Abstract
The COVID-19 pandemic has impacted the mental health of the entire population, and especially of the healthcare, due to their close contact with the virus and the health emergency. However, the diversity of studies makes it difficult to determine the prevalence of mental health problems in Spanish healthcare workers. This study aims to examine the studies carried out during COVID-19 with the Spanish healthcare population to determine the prevalence of anxiety, depression, stress, post-traumatic stress (PTSD) and burnout symptomatology. A systematic search of the articles in the PubMed, Scopus and Web of Science databases was performed following PRISMA criteria. Pooled prevalence was obtained for all the mental health symptomatology from moderate to severe, as well as divided by wave. Our data revealed that 50.54% of healthcare workers reported stress, 41.02% burnout, 35.25% anxiety, 29.76% depression, and 25.82% PTSD symptomatology. Anxiety, depression, PTSD and burnout symptomatology diminished in the second and/or the third waves but increased in the following waves. However, stress showed the maximum prevalence during the second wave. Our study highlights a significant impact on the mental health of healthcare workers during health crises, and emphasizes the immediate need for mental health support for healthcare workers during and after pandemics. Anxiety, depression, PTSD, and burnout symptomatology exhibit a “valley” effect, initially decreasing but increasing with prolonged exposure to the COVID-19 health crisis. This underscores the necessity to implement prevention strategies to enhance stress management, emotional regulation skills, and coping abilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychological distress is a common experience during a pandemic, affecting both the general population and healthcare professionals. Various studies have looked into the consequences of the first major disease outbreak of the 21st century before COVID-19, Severe Acute Respiratory Syndrome (SARS) (Chua et al., 2004; Lee et al., 2007; Mak et al., 2009). These studies discovered that following the SARS outbreak, people often faced mental health challenges like adjustment difficulties, stress, and increased anxiety levels. A study conducted in a large teaching hospital in Toronto during the SARS outbreak found that nearly two-thirds of healthcare workers surveyed were dealing with significant psychological distress (Sim & Chua, 2004).
Working during or immediately after the onset of an infectious disease outbreak or a pandemic that could affect the healthcare system takes a toll on healthcare workers’ mental health and overall well-being. In their research, Mak et al. (2009) emphasize the importance of improving the readiness and competence of healthcare professionals in recognizing and addressing the psychological impact of potential infectious disease outbreaks (like SARS) in the future.
The COVID-19 pandemic has impacted the mental health of the entire population, leading to detrimental mental health outcomes such as depression, anxiety and traumatic stress (Salari et al., 2020; Xiong et al., 2020). Specific pandemic stressors associated with the pandemic, such as exposure to the virus or death, can increase the threat of being infected, uncertainty, distress and anxiety (Boden et al., 2021). These stressors are particularly prevalent in specific occupations, such as healthcare-related ones. Healthcare workers have been identified as one of the most vulnerable populations due to their close contact with the virus and the potential resulting health emergency (Kang et al., 2020). They may experience fear of contagion and concerns about spreading the virus to their loved ones (Xiang et al., 2020).
Furthermore, the use of protective equipment during the COVID-19 pandemic has been related to physical and psychological issues, with fear due to the lack of protective equipment (Sánchez-Sánchez et al., 2021), but also fear and anxiety about wearing protective equipment reported by 14–28% of healthcare workers (Radha et al., 2022). Additionally, discrimination and stigmatization faced by healthcare workers during the pandemic (Bagcchi, 2020) could increase the risk of suffering distress, anxiety, and depression (Park et al., 2018). These factors collectively highlight healthcare workers as a population with a particular risk of suffering mental well-being deterioration during the Covid-19 pandemic (Tomalá León et al., 2021).
Healthcare workers have experienced a high prevalence of emotional disorders, sleep problems, physical and mental exhaustion, post-traumatic stress, and suicidal ideation (Kang et al., 2020). A recent meta-analysis (Saragih et al., 2021) revealed that post-traumatic stress disorder was the most common mental health disorder reported by healthcare workers during the COVID-19 pandemic (49%), followed by anxiety (40%), depression (37%) and distress (37%). In addition to impacting their well-being, these manifestations can affect the service quality and interfere with patients’ health (Firth-Cozens & Greenhalgh, 1997; Shanafelt et al., 2002; Williams et al., 2007).
Moreover, mental health problems such as depressive and anxiety disorders were especially increased in the areas more affected by COVID-19, where the restrictions were stricter (Aknin et al., 2022). Spain was one of the European countries more affected by the COVID-19 pandemic during the first wave, with a peak of 913 daily deaths in April 2020 (World Health Organization, 2023). The national health system faced overwhelming circumstances, and healthcare workers were exposed to significant risks of infection. A state of emergency was declared in March 2020 to manage the health emergency in this country when there was still no vaccine and a worldwide shortage of masks and protective equipment. Since then, urgent measures have been taken to address the spread of the virus and mitigate the impact of the COVID-19 pandemic. One of these measures was the lockdown, which was one of the most restrictive in Europe (Ayuso-Mateos et al., 2021). People were confined to their homes, except for essential activities, which also had a significant psychological and social impact on the Spanish population (Matalí-Costa & Camprodon-Rosanas, 2022). A study conducted in the initial stage of the COVID-19 pandemic showed that 18.7% of Spaniards revealed depression, 21.6% anxiety, and 15.8% PTSD symptoms (González-Sanguino et al., 2020). In addition, a study comparing the mental health of Chinese and Spanish individuals found that Spanish participants reported higher levels of stress and depression than their Chinese counterparts. Adverse mental health outcomes were associated with increased exposure to health information (Wang et al., 2021). Also, one study showed greater emotional problems in Spanish nursing students who volunteered to provide health aid in the absence of health personnel compared with other countries (Patelarou et al., 2021). This evidence raises questions about whether the Spanish health system could be particularly affected by the COVID-19 pandemic. Alonso et al. (2021) showed that one in seven Spanish healthcare workers could have suffered a mental disorder during the first wave of the COVID-19 pandemic. In the context of a pandemic, a “wave” refers to a period of increased disease incidence, where the number of cases rises sharply, reaches a peak, and then gradually declines. Waves represent peaks and troughs in the infection curve over time, indicating recurrent outbreaks of the disease in a population. The duration and magnitude of each wave can vary based on factors like control measures, virus variants, and population response. In Spain, to date, there have been seven distinct waves of the COVID-19 pandemic, resulting in a cumulative death toll exceeding 120,000 (INE, 2023). These successive waves represent complex epidemiological dynamics, requiring an analysis to understand their psychological impact better.
Based on the existing evidence on mental health in health professionals during the COVID-19 pandemic, the present study aims to provide a broad vision of the psychological impact caused on health professionals in Spain. Specifically, this study investigates the prevalence of symptoms of depression, anxiety, stress, post-traumatic stress disorder (PTSD), and burnout among Spanish healthcare workers. It encompasses both overall data and a comprehensive wave-by-wave analysis. Understanding the most prevalent symptoms among this population (e.g., doctors, nurses, paramedics, support staff, etc.) and identifying the characteristics of healthcare workers most affected by the COVID-19 pandemic are crucial steps toward developing effective tools to support these individuals (Tomalá León et al., 2021).
