Abstract
Chronotypes are diversely associated with sleep quality and mental health. Eveningness is generally associated with lower sleep quality and with increased risk for mental health complaints. Along with insomnia symptoms, frequent dysphoric dreams might be key elements of disturbed sleep, and may also indicate psychological imbalance. Our cross-sectional online study aimed to examine whether eveningness can be considered as an independent risk factor of poor mental well-being or whether this association is explained by symptoms of insomnia. Secondly, we examined the associations between eveningness and frequent dysphoric dreaming taking into account the influence of mental well-being and insomnia complaints. Method: We released an online survey with Morningness-Eveningness Questionnaire, Athens Insomnia Scale, General Mental Health, and frequency of dysphoric dreaming: nightmares and bad dreams separately. We analyzed the data of 2077 participants (MAGE = 28.5, SD = 9.6). Eveningness showed a weak but independent association with mental well-being. Additional analyses showed no signs of associations between eveningness and dysphoric dreaming, such as nightmares and bad dreams. The frequency of bad dreams was associated with insomnia complaints and mental well-being, but nightmare frequency was only linked to insomnia symptoms, but not to mental well-being. Insomnia complaints emerged as a more robust factor in poorer mental well-being than the eveningness preference. Eveningness was not associated with dysphoric dreaming. Restoring insomnia might be essential in individuals at risk for mental health complaints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
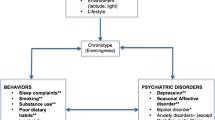
Daily preference as part of the sleep–wake cycle shows considerable individual differences within the continuum between extreme morning and extreme evening preference (Natale & Cicogna, 2002). Distinguishing between three categories (aka chronotypes) – morning, neither or intermediate, and evening -, is also widespread in the literature (Adan, 1994; Gaspar-Barba et al., 2009; Giampietro & Cavallera, 2007; Ong et al., 2007). Chronotype is primarily determined by internal (including genetic) factors (Archer et al., 2003); however, it is also influenced by environmental zeitgebers (e.g. light-, nutrition- and temperature-related changes and rhythms; Roenneberg & Merrow, 2007) and behavior (Roenneberg et al., 2003). Beyond chronotype, a wide range of physiological processes are also subjected to strong circadian modulation (Hidalgo et al., 2009; Wilson, 1990) and characterized by remarkably different diurnal rhythms across individuals with different chronotypes (See Adan et al., 2012 for an extensive review).
Evening-type individuals prefer later wake-up and bedtimes, as well as later daytime periods for mental and physical activities in comparison with morning-types (Adan et al., 2012). A large body of studies revealed that beyond the timing of daily activities, evening and morning-type individuals show differences in psychological dimensions such as personality traits. For instance, morningness is associated with higher level of introversion (Wilson, 1990), emotional stability (DeYoung et al., 2007; Tonetti et al., 2009), conscientiousness (Lázár et al., 2012; Tonetti et al., 2009), and agreeableness (Lázár et al., 2012). Morningness is also regarded as a protective factor against a variety of mental health problems (Fabbian et al., 2016; Jeon & Lee, 2019; Kivelä et al., 2018; Takeuchi et al., 2015; Taylor & Hasler, 2018).
In contrast, eveningness appears weakly, but consistently associated with negative psychological outcomes such as addiction (Prat & Adan, 2011), symptoms of depression (Hidalgo et al., 2009; Nguyen et al., 2019; Wittmann et al., 2006) and symptom severity among depressed patients (Chan et al., 2014; Emens et al., 2009; Levandovski et al., 2011), bipolar disorder (Melo et al., 2017), and seasonal affective disorder (Sandman et al., 2016). Overall, the reverse association between eveningness and mental well-being is widely accepted in the literature.
Eveningness is also related to impaired sleep quality as reflected by insufficient sleep and problems with initiating and maintaining sleep (Chan et al., 2014; Yazdi et al., 2014), daytime sleepiness (Núñez et al., 2019; Ong et al., 2007; Simor et al., 2015), and more frequent use of medication to improve sleep (Merikanto et al., 2012). Moreover, evening-type persons’ sleep duration was reported to be extended on weekends, probably to cover the deficit of weekday’s sleep (Randler et al., 2017). Evening-type individuals might be more exposed to social jetlag (Wittmann et al., 2006), which may contribute to daytime difficulties, hence, to negative mental health (Levandovski et al., 2011).
A number of previous studies indicate that impaired sleep might mediate the association between eveningness and mental health complaints (Levandovski et al., 2011; Tavernier & Willoughby, 2014); others, however, suggest that eveningness might be a partially independent risk factor for poor mental health regardless of sleep complaints (Simor et al., 2015).
