Abstract
Primary headache is a common somatic disorder in childhood that significantly affects quality of life. The condition is strongly associated with a variety of internalizing and externalizing disorders, and several dimensions are recognized to play a role in its development and expression, including attachment bonds. The present study aimed at exploring the associations between somatic symptoms, internalizing and externalizing problems, and attachment dimensions in a group of children and adolescents suffering from headache. The predictive effect of internalizing/externalizing problems and attachment dimensions on somatic symptoms was also explored. A sample of 50 children/adolescents with a headache diagnosis (i.e., 36 girls, 14 boys; mean age 13.18 years; SD = 2.85) participated in the study and completed the Children’s Somatization Inventory-24, the Experiences in Close Relationships Scale–Revised Child version, and a brief sociodemographic questionnaire. Mothers completed the Child Behavior Checklist 6–18. The correlational analysis revealed positive associations between child somatic symptoms and age, internalizing problems, and attachment anxiety and avoidance to the mother and the father, respectively; and a negative association between child somatic symptoms and secure attachment to the father. The regression analysis highlighted the significant effect of ECR-RC Avoidance-Father and CBCL Internalizing Problems in predicting greater somatic symptoms in young headache patients. The present findings highlight avoidant attachment to fathers and internalizing problems as risk factors for greater somatic symptoms in children/adolescents with headache. The results suggest that greater somatic symptoms in this clinical population may represent a learned maladaptive behavior to satisfy attachment needs. Clinical implications are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A primary headache diagnosis refers to the episodic or chronic occurrence of tension-type headaches, migraines, or both (Headache Classification Committee of the International Headache Society (IHS), 2018). A survey regarding chronic pain in youth found that 18.9% of respondents from the general pediatric population reported recurrent headache as their most prevalent chronic pain (Perquin et al., 2000). Indeed, headache is one of the most common somatic complaints in children and adolescents and its prevalence is estimated to be 10–20% in the school-age population, showing a progressive increase with age. Research has found that, among 13- to 14-year-olds, 27–32% experience headache at least once a month and 87–94% experience headache at least once a year (Bellini et al., 2013; Powers et al., 2006).
In children, headache can negatively affect several aspects of functioning, pertaining to both affective states (i.e., anxiety, depression, anger) and psychosocial dimensions (i.e., school attendance, peer and social interactions), determining a poor quality of life (Bellini et al., 2013; Faedda et al., 2016; Powers et al., 2006). Children and adolescents who experience headache are more likely to report other somatic symptoms, anxiety, and mood disorders, and to demonstrate behavioral problems (Balottin et al., 2013; Bruijn et al., 2010; Galli et al., 2007). Some studies, has shown that children with migraine had significantly higher levels of internalizing and somatic symptoms, as well as social and family problems compared to those without headache (Anttila et al., 2004; Arruda & Bigal, 2012; Margari et al., 2013; Natalucci et al., 2018). Guidetti et al. (1986) identified the presence of feelings of exclusion from the family group and repressed hostility toward important figures in children with migraine. Pitrou et al. (2010) found positive associations between headaches, emotional disorders, and comorbid physical conditions in children aged 6–11 years old. Moreover, in Margari et al. (2013) 26% of the children with headache reporting psychiatric comorbidity such as anxiety and mood disorders. Both psychological symptoms and environmental factors have been found to influence the onset, exacerbation, and maintenance of headache (Arruda et al., 2010; Tarantino et al., 2017). Therefore, internalizing and externalizing problems may contribute to manifesting headache and other somatic symptoms as expressions of psychological suffering.
On the side of environmental factors, dysfunctional family systems and attachment experiences/patterns may be considered most significant (Guidetti et al., 2019). According to Bowlby, the attachment system is formed during early childhood, based upon children’s interactions with primary caregivers (Bowlby, 1969). Through these interactions, children develop internal working models, or cognitive schemas regarding the self and others. These models influence children’s thoughts, emotional responses, and interpersonal relationships as they age, into adulthood. Additionally, children’s attachment patterns influence their ways of coping with threat and challenge, including the pain arising from headache (Arruda et al., 2010). Ideally, primary caregivers are sensitive and available, thereby determining a sense of attachment security in children that promotes positive psychological outcomes, even in the context of adversity (e.g., pain, illness) (Ciechanowski et al., 2003). Indeed, children with secure attachment tend to be supported in their efforts to manage the negative emotions that arise in the context of significant health issues (Bizzi et al., 2021).