Method
Search strategy
A systematic search of the literature available in the PubMed, Scopus and Web of Science databases was performed, following the criteria of the PRISMA statement (Page et al., 2021). The terms used for this systematic review were organized around three elements: (1) COVID-19 pandemic (terms used: COVID, coronavirus, SARS CoV-19); (2) health and social-health workers who provided healthcare during the pandemic (terms used: healthcare, staff, professional, workers, nurse, physician, professional caregivers); (3) psychological impact (terms used: mental, emotion, psychol*, stress and burnout). The search was conducted in September 2022. Additionally, Google Scholar and citations and reference lists from relevant articles were reviewed (forward and backward snowballing searches).
Identification and selection studies
Two investigators conducted the screening, identification, and selection process (IJ and CA-G). They independently analyzed all the articles by title and abstract to exclude those unrelated to the topic. Next, the investigators assessed full-text versions of the relevant articles to determine final eligibility. The inclusion criteria were (1) original articles, (2) Spanish or English language, (3) published between 2019 and 2022, (4) Spanish health and social-health professionals, (5) variables assessed: depression, anxiety, stress, PTSD, and burnout, (6) frequencies for moderate or severe symptomatology. The exclusion criteria were: (1) do not meet any of the inclusion criteria; (2) sample: physiotherapists, dentists, and pharmacists who do not work in a health or social-health centre; (3) insufficient data to obtain prevalences; (4) do not use of validated measures. After this classification by the authors, the agreement was checked. When consensus was not reached, a third reviewer (DC) was included, who made the final decision.
Data extraction
A pre-designed data extraction sheet was used to include the data about the final included studies. This sheet contains the following variables: (a) study (authors and year of publication), (b) aim of the study, (c) design of the study, (d) participants, (e) sample size, (f) wave of the pandemic when the data was collected, (g) measures of assessment, and (h) the percentage of participants with moderate to severe mental health symptomatology for anxiety, depression, stress, PTSD and/or burnout. Additionally, the number of participants with moderate and severe symptomatology was extracted or calculated from the percentages provided by the authors to obtain a pooled prevalence of mental health problems (Supplementary material 1). Studies that did not report specific percentages or the number of participants with anxiety, depression, stress, PTSD, or burnout symptomatology were excluded from this analysis. All the variables mentioned above were extracted and coded independently by IJ and CA-G. Disagreements were resolved through discussion with a third author (DC).
To mitigate the risk of analyzing the same sample across multiple publications, we carefully reviewed the articles to confirm the explicit specification of sample collection dates. Consequently, we decided to leave the baseline subsample of Alonso et al. (2022) out of our analyses, as it corresponds to the sample used in their 2021 study. Also, studies that recruited their samples during different waves were classified based on the wave when recruitment began. This method was implemented to prevent redundant analysis of identical datasets and to uphold the integrity of our systematic review. However, new data from two publications conducted by the same authors in the same wave were included (Mediavilla et al., 2021, 2022; Dosil et al., 2020, 2021) due to the uncertainty regarding the sample used in the more recent study.
Results
Selection and inclusion of studies
The search in the three databases generated a total of 515 articles (Pubmed = 104; Scopus = 371; Web of Science = 40). Additionally, one study was obtained through Google Scholar. After eliminating duplicates, a total of 459 documents were screened by title and abstract by two independent researchers. After comparing the findings from both researchers, 140 full-text versions were assessed for eligibility. After exclusions, a total of 44 studies were selected to be included in the systematic review (Fig. 1).
Characteristics of included studies
The characteristics of the included studies are presented in Table 1. The studies included in this systematic review were mainly conducted during the first wave. Some studies were conducted during the subsequent waves, including the second, third, fourth or fifth waves. Notably, no studies were identified that were conducted during the sixth wave. Regarding the study design, the majority of the studies were cross-sectional. Additionally, one study was a validation study, and one was a Randomized Controlled Trial. Furthermore, some studies utilized a longitudinal design to examine healthcare workers’ mental health during different phases of the COVID-19 pandemic.
Regarding the sample, studies usually included physicians, nurses, nursing assistants, technicians, and other health workers indistinctly. In addition, they collected a large number of participants from different inpatient and outpatient health centres such as primary care, hospitals, outpatient services, covid units, and ICUs, among others. Also, two studies were distributed in public and private socio-health care centres (e.g., nursing homes for older adults; Martínez-López et al., 2021; Molina-Mula et al., 2022).
Studies assessed anxiety (n = 24), depression (n = 26), stress (n = 19), PTSD symptomatology (n = 13) and burnout (n = 13) using different measures. Specifically for anxiety, studies included the Generalized Anxiety Disorder Scale (GAD-7; n = 7), the Depression Anxiety Stress Scale-21 (DASS-21; n = 6), the Hospital Anxiety Depression Scale (HADS, n = 5), the State-Trait Anxiety Inventory (STAI; n = 3), the Beck Anxiety Inventory (BAI; n = 1), and the Goldberg Anxiety and Depression Scale (GADS; n = 1). In terms of depression, the questionnaire most used was the Patient Health Questionnaire (PHQ), which was used in the nine (n = 7), eight (n = 2), and two items (n = 2) versions. The second measure most used was the DASS-21 (n = 6), followed by the HADS (n = 5), the Beck Depression Inventory-II (BDI-II; n = 1), the Hamilton Depression Rating Scale (HDRS; n = 1), the Montgomery-Asberg Depression Rating Scale (MADRS; n = 1), and the Goldberg Anxiety and Depression Scale (GADS; n = 1). Also, one study (Rodríguez-Rey et al., 2020) used two items in which participants were asked if they were depressed and how sad they were feeling to screen for depression, which had shown adequate sensitivity and specificity to detect emotional distress in previous studies. The scale most used for assessing stress was the DASS-21 (n = 6), followed by the Perceived Stress Scale (PSS) in the four (n = 1), ten (n = 1) or 14 items (n = 2) versions. The Stanford Reaction Questionnaire (n = 1), the General Health Questionnaire-12 (n = 3), the Impact of Event Scale-Revised (IES-R; n = 4), and the EASE (n = 1) were also used. In addition, one study also use screenings based on DSM-5 criteria for assessing acute stress. For the assessment of PTSD symptomatology, the measure most used was the PTSD Checklist for DSM-5 (PCL-5; n = 5). In addition, the Impact of Event Scale-Revised (IES-R; n = 4), the Davidson Trauma Scale (DTS; n = 3), the International Trauma Questionnaire (ITQ; n = 1), and the Primary Care PTSD Screen for the DSM-5 (n = 1) were used. Finally, the Burnout Syndrome was mainly evaluated by the Maslach Burnout Inventory (MBI; n = 8), but also with the Burnout Clinical Subtype Questionnaire (BCSQ-36; n = 1), and the Burnout subscale of the Professional Quality of Life Scale (ProQoL; n = 5).