Beyond insomnia, eveningness was also associated with disturbed dreaming, in particular with increased nightmare frequency (Merikanto et al., 2012; Nielsen, 2010), and dream anxiety (i.e. distress caused by frequent nightmares) (Selvi et al., 2012). Although nightmares (i.e. negative dreams followed by abrupt awakenings) and bad dreams (i.e. unpleasant dreams without awakenings) have received less research attention than insomnia complaints, they are nevertheless non-negligible from a clinical point of view: according to a meta-analysis, their prevalence in the population is 2–6% (Schredl & Reinhard, 2011). In our study we assessed the frequency of dysphoric dreams, which covers increased nightmare and/or bad dream frequency (Zadra & Donderi, 2000). Nightmare and bad dream frequency are associated with impaired sleep (Lancee et al., 2010; Li et al., 2010; Paul et al., 2015) and a wide variety of pathological conditions, such as dissociative disorders (Agargun et al., 2003; Levin & Nielsen, 2007), psychotic symptoms (Sheaves et al., 2016), and even increased risk for suicidal behaviour (Sjöström et al., 2009; Tanskanen et al., 2001). Nevertheless, it is not clear whether eveningness is associated with disturbed dreaming beyond the influence of impaired sleep and mental well-being, or whether the association between eveningness and disturbed dreaming can be accounted for by impaired sleep and mental well-being linked to eveningness.
The aim of our study was to corroborate and extend previous findings with respect to the associations between eveningness, insomnia complaints and dream quality, and mental well–being. More specifically, we examined if eveningness was associated with mental well-being above and beyond the influence of insomnia complaints. Our first hypothesis was that eveningness is associated with poorer mental well-being, regardless of the effect of insomnia complaints. Therefore, we performed hierarchical regression models to examine the association between eveningness and mental well-being after controlling for the association between insomnia and mental well-being. Additionally, we examined whether eveningness was associated with increased nightmare and/or bad dream frequency above and beyond the influence of impaired sleep and mental well-being; more specifically, we hypothesized that eveningness was associated with frequent nightmares and/or bad dreams regardless of the influence of insomnia complaints and mental well-being. Since we collected the data cross-sectionally, the independent effect of eveningness was inspected after controlling for (regressing out) the associations of insomnia symptoms and mental well-being with dysphoric dreaming.
Method
Participants and procedure
The present study included 2716 individuals who completed an online questionnaire that was made available on a Hungarian news portal. Data were collected in two periods; it started in 2016 and continued in 2019. In the second period, the questionnaire was sent to students of a university via e-mail and was shared on social media platforms as well. The data of those participants who reported prior or current neurological, psychiatric, or chronic somatic disorders (e.g. diabetes), the intake of medication known to alter sleep, or the daily consumption of alcoholic beverages were not included in the analysis. This way, we analyzed the data of 2077 individuals (1420 females, 68.4% of the whole sample). The data set was complete with the exception of the age of one participant. The age of the subjects ranged from 18 to 69 year (mean = 28.5, SD = 9.6). The participants had varied educational qualifications, including elementary school (N = 15), vocational school (N = 29), graduated from the high school (N = 485), graduated from the college (N = 293), graduated from the university (N = 664), university student (N = 591). The study has been approved by the United Ethical Review Board for Psychological Experiments (EBKEP, Hungary); all participants gave informed consent before completing the questionnaire. The study was conducted in accordance with the Declaration of Helsinki.
Questionnaires
Morningness-Eveningness Questionnaire (MEQ-H)
To assess participants' chronotype, we used the 13-item Hungarian version of the Horne-Östberg Morningness-Eveningness Questionnaire (Horne & Östberg, 1976; Zavecz et al., 2015). The 19-item original scale is commonly used to measure individual differences in morningness-eveningness preference. The items focus on the sleep–wake schedules individuals find ideal for themselves in addition to peak times for intellectually or physically demanding activities. On the morningness-eveningness continuum, higher scores reflect increased morningness. The 13-item Hungarian version of the questionnaire showed excellent internal consistency, test–retest reliability and adequate validity indices in previous studies (Simor & Polner, 2017; Simor et al., 2015; Zavecz et al., 2015). The MEQ-H can be used as a continuous measure, but it is also applicable for the differentiation of early and late chronotypes based on the first and last quartiles of the MEQ-H scores, respectively (Simor et al., 2015; Zavecz et al., 2015). In the present study we used the continuous form of the scale. The internal consistency (Cronbach's α coefficient) was 0.853.
Athen Insomnia Scale (AIS)
We used the Athen Insomnia Scale (Novak et al., 2004; Soldatos et al., 2000) to measure insomnia. The questionnaire assesses the most common complaints of insomnia with 8 items, such as difficulties in falling asleep, sleep fragmentation, early morning awakenings, daytime complaints related to fatigue, and sleepiness throughout the day. Items are assessed using a 4-point Likert-scale scale. The AIS proved to be an appropriate instrument to identify possible cases of insomnia at 10 points and above (Soldatos et al., 2000). The Hungarian version of the questionnaire is a reliable and valid tool for the assessment of sleep complaints in the adult population (Novak et al., 2004). The scale showed good internal consistency in the present study (Cronbach’s α = 0.793).
General Health Questionnaire (GHQ)
Mental well-being with respect to the last few weeks was measured by the Hungarian version of the 12-item General Health Questionnaire (Balajti et al., 2007; Goldberg, 1992). This short version focuses mostly on symptoms of anxiety and depression and low self-esteem, each measured with a 4-point Likert scale. The scale is widely used in epidemiological surveys assessing mental health problems. The Hungarian adaptation of the scale showed good internal consistency and construct validity in a previous study (Balajti et al., 2007). The internal consistency of the scale in the present study was excellent (Cronbach’s α = 0.895). To investigate our hypothesis, we used the total score without the second item that assesses sleep complaints.
