Abstract
Objectives
The aim of this study was to determine whether 11C-hydroxyephedrine (11C-HED) can predict adverse events including all-cause death in Japanese patients with left ventricular (LV) dysfunction.
Background
Although 11C-HED PET has been used to assess cardiac sympathetic innervation in various disease conditions, data on their prognostic value are limited.
Methods
Sixty patients (mean LVEF, 42 ± 14 %) with LV dysfunction (42 ischemic and 18 non-ischemic heart disease) underwent 11C-HED PET. Myocardial retention was calculated for 11C-HED PET as a measure of cardiac sympathetic neuronal integrity. Statistical analysis was performed using Cox proportional hazards regression and log-rank test.
Results
Thirteen deaths (7 cardiac and 6 non-cardiac deaths) occurred during a mean follow-up period of 33 ± 23 months. The patients with death were associated with significantly lower 11C-HED retention (7.1 ± 2.1 vs 9.0 ± 2.4, p = 0.015) than those without death. The hazard ratio for global 11C-HED retention per unit (/min) was 0.762 (p = 0.039), which remained significant in multivariate analysis. When the patients were divided into the high (≥8.5) and low (<8.5) 11C-HED retention groups, the low 11C-HED retention group was associated with significantly poorer survival than the high 11C-HED retention group (p = 0.004).
Conclusion
The low global 11C-HED retention is a marker of poor overall survival in patients with LV dysfunction in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite recent advances in therapeutic options, heart failure (HF) continues to be one of the leading causes of mortality and morbidity in many countries [1]. It is well known that autonomic nerve function plays an important role in the pathogenesis and progression of HF [2], which is associated with excessive activation of sympathetic nerve activity [3], and reduction in functional neuronal density [4, 5]. Positron emission tomography (PET) using radio-labeled norepinephrine analogs such as 11C-hydroxyephedrine (11C-HED) has successfully been used to assess global and regional pre-synaptic sympathetic neuronal integrity of the heart [4, 6, 7]. As compared with more widely available 123I- metaiodobenzylguanidine (123I-MIBG) imaging [8, 9], it provides better tomographic image quality due to higher counting sensitivity and spatial resolution and the possibility of absolute quantification by routine use of attenuation/scatter correction [10]. However, there are only a few data available focusing on the prognostic value of 11C-HED PET [11, 12]; there is none from Japan. Moreover, no 11C-HED PET studies have reported all-cause mortality, which is increasingly being utilized as an unbiased endpoint in clinical trials [13].
The aim of this study was to determine whether 11C-HED can predict adverse events including all-cause death in Japanese patients with left ventricular (LV) dysfunction.
Materials and methods
Study population
This was a retrospective analysis of observational study to characterize HF using imaging biomarkers [10]. We consecutively screened 81 patients who had been referred to The Medical and Pharmacological Research Center Foundation as potential candidates of the study using the following criteria: (1) angiographically proven coronary heart disease (CHD) or non-ischemic symptomatic HF, because both disease conditions are known to cause abnormalities in cardiac sympathetic neuronal integrity, (2) regional or global (left ventricular ejection fraction (LVEF) of <50 %) left ventricular (LV) dysfunction documented by echocardiography, (3) 11C-acetate/11C-HED PET having been performed under stable general condition within 1 month after the entry, and (4) could be followed-up for >6 months in case of no events. The first criterion was met in all 81 patients; the second criterion in 74 patients; the third and fourth criteria in 60 patients. Patients were excluded if they (1) had unstabilized HF, (2) had acute coronary events (<10 days) such as myocardial infarction or unstable angina prior to the imaging study, or (3) were premenopausal women. There are none who met the exclusion criteria. Thus, 60 patients were finally included in the study. All cardiac medications such as beta-blockers were continued during the study period for safety reasons. After giving a written informed consent in accordance with institutional ethical committee, all patients underwent 11C-HED/11C-acetate PET imaging.
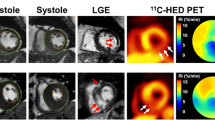
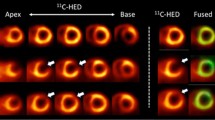
Positron emission tomography
The PET imaging was performed in a manner as described previously [5] using a full-ring PET scanner (Advance, GE Healthcare, Milwaukee, WI, USA). Briefly, transmission scan for 15 min was performed using 68Ge/68Ga pin sources for attenuation correction. Then, 370 MBq of 11C-acetate was intravenously injected, and a dynamic imaging sequence (21 frames, 10 × 10, 1 × 60, 5 × 100, 3 × 80, 2 × 300 s) was acquired for 30 min. In this study, 11C-acetate PET data were used to obtain relative perfusion images, which was necessary to measure perfusion defect size and mismatch size as mentioned later. Approximately 120 min after injection of 11C-acetate allowing for physical decay of 11C, the subjects were re-positioned in the scanner and a second transmission scan was acquired for 15 min. This was followed by intravenous injection of 370–600 MBq of 11C-HED, and a subsequent dynamic imaging for 40 min (14 frames, 6 × 30, 2 × 60, 2 × 150, 2 × 300, 2 × 600 s). The total radiation exposure for this imaging procedure was estimated to be <3.4 mSv [14, 15]. Images obtained from a representative case were shown in Fig. 1.