Conversely, children whose parents are inconsistent in response to their attachment needs may develop insecure attachment patterns. Such patterns tend to have negative consequences for both physical and mental health. As regards this clinical population, preliminary investigations have highlighted that the frequency and severity of headache are associated with insecure attachment dimensions (Berry & Drummond, 2014). Esposito et al. (2013) identified higher rates of insecure-dismissing attachment in a sample of school-aged children with headache, and Tarantino et al. (2017) and Faedda et al. (2016) found a prevalence of preoccupied attachment styles among children reporting a high attack frequency and severe pain. These findings suggest that an ambivalent attachment style may be a vulnerability factor that impacts pain severity, anxiety, depression, and somatization symptoms in children with headache (Tarantino et al., 2017).
Williams et al. (2017) found lower attachment security in a clinical group than a control group, and higher scores on all anxiety scales in the clinical group, with children’s attachment to their mother mediating their increase in global anxiety. Bizzi et al. (2021) found a greater percentage of insecure-preoccupied attachment to both parents in adolescents with primary headache, as well as higher levels of preoccupied anger (particularly toward the father) relative to healthy controls, suggesting that parent–child interaction may play a key role in contributing to primary headache in early adolescents. Finally, Barone et al. (2016) found that children’s perceived attachment security was associated with a weaker link between maternal stress and externalizing problems, suggesting that secure attachment may represent a protective factor in the management of painful and negative emotions associated with health issues.
It should be also noted that on March 2020, the spread of Coronavirus Disease 19 (COVID-19) pandemic and related consequences have exposed children and adolescents to their first great stressful community event (Caffo et al., 2021). In this light, also parents have experience a high distress and an increment in psychopathological diseases has been documented (Amerio et al., 2021). During lockdowns periods children had only their parents to provide support, but the highly distressful experience of pandemic may have potentially impaired their ability to be reassuring caregivers (Spinelli et al., 2021). After COVID-19 pandemic outbreak, psychological and physical health as well as the quality of life of children and adolescents worsened as testified by the evidence of neurovegetative and somatic symptoms as headache (Garcia-Adasme et al., 2021; Nobari et al., 2021; Renzi et al., 2022).
To the best of our knowledge, no previous study has jointly explored children’s attachment styles with both parents, children’s tendency to report somatic symptoms, and parents’ perceptions of their children’s internalizing/externalizing problems, in a sample of child headache patients.
The present study aimed at exploring the associations between somatic symptoms, internalizing/externalizing problems, and attachment dimensions in a group of children and adolescents suffering from headache. The considered internalizing problems were anxious/depressed, withdrawn-depressed, and somatic complaints; and the considered externalizing problems were rule-breaking and aggressive behavior. A further aim was to explore the predictive effect of internalizing and externalizing problems and attachment dimensions on somatic symptoms, to identify possible protective/risk factors associated with greater somatic symptoms. In accordance with the broader literature, we hypothesized that a positive association between symptomatic dimensions and attachment dimensions would emerge in the direction of higher symptomatology associated to higher scores of insecure attachment dimensions as well as lower symptoms associated to higher scores of secure attachment dimension. Moreover, we expected a significant effect of internalizing problems and insecure attachment scores on somatic symptoms reported by children and adolescents.
Methods
Participants and procedure
The present investigation was conducted between November 29 and December 21, 2022, in accordance with the code of ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Ethical approval was granted by the Ethics Committee of the Department of Dynamic and Clinical Psychology at Sapienza University of Rome (Prot. n. 0001990). Informed consent was obtained by all participants and their parents.
Participants were children recruited from the patient roster of the Centre for the Diagnosis and Treatment of Pediatric Headache of the Sant’Andrea Hospital of Rome, according to the following inclusion criteria: (a) headache diagnosis according to the International Classification for Headache Disorder (ICHD-III), (b) aged 8–18 years, and (c) able to adequately understand the Italian language. Patients with an inadequate understanding of the Italian language and patients who reported a history of another neurological disorder were excluded. A physician screened children for eligibility during the initial clinical interview, then the physician introduced the eligible children and their parents to the psychologist responsible for implementing the research protocol. Prior to completing the study questionnaires, patients consented to participation and their parents signed an informed consent form. The entire research protocol took place at the headache treatment center in the presence of the psychologist.
Fifty-four consecutive patients were invited to participate, and four declined, due to time constraints. No patient was excluded due to a neurological disorder or language difficulty. Fifty children/adolescents (i.e., 36 girls, 14 boys) participated in the study with a mean age of 13.18 years (SD = 2.85; range: 8–17) and a mean age at diagnosis of 10.92 years (SD = 3.84). All children lived with both parents and 66% had at least one sibling (see Table 1).