Nightmare and Bad Dream Frequency (BDF, NMF)
In addition, we assessed the frequency of bad dreams (BDF, “How frequently do you have bad (emotionally negative, like unpleasant, distressing or frightening) dreams that do not end in abrupt awakenings?”) and nightmares (NMF, “How frequently do you have emotionally negative dreams that suddenly wake you up?”) on a 9-point scale (never / less than once in a year / once in a year / 2–3 times a year / every 2–3 months / once in a month / 2–3 times a month / once in a week / more than once in a week). Data collections were completed in two periods. In the second period, the questionnaire was utilized as a prescreen evaluation for another study. Therefore, the answer ‘every 2–3 months’ was added to both NMF and BDF scales. Lastly, scores were transformed to a binary form for both variables. The purpose of the binary transformation was to assess the frequency of these dysphoric dreams more reliably through the two extremities, attenuating potential memory biases inherent in retrospective reports. The dichotomous form carries the relevant information whether the individual frequently experienced dysphoric dreams. Participants reporting at least 2–3 bad dreams or nightmares per month received a score of 1, whereas those reporting less frequent dysphoric dreams received a score of 0.
Statistical analysis
All analyses were performed in JASP v.0.14.1 (JASP Team, 2020). We estimated the associations between our variables using the Pearson’s r correlation coefficients.
To examine whether eveningness is associated with poorer mental well-being, regardless of self-reported insomnia complaints (Hypothesis 1), we first applied hierarchical linear regression analysis. The score of the GHQ was considered as the outcome variable, age and gender were included as control variables (Step 1), and insomnia complaints and morningness-eveningness (MEQ-H score as a continuous variable), were added to the model as predictor variables in consecutive steps (Step 2 and 3, respectively).
To investigate our second hypothesis on the presumed associations of frequent nightmares and bad dreams with morningness-eveningness, and to verify whether the potential links are independent of the influence of insomnia complaints and lower mental well-being, logistic regression models were tested, with nightmare frequency and bad dream frequency as the binary outcome variables in two separate models. We entered our predictors in the following order, in both of our models: age and gender were control variables (Step 1), and insomnia complaints, GHQ-score, and morningness-eveningness were entered in separate steps (Step 2–4, respectively).
Results
Descriptive statistics for chronotype, insomnia symptoms, frequency of nightmares, bad dreams, and mental well-being are reported in Table 1. Associations between our variables are shown in Table 2. Eveningness was weakly associated with insomnia complaints, poorer mental well-being, and bad dream frequency, but was not significantly related to nightmare frequency (see Table 2).
Eveningness and insomnia complaints in relation to mental well-being (Hypothesis 1)
A hierarchical linear regression analysis was conducted with mental well-being (GHQ) as the outcome variable and morningness-eveningness (MEQ-H) and self-reported insomnia complaints (AIS) as predictors (the results of each model are summarized in Table 3). After controlling for age and gender (R2 = 0.015, F(2, 2073) = 15.877, p < 0.001), the AIS score was entered into the model (Step 2), which explained a large proportion of the variance (R2 = 0.187, F(3, 2072) = 158.986, p < 0.001), indicating that insomnia symptoms were associated with poorer mental well-being. Morningness-eveningness (Step 3) was also related to lower mental well-being, explaining a small proportion of the variance (R2 = 0.192, F(4, 2071) = 122.653, p < 0.001).
Eveningness and dysphoric dreaming (Hypothesis 2)
The prevalence of frequent nightmares was 21% in the total sample (15% in males; 24% in females), while frequent bad dreams appeared in 26% of the cases (20% in males, 29% in females). Two logistic regression analyses were conducted to test the association between disturbing dream variables and eveningness.
Logistic regression for NMF
First, a logistic regression model was built to predict frequent nightmares from chronotype, insomnia symptoms and mental well-being. After the control variables (age and gender) were set (as Step 1), the added predictor variable (AIS, as Step 2) was found to be a significant contributor to the model (OR = 1.199, 95% CI = 1.158–1.243). GHQ score (as Step 3) was not associated with NMF. MEQ-H was not significantly associated with NMF either (Step 4). The result suggests that eveningness did not contribute to nightmare frequency in our sample. Gender, age, and self-reported insomnia symptoms emerged as significant predictors of NMF in the final model (see Table 4).
Logistic regression for BDF
In a similar vein, chronotype was not a significant predictor of frequent bad dreams. On the other hand, gender, age, insomnia complaints and mental well-being were associated with bad dream frequency in the final model (see Table 4).
Logistic regression for BDF among females
Taking into account the previous findings on gender differences regarding the link between eveningness and nightmare frequency (i.e. the association was only present in females and not in males) (Nielsen, 2010), we split our sample by gender and tested the above models separately for females. The results are shown in the Supplement (Table S1). Morningness-eveningness was not significantly associated with nightmares or bad dreams in females, frequent nightmares and bad dreams were only associated with complaints of insomnia in the final models.
Discussion
The aim of our study was to explore the associations between morningness-eveningness, symptoms of insomnia and frequency of dysphoric dreaming, and complaints of mental well-being. More specifically, we examined if chronotype was associated with lower mental well-being regardless of the influence of subjective insomnia complaints. In addition, we examined if eveningness was related to increased nightmare and bad dream frequency independently of insomnia symptoms and complaints with mental well-being.