Prevalence findings for anxiety
As shown in Table 1, the reported prevalence of moderate and severe anxiety symptoms among the studies included in this systematic review ranged from 14.28 to 98.43%. The lowest prevalence was found in the study by Bourne et al. (2022), conducted during the first wave with professionals working with ultrasounds in obstetrics and gynecology. The highest prevalence was found in the longitudinal study by Esteban-Sepúlveda et al. (2022) conducted during the second and third waves with healthcare workers with direct contact with patients with COVID-19.
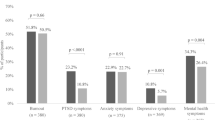
The pooled percentages of moderate and severe anxiety symptoms were calculated using the total number of participants with symptoms during each wave across all studies. Results indicated a pooled prevalence of 35.18% for moderate and severe anxiety symptoms. In addition, the analysis of prevalence conducted by wave showed that the third wave was the wave with a higher prevalence of anxiety (Fig. 2A). Likewise, the third, fourth, and fifth waves showed higher prevalence than the first and second waves.
Prevalence findings for depression
The prevalence of moderate and severe depressive symptoms in this systematic review ranged from 7.14 to 82.22%. As in the case of anxiety, the study of Bourne et al. (2022) was the study showing the lowest depression prevalence, while the highest prevalence was found in the study conducted by Moraleda-Cibrián et al. (2022) during the third and fourth waves.
The pooled prevalence of moderate and severe depression symptomatology was 29.77%. As shown in Fig. 2B, the prevalence of depression symptomatology decreased from the first to the second and third waves but raised again in the fourth and fifth waves, with the fifth wave showing the highest prevalence of depression symptomatology. Accordingly, longitudinal studies found that depression was less prevalent during the first wave compared to the second wave (Sánchez-Sánchez et al., 2021) and during the first wave compared to the third wave (Mediavilla et al., 2022).
Prevalence findings for stress
Concerning stress, the included studies reported a prevalence of moderate to severe symptoms with percentages ranging from 14.68% to 80,60%. Most studies that included stress as an outcome were conducted during the first wave, with only one study conducted during the fourth wave and none in the fifth wave. The lowest prevalence was found in the study conducted by Erquicia et al. (2020) during the first wave in hospitals, while the highest prevalence was found in the study by Gómez-Salgado et al. (2021) during the first wave in hospitals and primary care.
The pooled prevalence of stress was 50.52%, this symptom being the most prevalent during the COVID-19 pandemic, compared to the other outcomes included in this systematic review. As shown in Fig. 2C, the total stress prevalence pooled by the wave was similar for the first, second and third waves (50.20% and 56.20%, respectively), while the only study conducted in the fourth wave with health professionals of emergency medical services (Soto-Camara et al., 2022) found the lowest stress prevalence (37.37%).
Prevalence findings for post-traumatic stress symptoms
The studies included in this systematic review showed a wide range of PTSD symptoms prevalence, ranging from 11.10 to 78.07%. Specifically, the highest prevalence was found by Rodríguez-Rey (2020), who collected a sample of frontline professionals during the first wave. The lowest prevalence was found in the study conducted by Dosil et al. (2020) after fattening the curve of the first wave with a higher pool of healthcare professionals not necessarily working on the frontline.
Regarding the pooled prevalence, this study found that a quarter of the healthcare workers (25.82%) showed moderate-severe PTSD symptomatology. Notably, there was a decrease in prevalence observed between the first three waves (21.1-29.5%) and the fifth wave (12.3%) of the COVID-19 pandemic (Fig. 2D). These results are in line with the longitudinal study conducted by Esteban-Sepúlveda et al. (2022), which showed that the stress prevalence in the second and third waves was very similar, with a slight increase from the second to the third wave (24.44% and 26.56% respectively).
Prevalence for burnout symptoms
The prevalence of burnout symptoms among health workers during the COVID-19 pandemic has varied considerably depending on the study, ranging from 4.32 to 83.99%. The highest and the lowest prevalences were found during the first wave (Ruiz-Fernandez et al., 2020; Ruiz-Fernandez et al., 2020).
The pooled prevalence for burnout symptomatology was 41,02%. All studies that included burnout outcomes were conducted during the first, second, and third waves, with no studies found for the fourth and fifth waves. As shown in Fig. 2E, the cases of burnout symptomatology were higher during the first wave (43.1%) compared with the other waves. The rate of burnout symptoms decreased during the second wave; it increased again during the third wave, although without reaching the levels of the first wave.
Table 2 provides a summary of the prevalence ranges found for each symptom, as well as the mean for each wave.
Discussion
This systematic review represents the first comprehensive examination of the prevalence of depression, anxiety, stress, post-traumatic stress disorder (PTSD), and burnout symptoms among Spanish healthcare professionals during the COVID-19 pandemic. The study analyzed a total of 44 studies conducted during the first five waves of the COVID-19 pandemic in Spain, covering the period from the beginning of the pandemic to September 2022.
The results indicated that 50.54% of healthcare workers reported symptoms of stress, 41.02% reported burnout, 35.25% reported anxiety, 29.76% reported depression, and 25.82% reported PTSD symptoms. The prevalences obtained in this study were slightly higher than those reported by the global study by Salari et al. (2020), who found prevalences of stress, anxiety, and depression of 45%, 25.8%, and 24.3%, respectively. It is worth mentioning that most of the studies included in Salari et al. (2020) were conducted in Asia (i.e., China, Nepal, Iran, Japan, and India). Therefore, these findings align with previous literature (Wang et al., 2021), suggesting that the Spanish population report higher levels of emotional symptomatology than the Chinese population.
In addition, the pooled prevalences of post-traumatic stress, anxiety, and depression symptoms obtained in this study were lower than those reported in the meta-analyses conducted by Saragih et al. (2021), which included studies from various countries. However, the prevalence of stress shown in this systematic review was higher than the one reported by Saragih et al. (2021). One possible explanation for this discrepancy may be the difference in search dates. The current study included a larger set of studies published until September 2022, whereas Saragih et al. (2021) finished their search in November 2020. Subsequently, Saragih et al. (2021) included data collected only during the first two waves, while this systematic review included studies conducted from the first to the fifth wave, periods with fewer restrictions and severity of COVID-19 cases in medical services. This might explain the higher prevalence reported by Saragih et al. (2021) compared to the prevalence found in our study, as mortality rates were likely lower during later waves.