Measures
Sociodemographic questionnaire
A sociodemographic questionnaire was designed to collect information on children’s age, gender, age at the time of diagnosis, pain intensity (from 0 to 10), headache diagnosis, and siblings (i.e., present or absent).
Child behavior checklist 6–18
The Child Behavior Checklist 6–18 (CBCL 6–18) (Achenbach et al., 2002; Frigerio et al., 2004) assess child and adolescent psychopathology. The 113-item informant-report questionnaire asks parents to rate specific emotional-behavioral problems in their child over the prior 6 months. Items are grouped into eight syndrome subscales that can be combined into two broader subscales: Internalizing Problems (comprised of items from the Anxious/Depressed, Withdrawn-Depressed, and Somatic Complaints subscales) and Externalizing Problems (comprised of items from the Rule-Breaking and Aggressive Behavior subscales). The present study only considered these broader subscales. In the present study internal consistency was satisfactory for both Externalizing Problems (Cronbach’s α = 0.83) and Internalizing Problems (Cronbach’s α = 0.85).
Children’s somatization Inventory-24
The Children’s Somatization Inventory-24 (CSI-24) (Cerutti et al., 2017; Walker et al., 2009) is a 24 items test employed to evaluate children’s perception of somatic symptoms or complaints over the prior 2 weeks. Higher scores indicate higher levels of somatic symptoms. This measure showed adequate reliability and validity in both the original (Walker et al., 2009) and the Italian (Cerutti et al., 2017) versions. In the present study, Cronbach’s alpha was 0.91.
Experiences in close relationships scale–revised child version
The Experiences in Close Relationships Scale–Revised Child version (ECR-RC) (Lionetti et al., 2018) is a 12 items test assessing attachment in children and adolescents. Items are grouped into three subscales: Anxiety, Avoidance, and Security. In the present study, internal consistency was satisfactory for Anxiety (Cronbach’s α = 0.85 and 0.80 for mothers and fathers, respectively), Avoidance (Cronbach’s α = 0.83 and 0.85 for mothers and fathers, respectively), and Security (Cronbach’s α = 0.78 and 0.83 for mothers and fathers, respectively).
Statistical analyses
All statistical analyses were executed using the Statistical Package for Social Science version 25 for Windows (SPSS version 25; IBM, Armonk, NY, USA). Data were reported as frequency and percentage values for the discrete variables and means and standard deviations for the continuous variables. Pearson’s correlation analysis was conducted to measure the associations between somatic symptoms, internalizing and externalizing problems, attachment dimensions, age, and gender. Assumptions for linear regression were tested and no significant violations emerged. Three multiple regression models were performed to investigate: (1) the role of attachment dimensions regarding both mothers and fathers and (2) the effect of internalizing and externalizing problems on somatic symptoms. A third model was tested using the variable showing significance in the previous regression models, while also adding age and gender. All independent variables were entered simultaneously. A p < .05 was considered significant.
A posteriori power analysis was performed through the G*Power 3.1.9.2 programme to detect information about the effect size of the analysis performed with our limited sample. It has been evaluated that 50 subject allowed to detect effect with an effect size f of 0.30 a power of 80% and assuming an α of.05.
Results
The correlational analysis confirmed several significant associations (see Table 2). Specifically, children’s somatization showed several significant—and moderate to strong—positive associations were between CSI-24 scores and age (r = .486; p = .001); attachment anxiety (r = .558; p = .001; r = .415; p = .005), and avoidance (r = .569; p = .001; r = .654; p = .001) to the mother and father, respectively; and internalizing problems (r = .459; p = .003). Significant—and moderate to strong—negative associations were found between CSI-24 scores and secure attachment to the father (r=-.334; p = .029) and gender (r=-.353; p = .016), with girls showing greater somatic symptomatology.
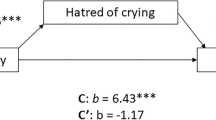
Two multiple linear regression models were tested using somatization as a dependent variable and attachment dimensions regarding mothers and fathers (first model) and internalizing and externalizing problems (second model), respectively, as independent variables (see Table 3). The first model explained 49.3% of the variance in the CSI-24 total score (R2 = 0.49; adjusted R2 = 0.41; p < .001), and only ECR-RC Avoidance-Father (beta = 0.574; p = .045) showed a significant effect. The second model explained 21% of the variance in the CSI-24 total score (R2 = 0.21; adjusted R2 = 0.18), and only CBCL Internalizing Problems showed a significant effect (beta = 0.455; p = .003).