Eveningness showed weak correlations with insomnia complaints and mental well-being complaints covering depressive and anxiety symptoms. Regarding dream disturbances, eveningness was weakly associated with bad dream frequency (i.e. unpleasant dreams without abrupt awakenings), but not with frequent nightmares (i.e. unpleasant dreams with abrupt awakenings). Moreover, the association between eveningness and bad dreams was no longer significant if we controlled for the influence of mental well-being and subjective insomnia symptoms in the regression models.
Hierarchical regression models indicated that eveningness was associated with poorer mental well-being, beyond the influence of insomnia complaints; however, it explained a much reduced amount of variance compared to insomnia symptoms. Although we observed a significant association between eveningness and lower mental well-being, the low effect size calls the clinical relevance of this association into question. This result suggests that insomnia complaints constitute a more robust factor associated with mental well-being complaints, compared to eveningness. Although our study is not able to explore the directionality of these links, previous research suggests that the evening preference increases the risk of sleep problems (Chan et al., 2014; Yazdi et al., 2014). Nevertheless, maladaptive sleep habits maintaining disrupted sleep might also facilitate a preference for eveningness (e.g. daytime naps, difficulties of falling asleep at night, morning fatigue, etc.) (Ong et al., 2007; Simor et al., 2015).
The second part of our research aimed to investigate the associations between eveningness with nightmare and bad dream frequency, taking into account the influence of insomnia complaints and mental well-being. Contrary to previous studies, eveningness was not associated with nightmare frequency in our sample. On the other hand, nightmare frequency and bad dream frequency were linked to gender (females showed higher incidence of frequent nightmares), younger age, and insomnia complaints, corroborating the findings of previous questionnaire-based studies (Levin, 1994; Levin & Nielsen, 2007; Schredl & Reinhard, 2011; Spoormaker et al., 2006). Interestingly, lower mental well-being was associated with frequent bad dreams, but not with frequent nightmares.
Our results are consistent with numerous previous findings linking eveningness with insomnia complaints (Chan et al., 2014; Núñez et al., 2019; Ong et al., 2007; Simor et al., 2015; Yazdi et al., 2014), and decreased mental well-being (Hidalgo et al., 2009; Nguyen et al., 2019; Wittmann et al., 2006). Despite the association between eveningness and mental well-being complaints, our analyses indicate that insomnia symptoms constitute a more relevant factor in poorer mental well-being than the preference for eveningness. Difficulties of falling asleep, sleep fragmentation, night time awakenings, and daytime sleepiness seem to be more common complaints among evening-type individuals, compromising daytime functioning. The mismatch between the preferred circadian rhythms as opposed to societal demands might exacerbate maladaptive sleep habits and difficulties in self-regulation (Levandovski et al., 2011).
Previous studies indicating a link between disturbed dreaming (e.g. dream anxiety) slightly differed in sample characteristics, for instance included mainly students (Selvi et al., 2012), or did not exclude participants with medical diagnosis (Nielsen, 2010). Regarding frequent bad dreams and nightmares, the demographic correlates, such as age and gender, are in line with previous findings (Li et al., 2010; Nielsen, 2010). With respect to nightmare frequency, contrary to our hypothesis, eveningness was not associated with frequent nightmares.
Poorer mental well-being emerged as a predictor of frequent bad dreams, corroborating a previous study by Blagrove and colleagues (Blagrove et al., 2004) who showed that lower well-being is not specifically linked to frequent nightmares provoking awakenings, but to the accompanying daytime distress caused by the dysphoric dream experience (Blagrove et al., 2004). We might consider the awakening from a nightmare as a contributor to fragmented sleep, therefore it might be able to worsen the symptoms of insomnia. On the other hand, the item inquiring the experience of bad dreams that do not awaken the dreamer might capture the daytime distress related to the negative dream experience, as bad dreams that do not end in abrupt awakenings may be recalled during the day hours after nocturnal or morning awakenings.
Among the limitations of our study we should mention that males were underrepresented compared to females in our sample, therefore we controlled for the effect of gender in our statistical models. Females are usually over-represented in similar studies (Nielsen, 2010; Sheaves et al., 2016; Rose et al., 2015; Concepcion et al., 2014) and might be more interested in psychological research, hence may be more involved in completing online surveys in psychological fields voluntarily. Secondly, due to the cross-sectional nature of our study we are not able to determine the direction of the associations between the measured variables. Given our study design, we may not exclude the bidirectional associations between our variables of interest. That is, it is also plausible that frequent nightmares and bad dreams lead to insomnia complaints and increased mental health complaints by producing autonomic arousal and a prolonged stress response (Hess et al., 2020). Although insomnia symptoms may also shift individuals to eveningness by increasing daytime fatigue, proneness to daytime naps, eventually later bedtimes (Richardson et al., 2016), and mental health complaints may also facilitate delayed sleep (Hasler et al., 2016; Simor et al., 2018), eveningness can be considered as a relatively stable trait (Druiven et al., 2020). A large body of studies indicate that extreme evening-type individuals are at a higher risk for suffering from insufficient sleep (Chan et al., 2014; Yazdi et al., 2014) and more depressive and/or anxiety symptoms (Hidalgo et al., 2009; Nguyen et al., 2019; Wittmann et al., 2006). Although individuals differ with respect to their proneness to experiencing dysphoric dreams, the frequency of nightmares and bad dreams appear to be linked to state-like fluctuations in emotional load (Carr & Nielsen, 2017; Nielsen, 2010; Schredl & Göritz, 2021; Schredl et al., 2019; Spoormaker et al., 2006). Accordingly, insomnia, mental health complaints, and dysphoric dreams might escalate into a vicious circle, reinforcing each other. Yet, these variables are more likely to be seen as indices linked to certain life-events compared to chronotype. However, our cross-sectional design is not able to capture state-like fluctuations in the measures of interest.