In this line, our results showed differences in the prevalence of symptomatology related to stress, PTSD, and burnout symptomatology across the different pandemic waves. Anxiety and burnout showed a reduction in symptomatology in the second wave but rose again in the third wave, affecting 51.8% and 34% of healthcare workers, respectively. Similarly, depression symptoms decreased during the second and third waves but increased again in the fourth, with up to 30% of healthcare workers experiencing it. Also, PTSD symptomatology decreased on the second wave with an increase in the third wave, although slighter in this case. Our findings are consistent with previous longitudinal studies that have reported a reduction in the prevalence of anxiety and depression symptoms from the first to the third wave (Sánchez-Sánchez et al., 2021; Mediavilla et al., 2022). However, our results suggest that Spanish healthcare workers still suffered from the emotional consequences of the pandemic during the fourth and fifth waves, with prevalences even higher than during the first wave. This is evident in the patterns of anxiety symptoms waves, in which the third, fourth, and fifth waves exhibited a higher prevalence than the first and second waves. These results are in contrast with longitudinal studies that were included in this review, showing that the prevalence of anxiety was higher during the first wave compared with the second and the third waves of the COVID-19 pandemic, suggesting that the beginning of the pandemic could be associated with more confusion, lack of information, lack of training of these professionals, the large number of infections and a lack of diagnostic tests (Mediavilla et al., 2022; Sánchez-Sánchez et al., 2021).
Importantly, it is widely recognised that long-term stress can lead to adverse psychological outcomes, and this holds particularly true for healthcare practitioners who encounter elevated levels of stress in their professional roles (Kersting et al., 2019; Lykkegaard et al., 2020). Therefore, although the number of studies decreases considerably after the third wave, it is crucial to continue monitoring and addressing the mental health needs of healthcare workers (Zhang et al., 2020). In fact, a recent study conducted in Romania showed that the COVID-19 pandemic continues to have a high impact on healthcare workers’ mental health (Briciu et al., 2023). Thus, prevention and developing intervention programs that enhance emotional skills are essential, especially in this population. Additionally, supportive leadership, communication, and access to mental health resources can help alleviate the pandemic’s burden on healthcare workers (Kang et al., 2021).
The prevalences obtained in this systematic review conducted with healthcare workers were higher compared to those obtained with the general population (Ozamis-Etxebarria et al., 2020; Sandin et al., 2020), yielding evidence of the mental health problem of healthcare workers during the COVID-19 pandemic. Furthermore, a study included in this systematic review (Seda-Gombau et al., 2021) showed a significant rise in burnout symptoms among health workers during the COVID-19 pandemic, compared with pre-pandemic periods. In this regard, several studies have highlighted the impact of healthcare workers’ mental health on the quality of care they provide (Shanafelt et al., 2015, 2016; Maben et al., 2012; Koinis et al., 2015). Therefore, it is essential to prioritize healthcare workers’ mental health to ensure high-quality patient care. By promoting and developing interventions to improve and preserve healthcare workers’ mental health, we can ensure they are better equipped to provide high-quality patient care.
Interestingly, this systematic review found differences in the prevalence of symptomatology even in studies conducted in the same period. This suggests that factors such as the type of healthcare professionals or the type of centre participating in the study may affect the prevalences obtained. For instance, some studies (Erquicia et al., 2020; Dosil-Santamaría et al., 2021) showed that the prevalence of mental problems was higher for centres with higher exposition to COVID-19 contagion (i.e., primary care centres) and the severity of the patients was greater (i.e., emergency services, urgencies, critical health units). However, most studies included a mix of different types of healthcare facilities, which makes it challenging to tease apart the specific influence of each factor in this study. In addition, it is worth noting that there was little representation of workers from social-health centres, either because there is a lack of studies focused on this population or because they have not been differentiated from the personnel from healthcare centres. Consequently, it was not possible to determine the specific prevalence of mental health symptomatology for social-health workers and compare them with healthcare personnel. Also, using different measures to assess mental health makes comparing the prevalences obtained in the different studies difficult.
Another notable aspect is that studies included in this systematic review have also shown that the proportion of healthcare workers with emotional symptomatology was higher when there is a perceived lack of centre preparedness (Alonso et al., 2022), including less personal protection equipment availability (Bajo et al., 2021). These findings highlight the importance of work-related factors concerning mental health problems and suggest the need to address them to decrease chronicity among healthcare workers (Alonso et al., 2022).
Limitations
Our research has several limitations that should be considered. Firstly, due to the relatively recent emergence of the COVID-19 pandemic, there is a possibility that we might have overlooked studies that have yet to be published. In addition, the differentiation between first-line healthcare services and other healthcare services was challenging because most of the studies included in this systematic review encompassed a variety of healthcare settings. Another limitation arises from the exclusion of certain studies from the analysis. Some studies were excluded because they did not provide data on the number or percentage of participants experiencing symptoms of anxiety, depression, stress, PTSD, or burnout (e.g., Lara-Cabrera et al., 2021). Also, in cases where studies recruited their samples during different waves, we categorized them according to the specific wave in which recruitment began. This categorization was essential to prevent analysis using identical datasets. However, this method could influence the prevalences obtained in this systematic review. Furthermore, we had to exclude studies that used the Maslach Burnout Inventory (MBI) to assess burnout symptoms but reported participant numbers affected by specific MBI subscales (such as emotional exhaustion, depersonalization, or personal realization) without reporting across all the scales, which is the criterion for diagnosing burnout syndrome with this measure (Maslach & Jackson, 1982).
Lastly, another potential limitation of this systematic review pertains to our choice of search terms, specifically “mental,” “emotion,” “psychol*,” “stress,” and “burnout.” Although these terms are comprehensive and encompass a wide range of psychological manifestations, the articles included in this systematic review primarily focus on the specific symptoms outlined in our research—stress, burnout, anxiety, depression, and PTSD symptomatology. This limitation suggests that our findings may not fully encompass the complete spectrum of psychological symptoms associated with this topic, primarily due to the constraints inherent in the reviewed articles.
Conclusions
To sum up, this systematic review revealed that stress was the most prevalent symptom experienced by healthcare workers during the COVID-19 pandemic, followed by burnout, anxiety, depression, and PTSD symptoms. The prevalence of mental health symptoms ranged from 27% to 49, highlighting the significant psychological impact that the pandemic had on healthcare workers. In addition, the results divided by wave provide insight into the impact of the COVID-19 pandemic on mental health across different and emphasize the urgent need for psychological interventions to improve and preserve the mental health of healthcare professionals, given their high risk of developing mental health disorders. Therefore, it is crucial to prioritize implementing measures and resources to support the psychological well-being of healthcare workers during and after the pandemic.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary material.
