Abstract
Objective
To investigate clinical usefulness of a novel program “Heart Function View (HFV)” for evaluating left ventricular (LV) function from myocardial perfusion SPECT (MPS), we compared LV functional parameters (F(x)) calculated by HFV with those obtained by the other similar programs QGS and cardioGRAF or by ultrasound echocardiography (UCG) and examined their correlations with clinical markers of heart failure: plasma BNP concentrations (BNPs) and exercise capacity.
Methods
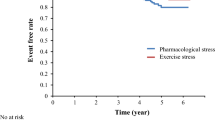
Studied patients (n = 60) underwent technetium-99m tetrofosmin quantitative gated MPS including treadmill exercise for examining heart disease. Myocardial stress images were acquired 30 min after the first tracer injection during maximal exercise. Three hours later, the second tracer was injected, and resting images were acquired. LV systolic F(x) [ejection fraction (EF), peak ejection rate (PER)] and diastolic F(x) [first third filling fraction (1/3FF), first third filling rate (1/3FR), peak filling rate (PFR), time to PFR (TPF)] were analyzed, and phase standard deviation (SD) and histogram bandwidth were obtained by phase analysis.
Results
LV end-diastolic volume (EDV), end-systolic volume (ESV) and EF obtained from HFV were well correlated with those from QGS, cardioGRAF and UCG. A diastolic parameter Doppler E/e′ from UCG was significantly with PFR from HFV. There were good correlations between LVEDV, LVESV, LVEF, PER, PFR, 1/3FR, TPF and 1/3FF from HFV and those from cardioGRAF. LVEF, PER, 1/3FR, and PFR were significantly correlated with plasma BNP concentrations. In patients with non-ischemic heart disease (n = 42), phase SD and histogram bandwidth were correlated negatively with exercise capacity or PFR.
Conclusions
HFV-derived LVF(x) are correlated with LVF(x) from the other programs or UCG, or with the clinical markers of heart failure and are thus useful in the functional assessment for patients with heart disease.






Similar content being viewed by others
Abbreviations
- AF:
-
Atrial fibrillation
- BNP:
-
B-type natriuretic peptide
- BNPs:
-
Plasma B-type natriuretic peptide concentrations
- ECG:
-
Electrocardiography/electrocardiogram
- EDV:
-
End-diastolic volume
- E/e′:
-
Tissue Doppler diastolic functional indicator
- EF:
-
Ejection fraction
- ESV:
-
End-systolic volume
- 1/3FF:
-
First third filling fraction
- 1/3FR:
-
First third filling rate
- F(x):
-
Functional parameters
- HFV:
-
Heart function view
- LBBB:
-
Left bundle branch block
- LV:
-
Left ventricle or ventricular
- MPS:
-
Myocardial perfusion SPECT
- PER:
-
Peak ejection rate
- PFR:
-
Peak filling rate
- QGS:
-
Quantitative gated SPECT
- SD:
-
Standard deviation
- SDS:
-
Summed difference score
- SPECT:
-
Single photon emission computed tomography
- SRS:
-
Summed rest score
- SSS:
-
Summed stress score
- TPF:
-
Time to peak filling
- UCG:
-
Ultrasound echocardiography
References
Wieczorek SJ, Wu AH, Christenson R, Krishnaswamy P, Gottlieb S, Rosano T, et al. A rapid B-type natriuretic peptide assay accurately diagnoses left ventricular dysfunction and heart failure: a multicenter evaluation. Am Heart J. 2002;144:834–9.
Lubien E, DeMaria A, Krishnaswarmy P, Clopton P, Koon J, Kazanegra R, et al. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation. 2002;105:595–601.
Bhatia V, Nayyar P, Dhindsa S. Brain natriuretic peptide in diagnosis and treatment of heart failure. J Postgrad Med. 2003;49:182–5.
Grossman W. Defining diastolic dysfunction. Circulation. 2000;101:2020–1.
Otterstad JE, Froeland G, St John Sutton M, Holme I. Accuracy and reproducibility of biplane two-dimensional echocardiographic measurements of left ventricular dimensions and function. Eur Heart J. 1997;18:507–13.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Redfield MM, Tajik AJ. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94.