Future studies, applying longitudinal assessments may unravel the directional associations between these variables. However, our cross-sectional design is not able to capture state-like fluctuations in the measures of interest. More specifically, a further study could involve individuals with extreme chronotype and focus on their day-to-day experiences. It might be able to capture the possible bidirectional, temporal associations between mental well-being and dysphoric dreaming while taking the quality of sleep into account. Objective sleep quality assessment could be ensured by mobile EEG headbands, dream diaries, and complemented with subjective daytime sleepiness. Perceived stress during the day, or changes in affect or mood could be measured on a day-to-day basis.
In spite of the limitations of the present study, our results highlight the relevance of insomnia complaints in relation to eveningness and mental health problems, which should be considered in treatment and prevention.
Data availability
The data that support the findings of this study are openly available in OSF at https://osf.io/x83qn/
References
Adan, A. (1994). Chronotype and personality factors in the daily consumption of alcohol and psychostimulants. Addiction, 89(4), 455–462. https://doi.org/10.1111/j.1360-0443.1994.tb00926.x
Adan, A., Archer, S. N., Hidalgo, M. P., Di Milia, L., Natale, V., & Randler, C. (2012). Circadian Typology: A Comprehensive Review. Chronobiology International, 29(9), 1153–1175. https://doi.org/10.3109/07420528.2012.719971
Agargun, M. Y., Kara, H., Özer, Ö. A., Selvi, Y., Kiran, Ü., & Özer, B. (2003). Clinical importance of nightmare disorder in patients with dissociative disorders. Psychiatry and Clinical Neurosciences, 57(6), 575–579. https://doi.org/10.1046/j.1440-1819.2003.01169.x
Archer, S. N., Robilliard, D. L., Skene, D. J., Smits, M., Williams, A., Arendt, J., & von Schantz, M. (2003). A Length Polymorphism in the Circadian Clock Gene Per3 is Linked to DeYoungDelayed Sleep Phase Syndrome and Extreme Diurnal Preference. Sleep, 26(4), 413–415. https://doi.org/10.1093/sleep/26.4.413
Balajti, I., Vokó, Z., Ádány, R., & Kósa, K. (2007). A koherencia-érzés mérésére szolgáló rövidített kérdőív és a lelki egészség (ghq-12) kérdőív magyar nyelvű változatainak validálása= Validation of the Hungarian versions of the abbreviated sense of coherence (SOC) scale and the general health questionnaire (GHQ-12). Mentálhigiéné És Pszichoszomatika, 8(2), 147–161. https://doi.org/10.1556/Mental.8.2007.2.4
Blagrove, M., Farmer, L., & Williams, E. (2004). The relationship of nightmare frequency and nightmare distress to well-being. Journal of Sleep Research, 13(2), 129–136. https://doi.org/10.1111/j.1365-2869.2004.00394.x
Carr, M., & Nielsen, T. (2017). A novel Differential Susceptibility framework for the study of nightmares: Evidence for trait sensory processing sensitivity. Clinical Psychology Review, 58, 86–96. https://doi.org/10.1016/j.cpr.2017.10.002
Chan, J. W. Y., Lam, S. P., Li, S. X., Yu, M. W. M., Chan, N. Y., Zhang, J., & Wing, Y.-K. (2014). Eveningness and Insomnia: Independent Risk Factors of Nonremission in Major Depressive Disorder. Sleep, 37(5), 911–917. https://doi.org/10.5665/sleep.3658
Concepcion, T., Barbosa, C., Vélez, J. C., Pepper, M., Andrade, A., Gelaye, B., Yanez, D., & Williams, M. A. (2014). Daytime sleepiness, poor sleep quality, eveningness chronotype, and common mental disorders among Chilean college students. Journal of American College Health, 62(7), 441–448. https://doi.org/10.1080/07448481.2014.917652
DeYoung, C. G., Hasher, L., Djikic, M., Criger, B., & Peterson, J. B. (2007). Morning people are stable people: Circadian rhythm and the higher-order factors of the Big Five. Personality and Individual Differences, 43(2), 267–276. https://doi.org/10.1016/j.paid.2006.11.030
Druiven, S. J., Hovenkamp-Hermelink, J. H., Knapen, S. E., Kamphuis, J., Haarman, B. C., Penninx, B. W., Antypa, N., Meesters, Y., Schoevers, R., A., & Riese, H. (2020). Stability of chronotype over a 7-year follow-up period and its association with severity of depressive and anxiety symptoms. Depression and Anxiety, 37(5), 466-474.https://doi.org/10.1002/da.22995.