Echocardiography
Echocardiography was performed in all patients on the same day of PET imaging (between 11C-acetate and 11C-HED scan) using Vivid 7 (GE Healthcare, Milwaukee, WI, USA) with a 4 MHz transducer. LVEF was measured using Simpson biplane method.
Processing of PET data
Attenuation-corrected transaxial images were reconstructed using ordered subset expectation maximization algorithm. The image data matrix was 128’’ 128 with pixel size of 2.73 mm and a slice thickness of 4.25 mm. A volumetric sampling procedure was used to create polar maps of relative myocardial perfusion distribution throughout the entire LV myocardium as described elsewhere. In brief, summed data sets of frames 11–13 of the imaging sequence for 11C-acetate were used to create polar maps of myocardial activity distribution at 2–4 min after injection, which served as a relative perfusion image.
To obtain global 11C-HED retention fraction, the 11C-HED uptake averaged for the entire left ventricular myocardium at 30–40 min image was divided by the integral of blood activity curve, which served as a quantitative index of cardiac sympathetic innervation. Then, the polar maps were normalized to the mean of six connected sectors showing the highest overall uptake in the left ventricular myocardium. Defect size on the 11C-acetate flow image or 11C-HED image was quantified using a cutoff threshold of 60 % of the reference sectors and was expressed as a percentage of the left ventricular myocardium (%LV). Mismatch size was defined as 11C-HED defect size minus 11C-acetate perfusion defect size. Thus, global 11C-HED retention, perfusion defect size, 11C-HED defect size, and mismatch size were measured from PET imaging.
Follow-up
Clinical outcomes were confirmed by patient medical records or telephone interview. The primary endpoint was set to all-cause death; the secondary, cardiac death; and the tertiary, the composite endpoint including HF progression requiring hospitalization, life-threatening arrhythmias such as ventricular tachycardia, and acute coronary syndrome, or death of any cause. In case of multiple events, only the first event was used for analysis.
Statistical analysis
Data were expressed as mean ± SD unless specified. Statistical analysis was performed using JMP10 (SAS Institute Inc. Cary, NC, USA), or GraphPad Prism6 (GraphPad Software, Inc. San Diego, CA, USA), where appropriate. Wilcoxon rank sum test was used for comparison of variables between the two groups. Proportional difference between the groups was assessed using Chi-square test. Univariate and multivariate analyses using a Cox proportional hazards model were performed. The multivariate model for time to all-cause mortality, cardiac death, or composite endpoint was evaluated using a stepwise forward elimination procedure using variables including sex, age, LVEF, BNP, global 11C-HED retention, 11C-HED defect size, and mismatch size. In this study, we included only quantitative or objective and discrete variables; those such as NYHA class or presence of hypertension were not included because they were subjective or not necessarily discrete. In addition, the Kaplan–Meier method with log-rank test was applied to obtain survival curves. Optimal cut-off points for continuous variables were determined retrospectively using receiver operating characteristic (ROC) analysis [16]. A p value <0.05 was considered significant.
Results
Study participants
The clinical characteristics and cause of death are summarized in Table 1 and Supplemantary Table 1, respectively. Of the 42 patients with ischemic etiology, prior myocardial infarction was present in 32 patients. Of a total of 60 patients enrolled, 13 died (7 cardiac and 6 non-cardiac deaths) during the mean follow-up period of 33 ± 23 months (range 1–82, median: 24 months). Of the 7 patients with cardiac death, 2 died of sudden cardiac death and the remaining 5 of progression of HF. Cardiac events occurred in 17 patients, including 13 HF progression, 2 acute coronary syndromes, and 2 life-threatening arrhythmias.