A third model, using the variable showing a significant effect in the preceding models (i.e., ECR-RC Avoidance-Father, CBCL Internalizing Problems) was run, with the addition of age and gender. This third model explained 53% of the variance in the CSI-24 total score (R2 = 0.53; adjusted R2 = 0.49) and confirmed the significant effect of both ECR-RC Avoidance-Father (beta = 0.479; p = .001) and CBCL Internalizing Problems (beta = 0.242; p = .045) (see Table 3).
Discussion
In the present study, positive associations emerged between somatic symptoms, internalizing problems, and avoidant and anxiety attachment to both parents. Moreover, an inverse association was found between somatic symptoms and secure attachment to fathers, in the direction of less somatic symptoms with higher levels of secure attachment to fathers. Both internalizing problems and attachment dimensions emerged as significant predictors of a greater children’s somatic symptomatology. However, contrary to the expectations, only avoidant attachment to fathers emerged as a significant factor, and no attachment dimensions associated with mothers.
The present findings are aligned with previous research highlighting strong associations between headache, internalizing disorders (e.g. depression, social withdraw), and specific psychophysiological correlates (Valeriani et al., 2009). In this vein, studies have demonstrated that somatic symptoms are common in adolescents suffering from depression, and this psychiatric comorbidity tend to be more depth and severe in duration (Bair et al., 2004; Bohman et al., 2010; Geerlings et al., 2002; Ohayon & Schatzberg, 2003). Similar findings have emerged with respect to anxiety, with children and adolescents suffering from anxiety disorders reporting higher rates of somatic symptoms compared to controls (Ginsburg et al., 2006). Moreover, more somatic symptoms have been associated with more severe anxiety disorders (Ginsburg et al., 2006). Finally, the present finding of an association between insecure attachment patterns and greater somatic symptoms in children and adolescents suffering from headache seems to confirm previous findings in normal and clinical school-age populations (Beck, 2007; Bizzi et al., 2019; Stuart & Noyes, 1999).
The finding regarding the role of avoidant attachment to fathers as significant predictor of a greater somatic symptomatology in children is particularly interesting, since it underlines the role of fathers and the importance of evaluating attachment to fathers in this specific population. It seems plausible that children with headache who perceive their fathers as insensitive and unavailable may experience less closeness to them, and this may represent a specific risk factor for the development of greater somatic symptoms. In this light, the greater manifestation of somatic symptoms may be considered a possible expression of an unconscious need for care from and proximity to fathers. Through a developmental psychopathology perspective, a child’s somatic symptoms or disorders may aim at generating closer proximity to an attachment figure (Bowlby, 1969), with expressions of physical discomfort operating to elicit care (Campo et al., 1999; Campo & Fritsch, 1994). In this direction, attachment theory and physiological studies highlighting functional somatic symptoms in children emphasize the importance of the parent–child relationship and caregiving environment on the development of somatic disorders (Beck, 2007; Bowlby, 1969; Gunnar & Donzella, 2002). In fact, experiences of chronic illness, particularly during childhood, may reinforce care-seeking behavior (Stuart & Noyes, 1999). More specifically, chronic pain (e.g., headache, somatic symptoms) requires the individual and their significant others to establish and maintain many illness-related behaviors; this may induce the use of maladaptive methods (i.e., expressions of emotional discomfort through somatic symptoms) to satisfy attachment needs (Beck, 2007; Stuart & Noyes, 1999).
Several limitations of the present study should be considered in the interpretation of the results. First, the restricted sample size may limit the generalizability of the results. Furthers studies with a greater number of participants are needed to performed more sophisticated analysis as well as to obtain findings with a greater effect size so improving the relevance of the results. Second, the data collection relied on self-report measures to assess, among other factors, attachment. The use of self-report measures introduces potential bias as those related to the social desirability (i.e. parents underestimating their child’s symptoms) as well as possible difficulties in the capabilities to evaluated their own symptoms in children. Moreover, as specifically regards attachment evaluation it should be noted that it was dimensional and not categorical; thus, further research adopting a categorical approach is needed to identify the most relevant attachment style in predicting somatic symptoms in this specific clinical population. In this direction, future studies using clinical interviews to explore attachment would allow children’s and adolescents’ experiences to be recorded in greater depth (Bizzi et al., 2021). Third, several psychological and social factors (e.g., mental health status, trauma, adverse child experiences, alexithymia, parental attachment) were not considered in the analysis, and these variables may have confounded the results. Thus, further studies should include these dimensions to enrich the investigation on the variable playing a role in this filed as well as to realize more refined analysis (i.e. mediation analysis). Finally, the cross-sectional study design did not allow causal conclusions to be drawn on the observed relationships, thus longitudinal studies are needed to obtain more elucidating information on the possible role of attachment in the etiopathogenesis of headache in developmental age.