References
Aknin, L. B., Andretti, B., Goldszmidt, R., Helliwell, J. F., Petherick, A., De Neve, J. E., Dunn, E. W., Fancourt, D., Goldberg, E., Jones, S. P., Karadag, O., Karam, E., Layard, R., Saxena, S., Thornton, E., Whillans, A., & Zaki, J. (2022). Policy stringency and mental health during the COVID-19 pandemic: A longitudinal analysis of data from 15 countries. The Lancet Public Health, 7(5), e417–e426. https://doi.org/10.1016/S2468-2667(22)00060-3
Alonso, J., Vilagut, G., Mortier, P., Ferrer, M., Alayo, I., Aragón-Peña, A., Aragonès, E., Campos, M., Cura-González, I. D., Emparanza, J. I., Espuga, M., Forjaz, M. J., González-Pinto, A., Haro, J. M., López-Fresneña, N., de Salázar, A. D. M., Molina, J. D., Ortí-Lucas, R. M., Parellada, M., & Pérez-Solà, V. (2021). Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Revista De Psiquiatria Y Salud Mental, 14(2), 90–105. https://doi.org/10.1016/j.rpsm.2020.12.001
Alonso, J., Vilagut, G., Alayo, I., Ferrer, M., Amigo, F., Aragón-Peña, A., Aragonès, E., Campos, M., Cura-González, D., Urreta, I., Espuga, I., González Pinto, M., Haro, A., López Fresneña, J. M., Martínez, N., De Salázar, A., Molina, J. D., Ortí Lucas, R. M., Parellada, M., Pelayo-Terán, J. M., & Mortier, P. (2022). Mental impact of Covid-19 among Spanish healthcare workers. A large longitudinal survey. Epidemiology and Psychiatric Sciences, 31. https://doi.org/10.1017/S2045796022000130
Aranda-Reneo, I., Pedraz-Marcos, A., & Pulido-Fuentes, M. (2021). Management of burnout among the staff of primary care centres in Spain during the pandemic caused by the SARS-CoV-2. Human Resources for Health, 19(1). https://doi.org/10.1186/s12960-021-00679-9
Ayuso-Mateos, J. L., Mediavilla, R., Rodriguez, K. R., & Bravo, M. F. (2021). Informing the response to COVID-19 in Spain: Priorities for mental health research. Revista De psiquiatria y salud Mental, 14(2), 79–82. https://doi.org/10.1016/j.rpsm.2021.04.001
Bagcchi, S. (2020). Stigma during the COVID-19 pandemic. The Lancet Infectious Diseases, 20(7), 782. https://doi.org/10.1016/S1473-3099(20)30498-9
Bajo, M., Gallego, P., Stavraki, M., Lamprinakos, G., Luna, P., & Díaz, D. (2021). Anxiety, trauma and well-being in health-care professionals during COVID-19 first wave in Spain: The moderating role of personal protection equipment availability. Health and Quality of Life Outcomes, 19(1). https://doi.org/10.1186/s12955-021-01845-2
Beneria, A., Arnedo, M., Contreras, S., Pérez-Carrasco, M., Garcia-Ruiz, I., Rodríguez-Carballeira, M., Raduà, J., & Rius, J. B. (2020). Impact of simulation-based teamwork training on COVID-19 distress in healthcare professionals. BMC Medical Education, 20(1), 515. https://doi.org/10.1186/s12909-020-02427-4
Boden, M., Zimmerman, L., Azevedo, K. J., Ruzek, J. I., Gala, S., Magid, A., Cohen, H. S., Walser, N., Mahtani, R., Hoggatt, N. D., K. J., & McLean, C. P. (2021). Addressing the mental health impact of COVID-19 through population health. Clinical Psychology Review, 85(March). https://doi.org/10.1016/j.cpr.2021.102006
Bourne, T., Kyriacou, C., Shah, H., Ceusters, J., Preisler, J., Metzger, U., Landolfo, C., Lees, C., & Timmerman, D. (2022). Experiences and well-being of healthcare professionals working in the field of ultrasound in obstetrics and gynaecology as the SARS-CoV-2 pandemic were evolving: A cross-sectional survey study. British Medical Journal Open, 12(2). https://doi.org/10.1136/bmjopen-2021-051700
Briciu, V., Leucuta, D. C., Tőkés, G. E., & Colcear, D. (2023). Burnout, depression, and job stress factors in healthcare workers of a Romanian COVID-19 dedicated hospital, after two pandemic years. International Journal of Environmental Research and Public Health, 20(5), 4118. https://doi.org/10.3390/ijerph20054118
Chua, S. E., Cheung, V., McAlonan, G. M., Cheung, C., Wong, J. W., Cheung, E. P., Chan, M. T., Wong, T. K., Choy, K. M., Chu, C. M., Lee, P. W., & Tsang, K. W. (2004). Stress and psychological impact on SARS patients during the outbreak. Canadian Journal of Psychiatry Revue canadienne de psychiatrie, 49(6), 385–390. https://doi.org/10.1177/070674370404900607
Cunill, M., Aymerich, M., Serdà, B. C., & Patiño-Masó, J. (2020). The impact of COVID-19 on Spanish health professionals: A description of physical and psychological effects. International Journal of Mental Health Promotion, 22(3), 185–198. https://doi.org/10.32604/IJMHP.2020.011615
Dosil, M., Ozamiz-Etxebarria, N., Redondo, I., Picaza, M., & Jaureguizar, J. (2020). Psychological symptoms in Health professionals in Spain after the first wave of the COVID-19 pandemic. Frontiers in Psychology, 11, https://doi.org/10.3389/fpsyg.2020.606121
Dosil Santamaria, M., Ozamiz-Etxebarria, N., Rodriguez, R., Alboniga-Mayor, I. J., J., & Gorrotxategi, P., M (2021). Psychological impact of COVID-19 on a sample of Spanish health professionals. Revista De Psiquiatria Y Salud Mental, 14(2), 106–112. https://doi.org/10.1016/j.rpsm.2020.05.004
Echeverria, I., Peraire, M., Haro, G., Mora, R., Camacho, I., Almodóvar, I., Mañes, V., Zaera, I., & Benito, A. (2021). Healthcare Kamikazes during the COVID-19 pandemic: Purpose in Life and moral courage as mediators of psychopathology. International Journal of Environmental Research and Public Health, 18(14). https://doi.org/10.3390/ijerph18147235
Erquicia, J., Valls, L., Barja, A., Gil, S., Miquel, J., Leal-Blanquet, J., Schmidt, C., Checa, J., & Vega, D. (2020). Emotional impact of the Covid-19 pandemic on healthcare workers in one of the most important infection outbreaks in Europe. Medicina Clinica, 155(10), 434–440. https://doi.org/10.1016/j.medcli.2020.07.006
Esteban-Sepúlveda, S., Terradas-Robledo, R., Castro-Ribeiro, T., García-Pagès, E., Sobregrau-Sangrà, P., & Lacueva-Pérez, L. (2022). COVID-19 pandemic on health professionals in a third level hospital in Spain: Job changes during the first wave, mental health at 4 months, and follow-up at 9 months. Enfermeria Clinica, 32(3), 143–151. https://doi.org/10.1016/j.enfcli.2021.12.009