Emens, J., Lewy, A., Kinzie, J. M., Arntz, D., & Rough, J. (2009). Circadian misalignment in major depressive disorder. Psychiatry Research, 168(3), 259–261. https://doi.org/10.1016/j.psychres.2009.04.009
Fabbian, F., Zucchi, B., De Giorgi, A., Tiseo, R., Boari, B., Salmi, R., Cappadona, R., Gianesini, G., Bassi, E., Signani, F., Raparelli, V., Basili, S., & Manfredini, R. (2016). Chronotype, gender and general health. Chronobiology International, 33(7), 863–882. https://doi.org/10.1080/07420528.2016.1176927
Gaspar-Barba, E., Calati, R., Cruz-Fuentes, C. S., Ontiveros-Uribe, M. P., Natale, V., De Ronchi, D., & Serretti, A. (2009). Depressive symptomatology is influenced by chronotypes. Journal of Affective Disorders, 119(1–3), 100–106. https://doi.org/10.1016/j.jad.2009.02.021
Giampietro, M., & Cavallera, G. M. (2007). Morning and evening types and creative thinking. Personality and Individual Differences, 42(3), 453–463. https://doi.org/10.1016/j.paid.2006.06.027
Goldberg, D. (1992). General Health Questionnaire (GHQ-12) NFER-Nelson. Windsor.
Hasler, B. P., Buysse, D. J., & Germain, A. (2016). Shifts toward morningness during behavioral sleep interventions are associated with improvements in depression, positive affect, and sleep quality. Behavioral Sleep Medicine, 14(6), 624–635. https://doi.org/10.1080/15402002.2015.1048452
Hess, G., Schredl, M., Gierens, A., & Domes, G. (2020). Effects of nightmares on the cortisol awakening response: An ambulatory assessment pilot study. Psychoneuroendocrinology, 122, 104900. https://doi.org/10.1016/j.psyneuen.2020.104900
Hidalgo, M. P., Caumo, W., Posser, M., Coccaro, S. B., Camozzato, A. L., & Chaves, M. L. F. (2009). Relationship between depressive mood and chronotype in healthy subjects: Depressive mood and chronotype. Psychiatry and Clinical Neurosciences, 63(3), 283–290. https://doi.org/10.1111/j.1440-1819.2009.01965.x
Horne, J. A., & Östberg, O. (1976). A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology, 4(2), 97–110.
JASP Team (2020). JASP (Version 0.14.1) [Computer Software].
Jeon, H. J., & Lee, S.-J. (2019). Chronobiology and Sleep on Resilience. Chronobiology in Medicine, 1(4), 149–151. https://doi.org/10.33069/cim.2019.0026.
Kivelä, L., Papadopoulos, M. R., & Antypa, N. (2018). Chronotype and Psychiatric Disorders. Current Sleep Medicine Reports, 4(2), 94–103. https://doi.org/10.1007/s40675-018-0113-8
Lancee, J., Spoormaker, V. I., & Van Den Bout, J. (2010). Nightmare frequency is associated with subjective sleep quality but not with psychopathology: Sleep quality and nightmare frequency. Sleep and Biological Rhythms, 8(3), 187–193. https://doi.org/10.1111/j.1479-8425.2010.00447.x
Lázár, A. S., Slak, A., Lo, J.C.-Y., Santhi, N., von Schantz, M., Archer, S. N., Groeger, J. A., & Dijk, D.-J. (2012). Sleep, Diurnal Preference, Health, and Psychological Well-being: A Prospective Single-Allelic-Variation Study. Chronobiology International, 29(2), 131–146. https://doi.org/10.3109/07420528.2011.641193
Levandovski, R., Dantas, G., Fernandes, L. C., Caumo, W., Torres, I., Roenneberg, T., Hidalgo, M. P. L., & Allebrandt, K. V. (2011). Depression Scores Associate With Chronotype and Social Jetlag in a Rural Population. Chronobiology International, 28(9), 771–778. https://doi.org/10.3109/07420528.2011.602445
Levin, R. (1994). Sleep and dreaming characteristics of frequent nightmare subjects in a university population. Dreaming, 4(2), 127. https://doi.org/10.1037/h0094407
Levin, R., & Nielsen, T. A. (2007). Disturbed dreaming, posttraumatic stress disorder, and affect distress: A review and neurocognitive model. Psychological Bulletin, 133(3), 482. https://doi.org/10.1037/0033-2909.133.3.482
Li, S. X., Zhang, B., Li, A. M., & Wing, Y. K. (2010). Prevalence and correlates of frequent nightmares: A community-based 2-phase study. Sleep, 33(6), 774–780. https://doi.org/10.1093/sleep/33.6.774
