Abstract
The COVID-19 pandemic has undoubtedly negatively affected individuals’ quality of life through multiple means such as social isolation, exacerbated mental health conditions, and financial instability. Multiple studies have demonstrated that one of the negative correlates of quality of life is the perceived danger of COVID-19 (i.e., fear of and anxiety about COVID-19). The current study addresses limitations in the literature by testing how life changes from COVID-19 explain the direct effect of the perceived danger of COVID-19 on quality of life using a United States sample between those who have had COVID-19 compared to those who have not had COVID-19. Undergraduate students (n = 196) from a Midwestern University in the United States participated in this study for course credit (White: n = 109; 55.61%; Male: n = 94; 48.0%). Participants completed this study online and at home where they responded to a demographic form and several measures of the effects of COVID-19 and quality of life. The results suggest that COVID-19 life changes fully explain the negative relationship between the perceived danger of COVID-19 and quality of life, but only in those who have had COVID-19. In the group that has never had COVID-19, the only significant relationship was the positive relationship between the perceived danger of COVID-19 on COVID-19 life changes. The results suggest that researchers may consider steering research away from the perceived danger of COVID-19 and onto remedying life changes from COVID-19 to improve individuals’ quality of life. I further discuss the theoretical findings, implications, limitations, and future directions.
Similar content being viewed by others
The COVID-19 pandemic has undoubtedly had a negative effect on individuals’ quality of life through multiple means, such as fear in the chronically ill, isolation in those with mental health concerns, challenges to maintaining a healthy lifestyle, and those directly harmed by contracting the coronaviruses (Gamberini et al., 2021; Huang et al., 2022; Koc et al., 2022; Rogers et al., 2021; Shoychet et al., 2022). Recent research demonstrates that the COVID-19 pandemic has negatively affected every domain that contributes to one’s quality of life as defined by the World Health Organization (World Health Organization, 1996) including social activities, long-term health problems, environmental factors, and diminished psychological well-being through mental health concerns (Alkire et al., 2021; Amdal et al., 2021; Brülhart et al., 2021; Fried et al., 2022; Saikia et al., 2021; Stamatis et al., 2022; Stone, 2022). Some researchers suggest that the coronaviruses that cause COVID-19 will likely not be eradicated soon (Case et al., 2021; Ioannidis, 2022), which suggests that learning about how to improve individuals’ quality of life, despite the presence of COVID-19, may be an effective means of mitigating some of the negative effects of the COVID-19 pandemic (Huang et al., 2021; Lucas et al., 2021; Rocco et al., 2021). Thus, research that clarifies how the COVID-19 pandemic negatively affects individuals' quality of life may contribute to the development of tools, interventions, and protocols that professionals can use to enhance people's quality of life.
One of the determinants that emerged as a negative correlate of quality of life is the fear of and anxiety about the COVID-19 pandemic, which is labeled as the perceived danger of COVID-19. Five studies to date have demonstrated this negative relationship between the perceived danger of COVID-19 and quality of life, all of which were cross-sectional (Demirbas et al., 2021; Gönenç et al., 2022; Hayes et al., 2021; Naghizadeh et al., 2021; Shoychet et al., 2022). Three of these studies focused on health-related populations (i.e., irritable bowel disease, pregnancy, and sexual health), and the effects were found in Canada, Turkey, Iran, and Australia, but researchers have yet to demonstrate these effects in the United States. Note also that none of these studies report the percentage of their sample who have had COVID-19 or if their effects differ between those who have had and not had COVID-19. It is reasonable to expect that one’s perception of the danger of COVID-19 and one’s quality of life may be affected by directly experiencing the disease, however, this group difference remains untested in the literature. Further, although one of these studies demonstrated that intolerance of uncertainty and health locus of control moderate this relationship (Shoychet et al., 2022), no studies to date have provided empirical evidence for potential explanations for why this relationship exists.