The study presents also two main strengths, the first is the examination of attachment to both parents and somatization tendency in a sample of children with a headache diagnosis in a specialized medical department. Moreover, somatization tendency was self-reported by children and adolescents, and not parent-reported, which is more common in the literature.
Conclusions
Within the context of these limitations, the present findings provide further evidence of associations between somatic symptoms, insecure attachment, and internalizing/externalizing problems, which have been insufficiently explored in the headache paediatric clinical population. Moreover, the findings emphasize the specific role played by avoidant attachment to fathers and internalizing problems in predicting greater somatic symptoms. The results suggested that greater somatic symptoms in children suffering from headache may represent maladaptive learned behavior aimed at satisfying attachment needs, especially with fathers. In this direction children may have employed to use the somatic complaints to ensure greater proximity and care from parents. In fact, when emotional needs are difficult to express and sometimes also to identify, as in the developmental age when these capabilities are in evolution, the body may represent a possible mean of expression of these affective dimensions. Moreover, parents may be more reactive and abler to respond to somatic suffering adopting a greater caregiving in this occasion. In this light, the possible result may the establishment of a maladaptive child-parents pattern. The study has significant clinical implications for health professionals working with children and adolescents with headache, highlighting the importance of attachment dimensions for understanding and intervening in this clinical population (Bizzi et al., 2019, 2021; Faedda et al., 2016). More specifically, the findings underline the importance of focused attachment-based interventions with the aim of improving child/adolescent–parent interactions, reinforcing parental skills, and promoting greater emotion regulation skills in children and adolescents (Bizzi et al., 2019), in order to reduce somatic symptoms. In fact, the implementation of programmes aimed to sustain the development of capabilities in identifying and describing emotions in children and adolescents appears essential for their health, as proved by the broader international literature highlighting the associations between alexithymic characteristics and both mental and physical diseases (Di Trani et al., 2018) as in juvenile primary headache sufferers (Gatta et al., 2011; Natalucci et al., 2018). Finally, the role of the father appears crucial, thus emphasizing the importance of involving both parents in both psychological interventions as well as in the clinical treatment of the headache. Fathers should be involved in the disease care process and in helping their children in correctly identify and express their emotional need associated to the relationship with them so preventing the process of chronicity of headache.
Data availability
The data that support the findings of this study are available upon request from the corresponding author [AR].
References
Achenbach, T. M., Dumenci, L., & Rescorla, L. A. (2002). Ten-year comparisons of problems and Competencies for National Samples of Youth: Self, parent, and teacher reports. Journal of Emotional and Behavioral Disorders, 10(4), 194–203. https://doi.org/10.1177/10634266020100040101.
Amerio, A., Lugo, A., Stival, C., Fanucchi, T., Gorini, G., Pacifici, R., Odone, A., Serafini, G., & Gallus, S. (2021). COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. Journal of Affective Disorders, 292, 398–404. https://doi.org/10.1016/j.jad.2021.05.117.
Anttila, P., Sourander, A., Metsähonkala, L., Aromaa, M., Helenius, H., & Sillanpää, M. (2004). Psychiatric symptoms in children with primary headache. Journal of the American Academy of Child & Adolescent Psychiatry, 43(4), 412–419. https://doi.org/10.1097/00004583-200404000-00007.
Arruda, M. A., & Bigal, M. E. (2012). Behavioral and emotional symptoms and primary headaches in children: A population-based study. Cephalalgia, 32(15), 1093–1100. https://doi.org/10.1177/0333102412454226.
Arruda, M. A., Guidetti, V., Galli, F., Albuquerque, R. C. A. P., & Bigal, M. E. (2010). Frequency of headaches in children is influenced by Headache Status in the mother. Headache: The Journal of Head and Face Pain, 50(6), 973–980. https://doi.org/10.1111/j.1526-4610.2010.01677.x.
Bair, M. J., Robinson, R. L., Eckert, G. J., Stang, P. E., Croghan, T. W., & Kroenke, K. (2004). Impact of Pain on Depression Treatment Response in Primary Care. Psychosomatic Medicine, 66(1), 17–22. https://doi.org/10.1097/01.PSY.0000106883.94059.C5.
Balottin, U., Fusar Poli, P., Termine, C., Molteni, S., & Galli, F. (2013). Psychopathological symptoms in child and adolescent migraine and tension-type headache: A meta-analysis. Cephalalgia, 33(2), 112–122. https://doi.org/10.1177/0333102412468386.