Melo, M. C. A., Abreu, R. L. C., Linhares Neto, V. B., de Bruin, P. F. C., & de Bruin, V. M. S. (2017). Chronotype and circadian rhythm in bipolar disorder: A systematic review. Sleep Medicine Reviews, 34, 46–58. https://doi.org/10.1016/j.smrv.2016.06.007
Merikanto, I., Kronholm, E., Peltonen, M., Laatikainen, T., Lahti, T., & Partonen, T. (2012). Relation of Chronotype to Sleep Complaints in the General Finnish Population. Chronobiology International, 29(3), 311–317. https://doi.org/10.3109/07420528.2012.655870
Natale, V., & Cicogna, P. (2002). Morningness-eveningness dimension: Is it really a continuum? Personality and Individual Differences, 32(5), 809–816. https://doi.org/10.1016/S0191-8869(01)00085-X
Nguyen, C., Murray, G., Anderson, S., Filipowicz, A., & Ingram, K. K. (2019). In vivo molecular chronotyping, circadian misalignment, and high rates of depression in young adults. Journal of Affective Disorders, 250, 425–431. https://doi.org/10.1016/j.jad.2019.03.050
Nielsen, T. (2010). Nightmares Associated with the Eveningness Chronotype. Journal of Biological Rhythms, 25(1), 53–62. https://doi.org/10.1177/0748730409351677
Novak, M., Mucsi, I., Shapiro, C. M., Rethelyi, J., & Kopp, M. S. (2004). Increased utilization of health services by insomniacs—an epidemiological perspective. Journal of Psychosomatic Research, 56(5), 527–536. https://doi.org/10.1016/j.jpsychores.2004.02.007
Núñez, P., Perillan, C., Arguelles, J., & Diaz, E. (2019). Comparison of sleep and chronotype between senior and undergraduate university students. Chronobiology International, 36(12), 1626–1637. https://doi.org/10.1080/07420528.2019.1660359
Ong, J. C., Huang, J. S., Kuo, T. F., & Manber, R. (2007). Characteristics of Insomniacs with Self-Reported Morning and Evening Chronotypes. Journal of Clinical Sleep Medicine, 03(03), 289–294. https://doi.org/10.5664/jcsm.26801
Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: An ambulatory polysomnographic study. Borderline Personality Disorder and Emotion Dysregulation, 2(1), 1–9. https://doi.org/10.1186/s40479-014-0023-4
Prat, G., & Adan, A. (2011). Influence of Circadian Typology on Drug Consumption, Hazardous Alcohol use, and Hangover Symptoms. Chronobiology International, 28(3), 248–257. https://doi.org/10.3109/07420528.2011.553018
Randler, C., Schredl, M., & Göritz, A. S. (2017). Chronotype, Sleep Behavior, and the Big Five Personality Factors. SAGE Open, 7(3), 215824401772832. https://doi.org/10.1177/2158244017728321
Richardson, C. E., Gradisar, M., & Barbero, S. C. (2016). Are cognitive “insomnia” processes involved in the development and maintenance of delayed sleep wake phase disorder? Sleep Medicine Reviews, 26, 1–8. https://doi.org/10.1016/j.smrv.2015.05.001
Roenneberg, T., & Merrow, M. (2007). Entrainment of the Human Circadian Clock. Cold Spring Harbor Symposia on Quantitative Biology, 72(1), 293–299. https://doi.org/10.1101/sqb.2007.72.043
Roenneberg, T., Wirz-Justice, A., & Merrow, M. (2003). Life between Clocks: Daily Temporal Patterns of Human Chronotypes. Journal of Biological Rhythms, 18(1), 80–90. https://doi.org/10.1177/0748730402239679
Rose, D., Gelaye, B., Sanchez, S., Castañeda, B., Sanchez, E., Yanez, N. D., & Williams, M. A. (2015). Morningness/eveningness chronotype, poor sleep quality, and daytime sleepiness in relation to common mental disorders among Peruvian college students. Psychology, Health & Medicine, 20(3), 345–352. https://doi.org/10.1080/13548506.2014.951367
Sandman, N., Merikanto, I., Määttänen, H., Valli, K., Kronholm, E., Laatikainen, T., Partonen, T., & Paunio, T. (2016). Winter is coming: Nightmares and sleep problems during seasonal affective disorder. Journal of Sleep Research, 25(5), 612–619. https://doi.org/10.1111/jsr.12416
Schredl, M., Gilles, M., Wolf, I., Peus, V., Scharnholz, B., Sütterlin, M., Bardtke, S., Send, T., S., Samaras, A., & Deuschle, M. (2019). Nightmares and stress: a longitudinal study. Journal of Clinical Sleep Medicine, 15(9), 1209-1215.https://doi.org/10.5664/jcsm.7904.