A potential explanation for why a negative relationship exists between the perceived danger of COVID-19 and quality of life may be due to the life changes caused by adjusting to the COVID-19 pandemic. Specifically, although it appears as if the perceived danger of COVID-19 is directly negatively related to an individual’s quality of life, dozens of studies have demonstrated that the perceived danger of COVID-19 is related to multiple life changes caused by the pandemic, and other studies have demonstrated that these life changes are directly related to an individual’s quality of life. For example, several studies have demonstrated that the fear of COVID-19 is negatively related to poor mental health (Belen, 2022; Duong, 2021; Kayis et al., 2021; Khattak et al., 2020; Khudaykulov et al., 2022; Mauer et al., 2022; Peker & Cengiz, 2021; Suhail et al., 2022; Vilca et al., 2022; Yenen & Çarkit, 2021), difficulties living with physical health concerns (Ahmed et al., 2021; Buran & Gerçek Öter, 2021a, 2021b; Duong, 2021), and vocational difficulties (De los Santos & Labrague, 2021; Khattak et al., 2020; Khudaykulov et al., 2022; Saracoglu et al., 2020). Further, numerous studies have found that life disruptions from COVID-19 affect domains that are involved in one’s quality of life (e.g., mental health or physical health) or quality of life measured directly (Bhogal et al., 2021; Buran & Gerçek Öter, 2021a, 2021b; Egede et al., 2022; Handberg et al., 2021; Koenig et al., 2021; Kurzhals et al., 2021; Saracoglu et al., 2020; Sugawara et al., 2021; Trucco et al., 2022). Thus, despite the numerous studies that support the indirect effect of the perceived danger of COVID-19 on quality of life through the intervening variable of COVID-19 life changes, no study to date has modeled this effect.
Evidence for the importance of stressful life changes explaining the relationship between emotion and mental health outcomes may come from the diathesis-stress model (Zuckerman, 1999). This model is a biosocial model supported by human and animal research that suggests that the development of mental illness comes from two potential and general factors which are 1) a biological or genetic factor (diathesis) and 2) stressful life situations. This model emphasizes that normal emotional experiences in individuals who are predisposed to mental illnesses may become dysfunctional when in the presence of stressful situations. In the case of COVID-19, normal fear and anxiety around COVID-19 may be exacerbated by the stressful life changes caused by COVID-19, leading to a reduction in quality of life. Specifically, this model suggests that the fear and anxiety of COVID-19 itself may not become problematic until the individual experiences the stressful situations caused by COVID-19. Thus, the relationship between fear and anxiety over COVID-19 may only exist because of the stressful life changes from COVID-19. The current study aims to find empirical evidence of the necessity of COVID-19 life changes and argue that without the stressful situations caused by COVID-19 life changes that the relationship between the perceived danger of COVID-19 and quality of life may not be significant. This study would be the first to apply the diathesis-stress model to the COVID-19 pandemic and quality of life.
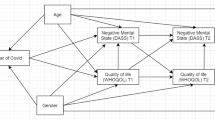
To model these effects, I tested a full structural equation model involving three latent factors which are, 1) the perceived danger of COVID-19, 2) COVID-19 life changes, and 3) quality of life. The perceived danger of COVID-19 factor is comprised of two scales (i.e., fear of COVID-19 and anxiety from COVID-19). The COVID-19 life changes factor is comprised of eight scales designed to measure various domains of living disrupted by the COVID-19 pandemic (i.e., finances, loved ones, job, safety, school, mental health, physical health, and social connections). The quality of life factor is comprised of the four subscales of quality of life as defined by the World Health Organization (i.e., physical health, psychological health, environment, and relationships). I specified three direct relationships, which are 1) the perceived danger of COVID-19 onto COVID-19 life changes, 2) COVID-19 life changes onto quality of life, and 3) the perceived danger of COVID-19 onto quality of life (see Fig. 1). To test the explanatory power of COVID-19 life changes I specified an indirect effect of the perceived danger of COVID-19 on quality of life through the intervening variable of COVID-19 life changes. Finally, I tested if these effects persist in those who have had COVID-19 compared to those who have not had COVID-19, as these group differences remain untested in the literature.
