HBED-CC PET scans improve lesion detectability in biochemical recurrence of prostate cancer with low PSA levels. Mol Imaging Biol. 2019;21:558–66. https://doi.org/10.1007/s11307-018-1263-2.
Szabo Z, Mena E, Rowe SP, Plyku D, Nidal R, Eisenberger MA, et al. Initial evaluation of [(18)F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol. 2015;17:565–74. https://doi.org/10.1007/s11307-015-0850-8.
Alberts I, Sachpekidis C, Dijkstra L, Prenosil G, Gourni E, Boxler S, et al. The role of additional late PSMA-ligand PET/CT in the differentiation between lymph node metastases and ganglia. Eur J Nucl Med Mol Imaging. 2020;47:642–51. https://doi.org/10.1007/s00259-019-04552-9.
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2017;44:678–88. https://doi.org/10.1007/s00259-016-3573-4.
Afshar-Oromieh A, Sattler LP, Mier W, Hadaschik BA, Debus J, Holland-Letz T, et al. The clinical impact of additional late PET/CT imaging with (68)Ga-PSMA-11 (HBED-CC) in the diagnosis of prostate cancer. J Nucl Med. 2017;58:750–5. https://doi.org/10.2967/jnumed.116.183483.
Derlin T, Weiberg D, von Klot C, Wester HJ, Henkenberens C, Ross TL, et al. (68)Ga-PSMA I&T PET/CT for assessment of prostate cancer: evaluation of image quality after forced diuresis and delayed imaging. Eur Radiol. 2016;26:4345–53. https://doi.org/10.1007/s00330-016-4308-4.
Chen Y, Lisok A, Chatterjee S, Wharram B, Pullambhatla M, Wang Y, et al. [(18)F]Fluoroethyl triazole substituted PSMA inhibitor exhibiting rapid normal organ clearance. Bioconjug Chem. 2016;27:1655–62. https://doi.org/10.1021/acs.bioconjchem.6b00195.
Funding
We acknowledge funding for this study from FutureChem Co, Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MGP has equity in FutureChem USA, a subsidiary of FutureChem Co, Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sheikhbahaei, S., Bello Martinez, R., Markowski, M.C. et al. Multi-timepoint imaging with PSMA-targeted [18F]F-Florastamin PET/CT: lesion detection and comparison to conventional imaging. Ann Nucl Med 37, 246–254 (2023). https://doi.org/10.1007/s12149-023-01823-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-023-01823-2