All-cause mortality
Imaging parameters, patients characteristics, and serum BNP levels in patients with and without all-cause death are summarized in Table 2. The patients with death were associated with a lower LVEF, lower global 11C-HED retention, higher age, and higher serum BNP level than those without death. However, there were no significant differences in sex and perfusion defect size, although there was a trend towards larger 11C-HED defect size or mismatch size in patients with death than those without death. The results of univariate and multivariate Cox hazards analysis are summarized in Table 3. The univariate analysis identified age, BNP, and 11C-HED retention as a predictor of all-cause death. In the multivariate analysis, age and global 11C-HED retention remained significant. When the patients were divided into the high (≥8.5) and low (<8.5) global 11C-HED retention groups based on ROC analysis (Supplementary Fig. 1), the low 11C-HED retention group was associated with significantly poorer survival than the high 11C-HED retention group (p = 0.004) (Fig. 2).
Other endpoints
Imaging parameters, patients characteristics, and serum BNP levels in patients with and without cardiac death are summarized in Supplementary Table 2. The patients with death were associated with a higher serum BNP level than those without death. Additionally, there was a trend toward a lower LVEF and larger 11C-HED defect size in patients with death than those without death. However, global 11C-HED retention did not differ between the 2 groups. Using univariate Cox hazards analysis, LVEF and serum BNP level were significant predictors of cardiac death, of which only serum BNP remained significant in multivariate analysis (Supplemantary Table 3). The Kaplan–Meier analysis showed no significant difference in survival curve between the high (≥8.4) and low (<8.4) global 11C-HED retention groups (Fig. 2). When the composite endpoint was applied, the patients with event were associated with a lower LVEF, lower global 11C-HED retention, and higher serum BNP level than those without event (Supplementary Table 4). Additionally, there was a trend toward larger 11C-HED defect size or mismatch size in patients with event than those without event. Using univariate Cox hazards analysis, LVEF, global 11C-HED retention, mismatch size, and serum BNP level were significant predictors of event, of which only serum BNP remained significant in multivariate analysis (Supplementary Table 5). The Kaplan–Meier analysis showed that the low (<8.9) 11C-HED retention group was associated with significantly poorer prognosis than the high (≥8.9) 11C-HED retention group (p = 0.012) (Fig. 2).
Discussion
The major findings of this study were that (1), of the imaging parameters tested, global 11C-HED retention was a significant predictor of all-cause death, whereas global 11C-HED retention and mismatch size were predictors of the composite endpoint; (2) in multivariate analysis, age and global 11C-HED retention were independent predictors of all-cause death, whereas only serum BNP remained a significant predictor of cardiac death or composite endpoint.
Sympathetic neuronal imaging and its prognostic value
There is a general consensus that cardiac sympathetic neuronal function plays an important role for the pathogenesis of HF [2]. It is also known that an elevated circulating norepinephrine is a marker of poor outcome [17]. Using imaging techniques with radio-labeled norepinephrine analogs such as 123I-MIBG, there are a number of studies showing the prognostic value of cardiac sympathetic neuronal imaging, where the patients with low myocardial 123I-MIBG uptake as measured by semi-quantitative heart-to-mediastinum (H/M) uptake ratio are associated with poor prognosis [8, 9, 16, 18–20]. As compared to the aforementioned 123I-MIBG imaging, 11C-HED PET is considered to be a more sophisticated technique with higher image quality and opportunity of quantification of absolute tracer uptake. Additionally, an advantage of 11C-HED PET over 123I-MIBG imaging is that it provides higher tomographic image quality and, therefore, is more suitable for regional assessment, as demonstrated in our previous study [10]. However, there are only two studies that have systemically investigated the prognostic value of 11C-HED PET due to its limited availability. A retrospective study by Pietila et al. [11] of 46 patients with chronic heart failure (CHF) indicated that CHF patients had significantly lower global 11C-HED retention than healthy subjects, and that patients with poor prognosis (death or transplantation) had even lower retention. More recently, Fallavollita et al. [12] have demonstrated that regional myocardial sympathetic denervation assessed by 11C-HED PET was predictive for the risk of sudden cardiac arrest in 204 ischemic HF patients who had undergone implantable cardioverter defibrillator therapy. Our results demonstrated that age and low global 11C-HED retention were independent predictors of all-cause mortality, which remained true when multivariate analysis was performed, indicating that cardiac sympathetic dysinnervation as measured by 11C-HED PET is related to poor survival in patients with LV dysfunction independent of age. Regional parameters such as 11C-HED defect size were not significant predictors of all-cause mortality in this study, although there was a trend toward larger perfusion/11C-HED mismatch size in patients with death as compared to those without death. This indicates that global rather than regional sympathetic dysinnervation is a better marker of overall mortality. An issue that needs to be addressed is that all-cause mortality includes patients died of non-cardiac disease, including those of malignancy, traffic accident, and unknown cause. Although the exact mechanisms are not clear, it could be possible that the presence of severe HF as reflected by low global 11C-HED retention may have unfavorably affected overall survival even in such patients.