Schredl, M., & Göritz, A. S. (2021). Stability of nightmare frequency and its relation to neuroticism: A longitudinal study. Journal of Sleep Research, 30(3), e13126. https://doi.org/10.1111/jsr.13126
Schredl, M., & Reinhard, I. (2011). Gender differences in nightmare frequency: A meta-analysis. Sleep Medicine Reviews, 15(2), 115–121. https://doi.org/10.1016/j.smrv.2010.06.002
Selvi, Y., Aydin, A., Gulec, M., Boysan, M., Besiroglu, L., Ozdemir, P. G., & Kilic, S. (2012). Comparison of dream anxiety and subjective sleep quality between chronotypes: Dream anxiety in chronotypes. Sleep and Biological Rhythms, 10(1), 14–22. https://doi.org/10.1111/j.1479-8425.2011.00511.x
Sheaves, B., Porcheret, K., Tsanas, A., Espie, C. A., Foster, R. G., Freeman, D., Harrison, P. J., Wulff, K., & Goodwin, G. M. (2016). Insomnia, Nightmares, and Chronotype as Markers of Risk for Severe Mental Illness: Results from a Student Population. Sleep, 39(1), 173–181. https://doi.org/10.5665/sleep.5342
Simor, P., Harsányi, A., Csigó, K., Miklós, G., Lázár, A. S., & Demeter, G. (2018). Eveningness is associated with poor sleep quality and negative affect in obsessive–compulsive disorder. Journal of Behavioral Addictions, 7(1), 10–20. https://doi.org/10.1556/2006.7.2018.07
Simor, P., & Polner, B. (2017). Differential influence of asynchrony in early and late chronotypes on convergent thinking. Chronobiology International, 34(1), 118–128. https://doi.org/10.1080/07420528.2016.1246454
Simor, P., Zavecz, Z., Pálosi, V., Török, C., & Köteles, F. (2015). The influence of sleep complaints on the association between chronotype and negative emotionality in young adults. Chronobiology International, 32(1), 1–10. https://doi.org/10.3109/07420528.2014.935786
Sjöström, N., Hetta, J., & Waern, M. (2009). Persistent nightmares are associated with repeat suicide attempt: A prospective study. Psychiatry Research, 170(2–3), 208–211. https://doi.org/10.1016/j.psychres.2008.09.006
Soldatos, C. R., Dikeos, D. G., & Paparrigopoulos, T. J. (2000). Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. Journal of Psychosomatic Research, 48(6), 555–560. https://doi.org/10.1016/S0022-3999(00)00095-7
Spoormaker, V. I., Schredl, M., & van den Bout, J. (2006). Nightmares: From anxiety symptom to sleep disorder. Sleep Medicine Reviews, 10(1), 19–31. https://doi.org/10.1016/j.smrv.2005.06.001
Takeuchi, H., Yamazaki, Y., Oki, K., Wada, K., Noji, T., Kawada, T., Nakade, M., Krejci, M., & Harada, T. (2015). Effects of chronotype and environmental factors upon sleep and mental health in Japanese students aged 18–40 yrs. Biological Rhythm Research, 46(6), 771–784. https://doi.org/10.1080/09291016.2015.1048952
Tanskanen, A., Tuomilehto, J., Viinamäki, H., Vartiainen, E., Lehtonen, J., & Puska, P. (2001). Nightmares as predictors of suicide. Sleep, 24(7), 845–848. https://doi.org/10.1093/sleep/24.7.845
Tavernier, R., & Willoughby, T. (2014). Are all evening-types doomed? Latent class analyses of perceived morningness–eveningness, sleep and psychosocial functioning among emerging adults. Chronobiology International, 31(2), 232–242. https://doi.org/10.3109/07420528.2013.843541
Taylor, B. J., & Hasler, B. P. (2018). Chronotype and Mental Health: Recent Advances. Current Psychiatry Reports, 20(8), 59. https://doi.org/10.1007/s11920-018-0925-8
Tonetti, L., Fabbri, M., & Natale, V. (2009). Relationship between Circadian Typology and Big Five Personality Domains. Chronobiology International, 26(2), 337–347. https://doi.org/10.1080/07420520902750995
Wilson, G. D. (1990). Personality, time of day and arousal. Personality and Individual Differences, 11(2), 153–168. https://doi.org/10.1016/0191-8869(90)90008-F
Wittmann, M., Dinich, J., Merrow, M., & Roenneberg, T. (2006). Social Jetlag: Misalignment of Biological and Social Time. Chronobiology International, 23(1–2), 497–509. https://doi.org/10.1080/07420520500545979
Yazdi, Z., Sadeghniiat-Haghighi, K., Javadi, A. R. H. S., & Rikhtegar, G. (2014). Sleep quality and insomnia in nurses with different circadian chronotypes: Morningness and eveningness orientation. Work, 47(4), 561–567. https://doi.org/10.3233/WOR-131664
Zadra, A. & Donderi D. C. (2000). Nightmares and bad dreams: Their prevalence and relation to psychological well-being. Journal of Abnormal Psychology, 109, 210–219. https://doi.org/10.1037/0021-843X.109.2.273
Zavecz, Z., Török, C., Köteles, F., Pálosi, V., & Simor, P. (2015). The psychometric properties of the Hungarian version of the Morningness-Eveningness Questionnaire (MEQ-H): The separate factors of morning freshness and circadian rhythmicity. Psychiatria Hungarica: A Magyar Pszichiátriai Társaság Tudományos Folyóirata, 30(3), 318–331.
Acknowledgements
The project was supported by the Hungarian Scientific Research Fund (NKFI FK 128100) of the National Research, Development and Innovation Office. The study was supported by ELTE Thematic Excellence Programme 2020 TKP2020-IKA-05 provided by National Research, Development and Innovation Office.
Funding
Open access funding provided by Eötvös Loránd University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics declarations
The study has been approved by the United Ethical Review Board for Psychological Experiments (EBKEP, Hungary); all participants gave informed consent before completing the questionnaire. The study was conducted in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Benkő, Z., Köteles, F. & Simor, P. Insomnia symptoms do, but chronotype does not show relevant associations with mental well-being and negative dream experiences. Curr Psychol 42, 7826–7835 (2023). https://doi.org/10.1007/s12144-022-03901-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03901-6