The current study aims to address and progress several limitations and absent findings in the literature. First, I will replicate the positive relationship between the perceived danger of COVID-19 and quality of life in a United States sample. This relationship may even be stronger than in other countries because the United States has one of the highest prevalence rates of COVID-19 (World Health Organization, 2022). Second, this is the first study that tested the indirect effect and full explanatory power of the perceived danger of COVID-19 on quality of life through the intervening variable of COVID-19 life changes. Although the literature supports all these relationships independently using bivariate correlations, this is the first study to test them all simultaneously. Third, this is the only study to date that compares these relationships between those who have had COVID-19 and those who have not had COVID-19. Finally, this is the only study to date that employs structural equation modeling (SEM), which has several benefits over bivariate correlations including 1) simultaneous multivariate testing of relationships, 2) the ability to control for the effects of each independent relationship, and 3) the use of latent variable scores over observed scores (Kline, 2016). I examine these important relationships and tested for between-group differences to guide future research on improving individuals’ quality of life, despite living during the COVID-19 pandemic.
Method
Participants
Participants were undergraduate students (n = 224) from a Midwestern University in the United States who participated in the study for course credit. Individuals who failed either of the two attention checks were removed (e.g., please select moderately true; n = 28; 12.50%), which resulted in a final sample of 196 participants. The complete demographic information and the demographic information for those who have had and not had COVID-19 separately are presented in Table 1. Note that there were no significant differences in demographics or sample size between the group who acquired COVID-19 and those who did not. Thus, I can attribute any differences in the structural equation models to the differences in contracting COVID-19, not demographic variation. All the data, scripts, and materials for the current study are on an Open Science Framework page, which can be accessed at the following link: https://osf.io/3yqtv/?view_only=f3800dc28cf74f739b46ac8c0296ad9a
Procedure
I guided participants to complete the study via the SONA Systems website (SONA Systems, Ltd., Tallinn, Estonia) during the Spring of 2022. Participants completed an informed consent document, a demographic survey, a survey consisting of several measures of the effects of COVID-19, a measure of their quality of life, and then a debriefing form. I awarded the participants course credit for their participation. The entire study took no longer than 30 min.
Measures
For internal consistencies, descriptive statistics, and mean differences between groups see Table 2. Note that there were no significant differences in the means between the group who acquired COVID-19 and those who did not. Thus, any differences in the structural equation models can be attributed to the differences in the relationships among the variables, not mean differences across groups.
Fear of COVID-19 scale
The Fear of COVID-19 scale is a 7-item unidimensional measure of individuals’ general fear about COVID-19 (Ahorsu et al., 2020). The participants rated items on a 5-point Likert-type scale from 1 = strongly disagree to 5 = strongly agree. The scale has a strong unidimensional factor structure, convergent validity, and internal consistency.
COVID anxiety scale
The COVID-19 Anxiety Scale is a unidimensional measure of anxiety about the COVID-19 pandemic (Lee, 2020). Individuals rate five items on a 5-point scale from 1 = not at all to 5 = nearly every day for the last two weeks. The scale has a robust unidimensional structure in both a principal components analysis and confirmatory factor analysis and has demonstrated measurement invariance across age and gender. Further, the scale demonstrated strong construct validity with measures of psychopathology and had a strong internal consistency.
WHOQOL-BREF
The World Health Organization Quality of Life – Bref is an abbreviated version of the World Health Organization Quality of Life-100 scale designed to measure various dimensions of an individual’s quality of life (World Health Organization, 1996). The participants rated 26 items on different 5-point Likert-type scales. The scale contains two global single-item subscales of global quality of life and global health quality of life, which I did not use in the current study. Instead, I used the four remaining subscales as indicators of a quality of life factor, which contains a 1) physical quality of life, 2) psychological quality of life, 3) environmental quality of life, and 4) relationships quality of life. Although the internal consistency in the current study is low, the scale has demonstrated strong psychometric properties and has been translated into multiple languages.
Coronavirus Impact Domains Scale (CIDS)
The Coronavirus Impact Domains Scale (CIDS) is a multidimensional measure of the effects the COVID-19 pandemic has had on individuals’ lives (Stone, 2022). The scale measures nine domains, containing 6-items each, which are 1) Finances, 2) Loved Ones, 3) Job, 4) Safety, 5) School, 6) Mental Health, 7) Physical Health, and 8) Social Activities. The Quality of Life subscale was removed to reduce redundancy between the independent and dependent variables. The participants rate how much an item applies to them on a 5-point scale from 1 = not at all to 5 = very much. The scale demonstrated excellent internal consistency, structural validity, and construct validity in the original study.