Fiol-DeRoque, M. A., Serrano-Ripoll, M. J., Jiménez, R., Zamanillo-Campos, R., Yáñez-Juan, A. M., Bennasar-Veny, M., Leiva, A., Gervilla, E., García-Buades, M. E., García-Toro, M., Alonso-Coello, P., Pastor-Moreno, G., Ruiz-Pérez, I., Sitges, C., García-Campayo, J., Llobera-Cánaves, J., & Ricci-Cabello, I. (2021). A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): Randomized controlled trial. JMIR MHealth and UHealth, 9(5). https://doi.org/10.2196/27039
Firth-Cozens, J., & Greenhalgh, J. (1997). Doctors’ perceptions of the links between stress and lowered clinical care. Social Science & Medicine (1982), 44(7), 1017–1022. https://doi.org/10.1016/s0277-9536(96)00227-4
Gago-Valiente, F. J., Moreno-Sánchez, E., Santiago-Sánchez, A., Gómez-Asencio, D., Merino-Godoy, M., Castillo-Viera, E., Costa, E. I., Segura-Camacho, A., Saenz-De-la-torre, L.-C., & Mendoza-Sierra, M. I. (2022). Work–Family interaction, self-perceived mental health and burnout in specialized physicians of huelva (Spain): A study conducted during the SARS-CoV-2 pandemic. International Journal of Environmental Research and Public Health, 19(6). https://doi.org/10.3390/ijerph19063717
Garcia-Hedrera, F. J., Gil-Almagro, F., Carmona-Monge, J., Penacoba-Puente, F., Catala-Meson, C., P., & Velasco-Furlong, L. (2021). Intensive care unit professionals during the COVID-19 pandemic in Spain: Social and work-related variables, COVID-19 symptoms, worries, and generalized anxiety levels. Acute And Critical Care, 36(3), 232–241. https://doi.org/10.4266/acc.2021.00213
Gómez-Salgado, J., Domínguez-Salas, S., Romero-Martín, M., Romero, A., Coronado-Vázquez, V., & Ruiz-Frutos, C. (2021). Work engagement and psychological distress of health professionals during the COVID-19 pandemic. Journal of Nursing Management, 29(5), 1016–1025. https://doi.org/10.1111/jonm.13239
González-Mesa, E., Jiménez‐López, J. S., Blasco‐Alonso, M., Anderica‐Herrero, J. R., & Lubián‐López, D. (2021). Effects of sars‐cov‐2 pandemic on the mental health of Spanish Ob‐gyn specialists—a nationwide study. Journal of Clinical Medicine, 10(24). https://doi.org/10.3390/jcm10245899
González-Sanguino, C., Ausín, B., Castellanos, M., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behavior and Immunity, 87, 172–176. https://doi.org/10.1016/j.bbi.2020.05.040
Guillén-Astete, C., Penedo-Alonso, R., Gallego-Rodríguez, P., Carballo-Cardona, C., Estévez-Rueda, M. J., Galli-Cambiaso, E., Collado-Martín, A. S., Clemente-Bermúdez, L., & Sánchez-Gómez, C. (2020). Levels of anxiety and depression among emergency physicians in Madrid during the SARS-CoV-2 pandemic. In Emergencias: revista de la Sociedad Espanola de Medicina de Emergencias (Vol. 32, Issue 5, pp. 369–371).
INE (2023). Información estadística para el análisis del impacto de la crisis COVID-19. Instituto Nacional de Estadística (España). https://ine.es/covid/covid_salud.htm
Jiménez-Labaig, P., Pacheco-Barcia, V., Cebrià, A., Gálvez, F., Obispo, B., Páez, D., Quílez, A., Quintanar, T., Ramchandani, A., Remon, J., Rogado, J., Sánchez, D. A., Sánchez-Cánovas, M., Sanz-García, E., Sesma, A., Tarazona, N., Cotés, A., González, E., & Bosch-Barrera, J. (2021). … lez, E. Identifying and preventing burnout in young oncologists, an overwhelming challenge in the COVID-19 era: a study of the Spanish Society of Medical Oncology (SEOM). ESMO Open, 6(4). https://doi.org/10.1016/j.esmoop.2021.100215
Kang, L., Ma, S., Chen, M., Yang, J., Wang, Y., Li, R., Yao, L., Bai, H., Cai, Z., Yang, X., Hu, B., Zhang, S., Wang, K., Ma, G., C., & Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behavior and Immunity, 87(March), 11–17. https://doi.org/10.1016/j.bbi.2020.03.028
Kang, L., Li, Y., Hu, S., Chen, M., Yang, C., Yang, B. X., & Wang, Y. (2021). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14.
Kersting, C., Zimmer, L., Thielmann, A., & Weltermann, B. (2019). Chronic stress, work-related daily challenges and medicolegal investigations: A cross-sectional study among German general practitioners. BMC Family Practice, 20(1), 143. https://doi.org/10.1186/s12875-019-1032-6
Koinis, A., Giannou, V., Drantaki, V., Angelaina, S., Stratou, E., & Saridi, M. (2015). The impact of healthcare workers job environment on their mental-emotional health. Coping strategies: The case of a local general hospital. Health Psychology Research, 3(1), 1984. https://doi.org/10.4081/hpr.2015.1984
Lara-Cabrera, M. L., Betancort, M., Muñoz-Rubilar, C. A., Novo, N. R., & De las Cuevas, C. (2021). The mediating role of resilience in the relationship between perceived stress and mental health. International Journal of Environmental Research and Public Health, 18(18). https://doi.org/10.3390/ijerph18189762
Lee, A. M., Wong, G. W. S., McAlonan, J., Cheung, G. M., Cheung, V., Sham, C., Chu, P. C., Wong, C. M., Tsang, P. C., K. W., & Chua, S. E. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. In The Canadian Journal of Psychiatry (Vol. 52, Issue 4).
Luceño-Moreno, L., Talavera-Velasco, B., García-Albuerne, Y., & Martín-García, J. (2020). Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(15), 1–29. https://doi.org/10.3390/ijerph17155514
Lykkegaard, J., Prior, A., & Rosendal, M. (2020). General practitioners’ management of patients with psychological stress: Audit results from Denmark. BMC Family Practice, 21(1), 67. https://doi.org/10.1186/s12875-020-01137-6
Maben, J., Adams, M., Peccei, R., Murrells, T., Robert, G., & Morrow, E. (2012). Improving the quality of care in care homes using an intervention focused on relationship-centred care: Results from a cluster randomised controlled trial. Age and Ageing, 41(5), 571–578.