Although all-cause mortality is considered to be an objective and unbiased clinical endpoint, the selection of endpoint is still a matter of debate [13]. Therefore, we additionally assessed other endpoints such as cardiac death and composite endpoint. Cardiac death is a cause-specific and commonly used endpoint in clinical studies in patients with heart disease [8, 9, 16, 18–20]. The results showed that, although the patients with cardiac death tended to be associated with a larger 11C-HED defect than those without death, the PET derived parameters failed to show predictive power for cardiac death. The small sample size as well as potential misclassification of patients who actually died of cardiac cause as non-cardiac may explain the results. However, serum BNP level, a conventional parameter for HF severity, was still a significant predictor of cardiac death despite the small sample size, indicating that 11C-HED parameters have less significant predictive power than serum BNP in this setting. Thus, the prognostic value of 11C-HED PET may differ depending on what endpoint is chosen.
For the composite endpoint including any cardiac event and any death, the patients with events were associated with a lower global 11C-HED retention and higher serum BNP level than those without event. However, in multivariate analysis, only serum BNP survived as a significant predictor of the endpoint. Whether 11C-HED PET parameters would provide incremental prognostic value to serum BNP needs to be addressed in larger trials in future.
A potential advantage of employing 11C-HED PET instead of serum BNP would be that regional abnormalities can be assessed using PET technique. As aforementioned, a study by Fallavollita et al. [12] has demonstrated that regional but not global denervation is a predictor of sudden cardiac death. In our study, however, the prognostic value of regional parameters such as HED defect size was not clear mainly because of the limited sample size. Thus, our data have demonstrated that measuring serum BNP is still convenient and useful tool for prediction of cardiac event in any underlying causes.
Limitations
There are limitations of the study that need to be mentioned. First, the retrospective nature of the study prevented the enrollment of a homogeneous population. Additionally, strict medication control was difficult, where the prevalence of patients with beta-blocker therapy (47 %) was somewhat lower than that (66–96 %) reported in prior imaging studies in HF particularly from western countries [12, 20, 21]. However, this prevalence is not much different from that (54 %) reported in the largest meta-analysis study in Japan [16]. Second, due to the small number of patients, we could not test some cause-specific endpoints such as lethal arrhythmias. Because regional abnormalities in sympathetic innervation is reportedly linked to ventricular arrhythmias [12, 22, 23], this needs to be addressed in further studies. Finally, our patient population consisted of those with ischemic and non-ischemic etiology. In ischemic HF, the presence or absence of prior myocardial infarction may have an impact on prognosis. However, such a specific analysis would require a larger number of patients to draw definitive conclusions. A further study with a large number of ischemic patients is required to address this issue.
Conclusions
Our results indicate that age and low global 11C-HED retention measured by PET are independent markers of poor overall survival in Japanese patients with LV dysfunction in this study. Furthermore, the prognostic value of 11C-HED PET may differ depending on what endpoint is chosen.
References
Beadle RM, Williams LK, Abozguia K, Patel K, Leon FL, Yousef Z, et al. Metabolic manipulation in chronic heart failure: study protocol for a randomised controlled trial. Trials. 2011;12:140.
Cohn JN. Abnormalities of peripheral sympathetic nervous system control in congestive heart failure. Circulation. 1990;82:159–67.
Imamura Y, Ando H, Mitsuoka W, Egashira S, Masaki H, Ashihara T, et al. Iodine-123 metaiodobenzylguanidine images reflect intense myocardial adrenergic nervous activity in congestive heart failure independent of underlying cause. J Am Coll Cardiol. 1995;26:1594–9.
Bengel FM, Permanetter B, Ungerer M, Nekolla SG, Schwaiger M. Relationship between altered sympathetic innervation, oxidative metabolism and contractile function in the cardiomyopathic human heart; a non-invasive study using positron emission tomography. Eur Heart J. 2001;22:1594–600.
Aoki H, Matsunari I, Nomura Y, Fujita W, Komatsu R, Miyazaki Y, et al. Myocardial sympathetic innervation, function, and oxidative metabolism in non-infarcted myocardium in patients with prior myocardial infarction. Ann Nucl Med. 2013;27:523–31.
Schwaiger M, Kalff V, Rosenspire K, Haka MS, Molina E, Hutchins GD, et al. Noninvasive evaluation of sympathetic nervous system in human heart by positron emission tomography. Circulation. 1990;82:457–64.