Planned analyses
I conducted the analyses for the current paper using IBM SPSS Statistics (IBM Corp. Released 2021. IBM SPSS Statistics for Mac, Version 28.0. Armonk, NY: IBM Corp) and R 3.6.0 (R Core Team 2020, R Foundation for Statistical Computing, Vienna, Austria). I used Kline’s (2016) three-step process of assessing model fit, which involves first fitting the model to the data and reporting the exact fit test. In step two, I examine correlational residuals larger than an absolute value of 0.10 to assess for local areas of misfit. Finally, in step three, I report the RMSEA, CFI, and SRMR. I used the lavaan package 0.6–5 (Rosseel, 2012) and the Diagonally Weighted Least Squares estimator for parameter estimates to account for ordinal indicators.
Results
Preliminary analyses
The data were first checked for outliers, skewness, and kurtosis of the scale and subscale scores. Several variables contained outliers as defined as two standard deviations above or below the mean, including the COVID-19 Anxiety Scale (23), physical quality of life (1), environmental quality of life (3), relationship quality of life (6), and Fear of COVID-19 Scale (1). However, all outliers were valid cases, so they were not eliminated from the analyses (Orr et al., 1991). An analysis of skewness and kurtosis revealed no non-normal distributions, which is defined as an absolute value of skewness of greater than two or an absolute value of kurtosis of greater than seven (West et al., 1995), except for the COVID-19 Anxiety Scale with a skewness of 3.73 and kurtosis of 15.19. I did not transform the COVID-19 Anxiety Scale because it was the only nonnormally distributed variable; thus, artifactual factors are not an issue. Skewness for the other variables ranged from -0.44 to 1.35, and kurtosis ranged from -1.09 to 0.94. To conserve power and stabilize the parameter estimates, I used the scale and subscale scores as indicators instead of the individual items. There were no missing data.
Measurement models
The first step to demonstrating a full indirect effect is demonstrating that a direct relationship exists without the specified indirect effect. I demonstrated this relationship by using a two-step process. The first step involved fitting a measurement model involving all the factors covaried. Then, the direct effects are specified, and assess the fit of the structural model. The measurement and structural models in the current study are equivalent, which means they fit the data equally well and share the same indicator loadings, error variances, and correlational residuals (Kline, 2016). Regarding the sample of those who have had COVID-19, the measurement model passed the exact fit test, χ2(74) = 61.58, p = 0.848. After examining the correlational residuals, there were 13 residuals that were larger than an absolute value of 0.10. These residuals were randomly distributed (see Table 3), RMSEA = 0.000, 90% CI[0.000, 0.033], p = 0.991, SRMR = 0.077; CFI = 1.00 (see Model A in Fig. 2). The measurement model in those who have not had COVID-19 followed a similar pattern, where it passed the exact fit test, χ2(74) = 37.71, p > 0.999, with 11 correlational residuals larger than an absolute value of 0.10 distributed in a random pattern, (see Table 3), RMSEA = 0.000, 90% CI[0.000, 0.000], p > 0.999, SRMR = 0.076; CFI = 1.00 (see Model C in Fig. 2). Although I could make modifications to these models by adding error covariances between the areas of misfit suggested by the correlational residuals, given the outstanding fit and lack of strong theoretical justifications, it was not necessary to make modifications due to diminishing returns in model fit. Thus, each measurement model was retained as a plausible explanation of the data.
Measurement and Structural Models Between Those Who Have Had COVID-19 and Those Who Have Not Had COVID-19. Note. A = Measurement model in the COVID-19 positive sample. B = Structural model in the COVID-19 positive sample. C = Measurement model in the COVID-19 negative sample. D = Structural model in the COVID-19 negative sample, *p < .05
The relationship between the perceived danger of COVID-19 and quality of life was significant and negative in both samples. In those who have had COVID-19, the unstandardized estimate for the covariance was -0.13, SE = 0.02, p < 0.001, and in those who have never had COVID-19 the unstandardized estimate for the covariance was -0.10, SE = 0.3, p < 0.001. Thus, when I fit the structural models, they must meet two criteria to determine if COVID-19 life changes fully explain the relationship between the perceived danger of COVID-19 and quality of life. The first criterion is a significant indirect effect of the perceived danger of COVID-19 on quality of life through the intervening variable of COVID-19 life changes. Second, the relationship between the perceived danger of COVID-19 and quality of life should become nonsignificant (i.e., and thus fully explained by the indirect effect).