Barone, L., Lionetti, F., Dellagiulia, A., Galli, F., Molteni, S., & Balottin, U. (2016). Behavioural problems in children with headache and maternal stress: Is children’s attachment security a protective factor? Behavioural problems and maternal stress: The role of attachment. Infant and Child Development, 25(6), 502–515. https://doi.org/10.1002/icd.1950.
Beck, J. E. (2007). A developmental perspective on functional somatic symptoms. Journal of Pediatric Psychology, 33(5), 547–562. https://doi.org/10.1093/jpepsy/jsm113.
Bellini, B., Arruda, M., Cescut, A., Saulle, C., Persico, A., Carotenuto, M., Gatta, M., Nacinovich, R., Piazza, F. P., Termine, C., Tozzi, E., Lucchese, F., & Guidetti, V. (2013). Headache and comorbidity in children and adolescents. The Journal of Headache and Pain, 14(1), 79. https://doi.org/10.1186/1129-2377-14-79.
Berry, J. K. M., & Drummond, P. D. (2014). Does attachment anxiety increase vulnerability to headache? Journal of Psychosomatic Research, 76(2), 113–120. https://doi.org/10.1016/j.jpsychores.2013.11.018.
Bizzi, F., Ensink, K., Borelli, J. L., Mora, S. C., & Cavanna, D. (2019). Attachment and reflective functioning in children with somatic symptom disorders and disruptive behavior disorders. European Child & Adolescent Psychiatry, 28(5), 705–717. https://doi.org/10.1007/s00787-018-1238-5.
Bizzi, F., Riva, A., Charpentier Mora, S., Cavanna, D., & Nacinovich, R. (2021). Attachment representation to caregivers and mentalizing ability in early adolescents with primary headache. Clinical Psychology & Psychotherapy, 28(4), 862–871. https://doi.org/10.1002/cpp.2540.
Bohman, H., Jonsson, U., Von Knorring, A. L., Von Knorring, L., Päären, A., & Olsson, G. (2010). Somatic symptoms as a marker for severity in adolescent depression: Somatic adolescent depression. Acta Paediatrica, 99(11), 1724–1730. https://doi.org/10.1111/j.1651-2227.2010.01906.x.
Bowlby, J. (1969). Attachment and loss (Vol. 1). Basic Books.
Bruijn, J., Locher, H., Passchier, J., Dijkstra, N., & Arts, W. F. (2010). Psychopathology in children and adolescents with migraine in Clinical studies: A systematic review. Pediatrics, 126(2), 323–332. https://doi.org/10.1542/peds.2009-3293.
Caffo, E., Asta, L., & Scandroglio, F. (2021). Predictors of mental health worsening among children and adolescents during the coronavirus Disease 2019 pandemic. Current Opinion in Psychiatry, 34(6), 624–630. https://doi.org/10.1097/YCO.0000000000000747.
Campo, J. V., & Fritsch, S. L. (1994). Somatization in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 33(9), 1223–1235. https://doi.org/10.1097/00004583-199411000-00003.
Campo, J. V., Jansen-Mcwilliams, L., Comer, D. M., & Kelleher, K. J. (1999). Somatization in Pediatric Primary Care: Association with psychopathology, functional impairment, and Use of services. Journal of the American Academy of Child & Adolescent Psychiatry, 38(9), 1093–1101. https://doi.org/10.1097/00004583-199909000-00012.
Cerutti, R., Spensieri, V., Valastro, C., Presaghi, F., Canitano, R., & Guidetti, V. (2017). A comprehensive approach to understand somatic symptoms and their impact on emotional and psychosocial functioning in children. PLOS ONE, 12(2), e0171867. https://doi.org/10.1371/journal.pone.0171867.
Ciechanowski, P., Sullivan, M., Jensen, M., Romano, J., & Summers, H. (2003). The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain, 104(3), 627–637. https://doi.org/10.1016/S0304-3959(03)00120-9.
Di Trani, M., Presaghi, F., Renzi, A., Greenman, P. S., & Solano, L. (2018). The Italian version of the Alexithymia Questionnaire for Children (AQC): Factor structure and reliability. Rassegna Di Psicologia, 35, 47–60. https://doi.org/10.13133/1974-4854/16690.
Esposito, M., Parisi, L., Gallai, B., Marotta, R., Di Dona, A., Lavano, S. M., Roccella, M., & Carotenuto, M. (2013). Attachment styles in children affected by migraine without aura. Neuropsychiatric Disease and Treatment, 1513. https://doi.org/10.2147/NDT.S52716.
Faedda, N., Cerutti, R., Verdecchia, P., Migliorini, D., Arruda, M., & Guidetti, V. (2016). Behavioral management of headache in children and adolescents. The Journal of Headache and Pain, 17(1), 80. https://doi.org/10.1186/s10194-016-0671-4.