Macía-Rodríguez, C., De Oña, A., Martín-Iglesias, Á., Barrera-López, D., Pérez-Sanz, L., Moreno-Diaz, M. T., J., & González-Munera, A. (2021). Burn-out syndrome in Spanish internists during the covid-19 outbreak and associated factors: A cross-sectional survey. British Medical Journal Open, 11(2). https://doi.org/10.1136/bmjopen-2020-042966
Mak, I. W. C., Chu, C. M., Pan, P. C., Yiu, M. G. C., & Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry, 31(4), 318–326. https://doi.org/10.1016/j.genhosppsych.2009.03.001
Manzanares, I., Sevilla Guerra, S., Lombraña Mencía, M., Acar-Denizli, N., Salmerón, M., J., & Estalella, M., G (2021). Impact of the COVID-19 pandemic on stress, resilience and depression in health professionals: A cross-sectional study. International Nursing Review, 68(4), 461–470. https://doi.org/10.1111/inr.12693
Martín, J., Padierna, Á., Villanueva, A., & Quintana, J. M. (2021). Evaluation of the mental health of care home staff in the Covid-19 era. What price did care home workers pay for standing by their patients? International Journal of Geriatric Psychiatry, 36(11), 1810–1819. https://doi.org/10.1002/gps.5602
Martínez-Caballero, C. M., Cárdaba-García, R. M., Varas-Manovel, R., García-Sanz, L. M., Martínez-Piedra, J., Fernández-Carbajo, J. J., Pérez-Pérez, L., Madrigal-Fernández, M. A., Barba-Pérez, M., Olea, E., Durantez-Fernández, C., & Herrero-Frutos, M. T. (2021). Analyzing the impact of COVID-19 trauma on developing post-traumatic stress disorder among emergency medical workers in Spain. International Journal of Environmental Research and Public Health, 18(17). https://doi.org/10.3390/ijerph18179132
Martínez-López, J., Lázaro-Pérez, C., & Gómez-Galán, J. (2021). Burnout among direct-care workers in nursing homes during the covid-19 pandemic in Spain: A preventive and educational focus for sustainable workplaces. Sustainability (Switzerland), 13(5), 1–15. https://doi.org/10.3390/su13052782
Maslach C. & Jackson S. E. (1982). Burnout in health care professions: A social psychological analysis. In G. Sanders & J. Suls (Eds.), Social Psychology of Health and Illness (pp. 227–251). Erlbaum.
Matalí-Costa, J., & Camprodon-Rosanas, E. (2022). COVID-19 lockdown in Spain: Psychological impact is greatest on younger and vulnerable children. Clinical Child Psychology and Psychiatry, 27(1), 145–156. https://doi.org/10.1177/13591045211055066
Mediavilla, R., Fernández-Jiménez, E., Martinez-Morata, I., Jaramillo, F., Andreo-Jover, J., Morán-Sánchez, I., Mascayano, F., Moreno-Küstner, B., Minué, S., Ayuso-Mateos, J. L., Bryant, R. A., Bravo-Ortiz, M. F., & Martínez-Alés, G. (2022). Sustained negative mental health outcomes among healthcare workers over the first year of the COVID-19 pandemic: A prospective cohort study. International Journal of Public Health, 67. https://doi.org/10.3389/ijph.2022.1604553
Mediavilla, R., Fernández-Jiménez, E., Martínez-Alés, G., Moreno-Küstner, B., Martínez-Morata, I., Jaramillo, F., Morán-Sánchez, I., Minué, S., Torres-Cantero, A., Alvarado, R., Ayuso-Mateos, J. L., Mascayano, F., Susser, E., Bravo-Ortiz, M. F., & Group, T. C.-19 H. C. W. (C19-H. W. (2021). Role of access to personal protective equipment, treatment prioritization decisions, and changes in job functions on health workers’ mental health outcomes during the initial outbreak of the COVID-19 pandemic. Journal of Affective Disorders, 295, 405–409. https://doi.org/10.1016/j.jad.2021.08.059
Mira, J. J., Carrillo, I., Guilabert, M., Mula, A., Martin-Delgado, J., Pérez-Jover, M. V., Vicente, M. A., & Fernández, C. (2020). Acute stress of the healthcare workforce during the COVID-19 pandemic evolution: A cross-sectional study in Spain. British Medical Journal Open, 10(11). https://doi.org/10.1136/bmjopen-2020-042555
Molina-Mula, J., González-Trujillo, A., Perelló-Campaner, C., Tortosa-Espínola, S., Tera-Donoso, J., la Rosa, L. O. D., & Romero-Franco, N. (2022). The emotional impact of COVID-19 on Spanish nurses and potential strategies to reduce it. Collegian (Royal College of Nursing, Australia), 29(3), 296–310. https://doi.org/10.1016/j.colegn.2021.12.004
Moraleda-Cibrian, M., Ahmed, O., Albares-Tendero, J., & Chung, S. (2022). Validity and Reliability of the Stress and Anxiety to Viral Epidemics-6 (SAVE-6) Scale to measure viral anxiety of healthcare workers in Spain during the COVID-19 pandemic. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.796225
Oprisan, A., Baettig-Arriagada, E., Baeza-Delgado, C., & Martí-Bonmatí, L. (2022). Prevalence of burnout syndrome during the COVID-19 pandemic and associated factors. Radiologia, 64(2), 119–127. https://doi.org/10.1016/j.rx.2021.09.003
Ortega-Galan, A. M., Ruiz-Fernandez, M. D., Lirola, M. J., Ramos-Pichardo, J. D., Ibanez-Masero, O., Cabrera-Troya, J., Salinas-Perez, V., Gomez-Beltran, P. A., & Fernandez-Martinez, E. (2020). Professional quality of life and perceived stress in health professionals before COVID-19 in Spain: Primary and hospital care. Healthcare, 8(4). https://doi.org/10.3390/healthcare8040484
Ozamiz-Etxebarria, N., Dosil-Santamaria, M., Picaza-Gorrochategui, M., & Idoiaga-Mondragon, N. (2020). Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en El norte de España (p. 36). Cadernos de Saúde Pública.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., & Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372. https://doi.org/10.1136/bmj.n71
Park, J. S., Lee, E. H., Park, N. R., & Choi, Y. H. (2018). Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Archives of Psychiatric Nursing, 32(1), 2–6. https://doi.org/10.1016/j.apnu.2017.09.006
Patelarou, A., Mechili, E. A., Galanis, P., Zografakis-Sfakianakis, M., Konstantinidis, T., Saliaj, A., Bucaj, J., Alushi, E., Carmona-Torres, J. M., Cobo-Cuenca, A. I., Laredo-Aguilera, J. A., & Patelarou, E. (2021). Nursing students, mental health status during COVID-19 quarantine: Evidence from three European countries. Journal of Mental Health (Abingdon England), 30(2), 164–169. https://doi.org/10.1080/09638237.2021.1875420
Pérez-Chacón, M., Chacón, A., Borda-Mas, M., & Avargues-Navarro., M. L. (2021). Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. Environmental Research and Public Health, 18, 611.