Fallavollita JA, Banas MD, Suzuki G, deKemp RA, Sajjad M, Canty JM Jr. 11C- meta-hydroxyephedrine defects persist despite functional improvement in hibernating myocardium. J Nucl Cardiol. 2010;17:85–96.
Kasama S, Toyama T, Sumino H, Nakazawa M, Matsumoto N, Sato Y, et al. Prognostic value of serial cardiac 123I-MIBG imaging in patients with stabilized chronic heart failure and reduced left ventricular ejection fraction. J Nucl Med. 2008;49:907–14.
Verberne HJ, Brewster LM, Somsen GA, van Eck-Smit BL. Prognostic value of myocardial 123I-metaiodobenzylguanidine (MIBG) parameters in patients with heart failure: a systematic review. Eur Heart J. 2008;29:1147–59.
Matsunari I, Aoki H, Nomura Y, Takeda N, Chen WP, Taki J, et al. Iodine-123 metaiodobenzylguanidine imaging and carbon-11 hydroxyephedrine positron emission tomography compared in patients with left ventricular dysfunction. Circ Cardiovasc Imaging. 2010;3:595–603.
Pietilä M, Malminiemi K, Ukkonen H, Saraste M, Någren K, Lehikoinen P, et al. Reduced myocardial carbon-11 hydroxyephedrine retention is associated with poor prognosis in chronic heart failure. Eur J Nucl Med. 2001;28:373–6.
Fallavollita JA, Heavey BM, Luisi AJ Jr, Michalek SM, Baldwa S, Mashtare TL Jr, et al. Regional myocardial sympathetic denervation predicts the risk of sudden cardiac arrest in ischemic cardiomyopathy. J Am Coll Cardiol. 2014;63:141–9.
Zannad F, Garcia AA, Anker SD, Armstrong PW, Calvo G, Cleland JG, et al. Clinical outcome endpoints in heart failure trials: a European Society of Cardiology Heart Failure Association consensus document. Eur J Heart Fail. 2013;15:1082–94.
Seltzer MA, Jahan SA, Sparks R, Stout DB, Satyamurthy N, Dahlbom M, et al. Radiation dose estimates in humans for 11C-acetate whole-body PET. J Nucl Med. 2004;45:1233–6.
Shulkin BL, Wieland DM, Schwaiger M, Thompson NW, Francis IR, Haka MS, et al. PET scanning with hydroxyephedrine: an approach to the localization of pheochromocytoma. J Nucl Med. 1992;33:1125–31.
Nakata T, Nakajima K, Yamashina S, Yamada T, Momose M, Kasama S, et al. A pooled analysis of multicenter cohort studies of 123I-MIBG imaging of sympathetic innervation for assessment of long- term prognosis in heart failure. JACC Cardiovasc imaging. 2013;6:772–84.
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Fracis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311:819–23.
Merlet P, Valette H, Dubois-Randé JL, Moyse D, Duboc D, Dove P, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med. 1992;33:471–7.
Merlet P, Benvenuti C, Moyse D, Pouillart F, Dubois-Randé JL, Duval AM, et al. Prognostic value of MIBG imaging in idiopathic dilated cardiomyopathy. J Nucl Med. 1999;40:917–23.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212–21.
Verschure DO, Veltman CE, Manrique A, et al. For what endpoint does myocardial 123I-MIBG scintigraphy have the greatest prognostic value in patients with chronicheart failure? Results of a pooled individual patient data meta-analysis. Eur Heart J Cardiovasc Imaging. 2014;15:996–1003.
Simoes MV, Barthel P, Matsunari I, Nekolla SG, Schömig A, Schwaiger M, et al. Presence of sympathetically denervated but viable myocardium and its electrophysiologic correlates after early revascularised, acute myocardial infarction. Eur Heart J. 2004;25:551–7.
Bax JJ, Kraft O, Buxton AE, Fjeld JG, Pařízek P, Agostini D, et al. 123I-MIBG scintigraphy to predict inducibility of ventricular arrhythmias on cardiac electrophysiology testing: a prospective multicenter pilot study. Circ Cardiovasc Imaging. 2008;1:131–40.
Acknowledgments
This work was supported by Ishikawa prefectural government.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors have conflicts to disclose.
Funding sources
This work was supported by Ishikawa prefectural government.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fujita, W., Matsunari, I., Aoki, H. et al. Prediction of all-cause death using 11C-hydroxyephedrine positron emission tomography in Japanese patients with left ventricular dysfunction. Ann Nucl Med 30, 461–467 (2016). https://doi.org/10.1007/s12149-016-1081-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-016-1081-z