Frigerio, A., Cattaneo, C., Cataldo, M., Schiatti, A., Molteni, M., & Battaglia, M. (2004). Behavioral and emotional problems among Italian children and adolescents aged 4 to 18 years as reported by parents and teachers. European Journal of Psychological Assessment, 20(2), 124–133. https://doi.org/10.1027/1015-5759.20.2.124.
Galli, F., D’Antuono, G., Tarantino, S., Viviano, F., Borrelli, O., Chirumbolo, A., Cucchiara, S., & Guidetti, V. (2007). Headache and recurrent Abdominal Pain: A controlled study by the means of the child Behaviour Checklist (CBCL). Cephalalgia, 27(3), 211–219. https://doi.org/10.1111/j.1468-2982.2006.01271.x.
Garcia-Adasme, S. I., Cárdenas‐Rebollo, J. M., Jimenez‐Perianes, A., Lalinde, M., Jimeno, S., Ventura, P. S., Díaz, A., & López‐Escobar, A. (2021). Pediatric home confinement due to COVID‐19: Somatic and anxiety spectrum consequences. Journal of Clinical Nursing, 30(21–22), 3238–3248. https://doi.org/10.1111/jocn.15829.
Gatta, M., Canetta, E., Zordan, M., Spoto, A., Ferruzza, E., Manco, I., Addis, A., Dal Zotto, L., Toldo, I., Sartori, S., & Battistella, P. A. (2011). Alexithymia in juvenile primary headache sufferers: A pilot study. The Journal of Headache and Pain, 12(1), 71–80. https://doi.org/10.1007/s10194-010-0248-6.
Geerlings, S. W., Twisk, J. W. R., Beekman, A. T. F., Deeg, D. J. H., & van Tilburg, W. (2002). Longitudinal relationship between pain and depression in older adults: Sex, age and physical disability. Social Psychiatry and Psychiatric Epidemiology, 37(1), 23–30. https://doi.org/10.1007/s127-002-8210-2.
Ginsburg, G. S., Riddle, M. A., & Davies, M. (2006). Somatic symptoms in children and adolescents with anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 45(10), 1179–1187. https://doi.org/10.1097/01.chi.0000231974.43966.6e.
Guidetti, V., Mazzei, G., Ottaviano, S., Pagliarini, M., Paolella, A., & Seri, S. (1986). The utilization of the Rorschach Test in a case-controlled study. Cephalalgia, 6(2), 87–93. https://doi.org/10.1046/j.1468-2982.1986.0602087.x.
Guidetti, V., Cerutti, R., Faedda, N., & Natalucci, G. (2019). Migraine in childhood: An organic, biobehavioral, or psychosomatic disorder? Neurological Sciences, 40(S1), 93–98. https://doi.org/10.1007/s10072-019-03827-1.
Gunnar, M. R., & Donzella, B. (2002). Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology, 27(1–2), 199–220. https://doi.org/10.1016/S0306-4530(01)00045-2.
Headache Classification Committee of the International Headache Society (IHS). (2018). The International classification of Headache disorders, 3rd edition (Vol. 38, pp. 1–211). Cephalalgia. 1https://doi.org/10.1177/0333102417738202.
Lionetti, F., Mastrotheodoros, S., & Palladino, B. E. (2018). Experiences in Close relationships revised child version (ECR-RC): Psychometric evidence in support of a security factor. European Journal of Developmental Psychology, 15(4), 452–463. https://doi.org/10.1080/17405629.2017.1297228.
Margari, F., Lucarelli, E., Craig, F., Petruzzelli, M. G., Lecce, P. A., & Margari, L. (2013). Psychopathology in children and adolescents with primary headaches: Categorical and dimensional approaches. Cephalalgia, 33(16), 1311–1318. https://doi.org/10.1177/0333102413495966.
Natalucci, G., Faedda, N., Calderoni, D., Cerutti, R., Verdecchia, P., & Guidetti, V. (2018). Headache and Alexithymia in Children and adolescents: What is the connection? Frontiers in Psychology, 9, 48. https://doi.org/10.3389/fpsyg.2018.00048.
Nobari, H., Fashi, M., Eskandari, A., Villafaina, S., Murillo-Garcia, Á., & Pérez-Gómez, J. (2021). Effect of COVID-19 on Health-Related Quality of Life in adolescents and children: A systematic review. International Journal of Environmental Research and Public Health, 18(9), 4563. https://doi.org/10.3390/ijerph18094563.