Arques S, Roux E, Luccioni R. Current clinical applications of spectral tissue Doppler echocardiography (E/E′ ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound. 2007;5:16 Review.
Dhutia NM, Cole GD, Willson K, Rueckert D, Parker KH, Hughes AD, et al. A new automated system to identify a consistent sampling position to make tissue Doppler and transmitral Doppler measurements of E, E′ and E/E′. Int J Cardiol. 2012;155:394–9.
Germano G, Kavanagh P, Su HT, Mazzanti M, Hiat H, Hachamovich R, et al. Automatic reorientation of three-dimensional transaxial myocardial perfusion SPECT images. J Nucl Med. 1995;36:1107–14.
Germano G, Kiat H, Kavanagh P, Moriei M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med. 1995;36:2138–47.
Yamamoto A, Hosoya T, Takahashi N, Iwahara S, Munakata K. Quantification of left ventricular regional functions using ECG-gated myocardial perfusion SPECT—validation of left ventricular systolic functions. Ann Nucl Med. 2006;7:446–56.
Yamamoto A, Takahashi N, Munakata K, Hosoya T, Shiiba M, Okuyama T, et al. Global and regional evaluation of systolic and diastolic left ventricular temporal parameters using a novel program for ECG-gated myocardial perfusion SPECT—validation by comparison with gated equilibrium radionuclide angiography and speckle-tracking radial strain from echocardiography. Ann Nucl Med. 2007;21:115–21.
Hida S, Chikamori T, Tanaka H, Igarashi Y, Shiba C, Usui Y, et al. Diagnostic value of left ventricular dyssynchrony after exercise and at rest in the detection of multivessel coronary artery disease on single-photon emission computed tomography. Circ J. 2012;76:1942–52.
Matsuo S, Nakajima K, Kinuya S. Clinical use of nuclear cardiology in the assessment of heart failure. World J Cardiol. 2010;2:344–56.
Bruce RA. Exercise testing of patients with coronary heart disease: principles and normal standards for evaluation. Ann Clin Res. 1971;3:323–32.
Nakata T, Katagiri Y, Odawara Y, Eguchi M, Kuroda M, Tsuchihashi K, et al. Two- and three- dimensional assessments of myocardial perfusion and function by using technetium-99m sestamibi gated SPECT with a combination of count- and image-based techniques. J Nucl Cardiol. 2000;7:623–32.
Nakajima K, Taki J, Higuchi T, Kawano M, Taniguchi M, Maruhashi K, et al. Gated SPET quantification of small hearts: mathematical simulation and clinical application. Eur J Nucl Med. 2000;27:1372–9.
Nakajima K, Okuda K, Nyström K, Richter J, Minarik D, Wakabayashi H, et al. Improved quantification of small hearts for gated myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2013;40:1163–70.
Nakajima K. Normal values for nuclear cardiology: Japanese databases for myocardial perfusion, fatty acid and sympathetic imaging and left ventricular function. Ann Nucl Med. 2010;24:125–35.
Nagamachi S, Wakamatsu H, Fujita S, Nishii R, Kamimura K, Kiyohara S, et al. Assessment of diastolic function using 16-frame 201Tl gated myocardial perfusion SPECT: a comparative study of QGS2 and pFAST2. Ann Nucl Med. 2008;22:115–22.
Yoshino T, Nakae I, Matsumoto T, Mitsunami K, Horie M. Relationship between exercise capacity and cardiac diastolic function assessed by time–volume curve from 16-frame gated myocardial perfusion SPECT. Ann Nucl Med. 2010;24:469–76.
Skaluba SJ, Litwin SE. Mechanisms of exercise intolerance. Insight from tissue doppler imaging. Circulation. 2004;109:972–7.
Grewal J, McCully RB, Kane GC, Lam C, Pellikka PA. Left ventricular function and exercise capacity. JAMA. 2009;301:286–94.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakae, I., Hayashi, H., Matsumoto, T. et al. Clinical usefulness of a novel program “Heart Function View” for evaluating cardiac function from gated myocardial perfusion SPECT. Ann Nucl Med 28, 812–823 (2014). https://doi.org/10.1007/s12149-014-0875-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-014-0875-0