Radha, K., George, G., Varghese, A., Joseph, J., & Vijayanarayanan, N. (2022). Prevalence of physical and psychological impacts of wearing personal protective equipment on health care workers during COVID-19: A systematic review and Meta-analysis. Indian Journal of Occupational and Environmental Medicine, 26(3), 140–150. https://doi.org/10.4103/ijoem.ijoem_32_22
Reno-Chanca, S., Van Hoey, J., Santolaya-Prego de Oliver, J. A., Blasko-Ochoa, I., Aguilar, S., P., & Moret-Tatay, C. (2021). Differences between the psychological symptoms of health workers and general community after the first wave of the COVID-19 outbreak in Spain. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.644212
Rodríguez-Rey, R., Garrido-Hernansaiz, H., & Bueno-Guerra, N. (2020). Working in the times of covid-19. Psychological impact of the pandemic in frontline workers in Spain. International Journal of Environmental Research and Public Health, 17(21), 1–23. https://doi.org/10.3390/ijerph17218149
Ruiz-Fernández, M. D., Ramos-Pichardo, J. D., Ibáñez-Masero, O., Cabrera-Troya, J., Carmona-Rega, M. I., & Ortega-Galán, Á. M. (2020). Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Journal of Clinical Nursing, 29(21–22), 4321–4330. https://doi.org/10.1111/jocn.15469
Ruiz-Frutos, C., Ortega-Moreno, M., Soriano-Tarín, G., Romero-Martín, M., Allande-Cussó, R., Cabanillas-Moruno, J. L., & Gómez-Salgado, J. (2021). Psychological distress among occupational health professionals during coronavirus disease 2019 pandemic in Spain: Description and effect of work engagement and work environment. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.765169
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., Rasoulpoor, S., & Khaledi-Paveh, B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health, 16(1), 57. https://doi.org/10.1186/s12992-020-00589-w
Sánchez-Sánchez, E., García-álvarez, J., García-Marín, E., Gutierrez-Serrano, M., Alférez, M. J. M., & Ramirez-Vargas, G. (2021). Impact of the covid-19 pandemic on the mental health of nurses and auxiliary nursing care technicians—a voluntary online survey. International Journal of Environmental Research and Public Health, 18(16). https://doi.org/10.3390/ijerph18168310
Sandín, B., Valiente, R. M., García-Escalera, J., & Chorot, P. (2020). Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al periodo de confinamiento nacional. Revista de Psicopatología y Psicología Clínica, 25(1), 1–22.
Saragih, I. D., Tonapa, S. I., Saragih, I. S., Advani, S., Batubara, S. O., Suarilah, I., & Lin, C. J. (2021). Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. International Journal of Nursing Studies, 121, 104002. https://doi.org/10.1016/j.ijnurstu.2021.104002
Seda-Gombau, G., Montero-Alía, J. J., Moreno-Gabriel, E., & Torán-Monserrat, P. (2021). Impact of the covid-19 pandemic on burnout in primary care physicians in catalonia. International Journal of Environmental Research and Public Health, 18(17). https://doi.org/10.3390/ijerph18179031
Shanafelt, T. D., Bradley, K. A., Wipf, J. E., & Back, A. L. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136(5), 358–367. https://doi.org/10.7326/0003-4819-136-5-200203050-00008
Shanafelt, T. D., Hasan, O., Dyrbye, L. N., Sinsky, C., Satele, D., Sloan, J., & West, C. P. (2015). Intentional rounding in hospital settings: A systematic review and meta-analysis. The Lancet, 386(10010), 1376–1384.
Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., & West, C. P. (2016). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 176(2), 204–213.
Sim, K., & Chua, H. C. (2004). The psychological impact of SARS: A matter of heart and mind. CMAJ: Canadian Medical Association Journal = Journal de l’Association medicale canadienne, 170(5), 811–812. https://doi.org/10.1503/cmaj.1032003
Sobregrau Sangrà, P., Aguiló Mir, S., Castro Ribeiro, T., Esteban-Sepúlveda, S., García Pagès, E., López Barbeito, B., Moya-Prats, P., Pintor, J. L., Pérez, L., & Aguiló Llobet, J. (2022). Mental health assessment of Spanish healthcare workers during the SARS-CoV-2 pandemic. A cross-sectional study. Comprehensive Psychiatry, 112, 152278. https://doi.org/10.1016/j.comppsych.2021.152278
Soto-Cámara, R., Navalpotro-Pascual, S., Jiménez-Alegre, J. J., García-Santa-basilia, N., Onrubia-Baticón, H., Navalpotro-Pascual, J. M., Thuissard, I. J., Fernández-Domínguez, J. J., Matellán-Hernández, M. P., Pastor-Benito, E., Polo-Portes, C. E., & Cárdaba-García, R. M. (2022). Influence of the cumulative incidence of COVID-19 cases on the mental health of the Spanish out-of-hospital professionals. Journal of Clinical Medicine, 11(8), 2227. https://doi.org/10.3390/jcm11082227
Tomalá León, M. L., Domínguez, G., Maza Santos, Y., E. H.&, & Villamar Guale, J. A. (2021). Factores De Riesgo Psicosocial Y salud mental Del personal de salud en ámbito hospitalario. Revista Científica Higía De La Salud, 4(1). https://doi.org/10.37117/higia.v1i4.491
Torrente, M., Sousa, P. A. C., Sánchez-Ramos, A., Pimentao, J., Royuela, A., Franco, F., Collazo-Lorduy, A., Menasalvas, E., & Provencio, M. (2021). To burn-out or not to burn-out: A cross-sectional study in healthcare professionals in Spain during Covid-19 pandemic. British Medical Journal Open, 11(2), e044945.
Wang, C., López-Núñez, M. I., Pan, R., Wan, X., Tan, Y., Xu, L., Choo, F., Ho, R., Ho, C., & Aparicio García, M. E. (2021). The impact of the COVID-19 pandemic on physical and mental health in China and Spain: Cross-sectional study. JMIR Form Res, 5(5), e27818. https://doi.org/10.2196/27818
Williams, E. S., Manwell, L. B., Konrad, T. R., & Linzer, M. (2007). The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: Results from the MEMO study. Health Care Management Review, 32(3), 203–212. https://doi.org/10.1097/01.HMR.0000281626.28363.59
World Health Organization. (2023). Spain: WHO Coronavirus Disease (COVID-19) dashboard with Vaccination Data. WHO Health Emergency Dashboard WHO (COVID-19.
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry, 7(3), 228–229. https://doi.org/10.1016/S2215-0366(20)30046-8
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277(June), 55–64. https://doi.org/10.1016/j.jad.2020.08.001
Zhang, Y., Wei, L., Li, H., Pan, Y., Wang, J., Li, Q., & Liu, J. (2020). The psychological change process of frontline nurses caring for patients with COVID-19 during its outbreak. Issues in Mental Health Nursing, 41(6), 525–530.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This work was supported by Generalitat Valenciana. Consellería de Educación, Universidades y Empleo. «Subvenciones para la realización de proyectos I + D + i desarrollados por grupos de investigación emergentes 2022». Proyecto CIGE/2021/102.
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
Conceptualization: Diana Castilla; Methodology and analysis: Irene Jaén and Carolina Ausín; Writing the manuscript: Irene Jaén; Review and editing the manuscript: Diana Castilla; Supervision: Diana Castilla.
Corresponding author
Ethics declarations
Ethical approval
An ethics statement is not applicable because this study is based exclusively on published literature.
Informed consent
Informed consent is not required since this work is a systematic review.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jaén, I., Ausín, C. & Castilla, D. Psychological impact of the COVID-19 pandemic on Spanish healthcare workers: a systematic review of prevalence and wave-based patterns. Curr Psychol (2023). https://doi.org/10.1007/s12144-023-05542-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s12144-023-05542-9