Ohayon, M. M., & Schatzberg, A. F. (2003). Using Chronic Pain to predict depressive morbidity in the General Population. Archives of General Psychiatry, 60(1), 39. https://doi.org/10.1001/archpsyc.60.1.39.
Perquin, C. W., Hazebroek-Kampschreur, A. A. J. M., Hunfeld, J. A. M., van Suijlekom-Smit, L. W. A., Passchier, J., & van der Wouden, J. C. (2000). Chronic Pain among children and adolescents: Physician Consultation and Medication Use. The Clinical Journal of Pain, 16(3), 229–235. https://doi.org/10.1097/00002508-200009000-00008.
Pitrou, I., Shojaei, T., Chan-Chee, C., Wazana, A., Boyd, A., & Kovess-Masféty, V. (2010). The associations between headaches and psychopathology: A Survey in School children: November/December 2010. Headache: The Journal of Head and Face Pain, 50(10), 1537–1548. https://doi.org/10.1111/j.1526-4610.2010.01781.x.
Powers, S. W., Gilman, D. K., & Hershey, A. D. (2006). Headache and psychological functioning in children and adolescents. Headache: The Journal of Head and Face Pain, 46(9), 1404–1415. https://doi.org/10.1111/j.1526-4610.2006.00583.x.
Renzi, A., Conte, G., & Tambelli, R. (2022). Somatic, emotional and behavioral symptomatology in children during COVID-19 pandemic: The role of children’s and parents’ Alexithymia. Healthcare, 10(11), 2171. https://doi.org/10.3390/healthcare10112171.
Spinelli, M., Lionetti, F., Setti, A., & Fasolo, M. (2021). Parenting stress during the COVID-19 outbreak: Socioeconomic and environmental risk factors and implications for children emotion regulation. Family Process, 60(2), 639–653. https://doi.org/10.1111/famp.12601.
Stuart, S., & Noyes, R. (1999). Attachment and interpersonal communication in somatization. Psychosomatics, 40(1), 34–43. https://doi.org/10.1016/S0033-3182(99)71269-7.
Tarantino, S., De Ranieri, C., Dionisi, C., Gagliardi, V., Paniccia, M. F., Capuano, A., Frusciante, R., Balestri, M., Vigevano, F., Gentile, S., & Valeriani, M. (2017). Role of the attachment style in determining the Association between Headache Features and psychological symptoms in Migraine Children and adolescents. An Analytical Observational Case-Control Study: Headache. Headache: The Journal of Head and Face Pain, 57(2), 266–275. https://doi.org/10.1111/head.13007.
Valeriani, M., Galli, F., Tarantino, S., Graceffa, D., Pignata, E., Miliucci, R., Biondi, G., Tozzi, A., Vigevano, F., & Guidetti, V. (2009). Correlation between abnormal brain excitability and emotional symptomatology in Paediatric Migraine. Cephalalgia, 29(2), 204–213. https://doi.org/10.1111/j.1468-2982.2008.01708.x.
Walker, L. S., Beck, J. E., Garber, J., & Lambert, W. (2009). Children’s somatization inventory: Psychometric properties of the revised form (CSI-24). Journal of Pediatric Psychology, 34(4), 430–440. https://doi.org/10.1093/jpepsy/jsn093.
Williams, R., Leone, L., Faedda, N., Natalucci, G., Bellini, B., Salvi, E., Verdecchia, P., Cerutti, R., Arruda, M., & Guidetti, V. (2017). The role of attachment insecurity in the emergence of anxiety symptoms in children and adolescents with migraine: An empirical study. The Journal of Headache and Pain, 18(1), 62. https://doi.org/10.1186/s10194-017-0769-3.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. FG received financial support for this research from university funds, within the SEED National Programme for Research (PNR).
Author information
Authors and Affiliations
Contributions
Conceptualization, A.R. and F.G.; methodology, A.R., F.G., and F.L.; formal analysis, A.R. and F.G; investigation, O.B, and P.P.; resources, O.B, P.P., and F.G; data curation, A.R. and F.G; writing—original draft preparation, A.R., F.G., and F.L.; writing—review and editing, A.R., F.G., F.L. O.B., and P.P; supervision, O.B, P.P., and F.G; project administration, F.G.; funding acquisition, F.G. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional review board statement
The present study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Department of Dynamic and Clinical Psychology and Health Studies (Prot. n. 0001990–25/11/2022).
Informed consent
Informed consent was obtained from all subjects involved in the study (children and parents).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Renzi, A., Lionetti, F., Bruni, O. et al. Somatization in children and adolescents with headache: the role of attachment to parents. Curr Psychol 43, 14358–14366 (2024). https://doi.org/10.1007/s12144-023-05466-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-05466-4