Structural models
I fit the structural model by specifying the direct and indirect relationships in those who have had COVID-19 (see Model B in Fig. 2). The analysis met the criteria for a full explanation, with the indirect effect being significant with an unstandardized estimate of -0.18, SE = 0.06, p = 0.003, and the direct effect from the perceived danger of COVID-19 on quality of life becoming nonsignificant with an unstandardized estimate of -0.07, SE = 0.06, p = 0.236 (see Fig. 3). The model explained 40.6% of the variability in quality of life. A different pattern emerged for those who have not had COVID-19, with the indirect effect being nonsignificant with an unstandardized estimate of -0.44, SE = 0.44, p = 0.317 (see Model D in Fig. 2). The only significant direct effect in the structural model for those who have never had COVID-19 was between the perceived danger of COVID-19 and COVID-19 life changes, with an unstandardized estimate of 1.08, SE = 0.51, p = 0.034. Thus, COVID-19 life changes can fully explain the relationship between the perceived danger of COVID-19 and quality of life, but only in those who have had COVID-19.
Post-hoc exploratory control for COVID-19 severity
Although the current study classified those who have had COVID-19 and those who have not had COVID-19 into two groups, it is possible that there are different effects within the group that had COVID-19 as a function of the severity of their COVID-19 symptoms. To control for this range of severity, participants reported how severe their COVID-19 symptoms were on a scale from 1 = asymptomatic to 5 = hospitalization. 20 people reported being asymptomatic (19.05%), 44 mild (41.90%), 30 moderate (28.57%), 8 severe (7.62%), and 2 were hospitalized (1.90%). Thus, 70.48% of the sample reported mild to moderate COVID-19 symptoms, suggesting that the group who reported having COVID-19 was largely symptomatic and homogeneous. Further, an independent samples t-test revealed that the difference in COVID-19 symptoms between those who have had COVID-19 and those who have not was significant and very large, p < 0.001, Cohen’s d = 3.07, suggesting that these groups are starkly different in their experiences of COVID-19.
I specified the severity of COVID-19 to control for quality of life in the measurement model in those who had COVID-19 to examine if the effects found in the study remain, despite the severity of COVID-19. In this measurement model, all three relationships between the factors were significant, ps < 0.001. In the structural model, the relationship between fear of COVID-19 and quality of life was non-significant, p = 0.260, and the indirect effect of fear of COVID-19 on quality of life through the intervening variable of COVID-19 life changes was significant and negative, with an unstandardized parameter estimate of -0.18, SE = 0.6, p = 0.003. Further, the direct effect from severity to quality of life was significant, p < 0.001. Thus, controlling for COVID-19 severity did not change the results. However, when controlling for COVID-19 severity, the R2 increased from 40.6% to 50.1%. This increase is a medium effect, Cohen’s f2 = 0.19. Although controlling for severity does not change the model, it does explain 9.5% more variability in the quality of life factor.
Discussion
The current study attempted to explain the negative relationship between the perceived danger of COVID-19 and quality of life through COVID-19 life changes and to test if this effect occurs differently between those who have had COVID-19 and those who have not. The results suggest that COVID-19 life changes fully explain the replicated effect in the literature of the negative relationship between COVID-19 perceived danger and quality of life, even when controlling for severity of symptoms. Further, I only found this full indirect effect in those who have had COVID-19. In the group that has never had COVID-19, the only significant relationship was the positive relationship between the perceived danger of COVID-19 on COVID-19 life changes. In the following disucssion, I discuss the findings, theoretical implications, practical implications, the limitations of the study, and future directions researchers may consider.
The results suggest that the reason that individuals who have had COVID-19 experience a lower quality of life when their perceived danger of COVID-19 is higher is strictly because of the changes in their lives from the COVID-19 pandemic. Therefore, the perceived danger of COVID-19 may not be the direct risk factor for the worsened quality of life as some of the literature suggests (e.g., Demirbas et al., 2021; Gönenç et al., 2022; Hayes et al., 2021; Naghizadeh et al., 2021; Shoychet et al., 2022). Instead, it is the life changes COVID-19 has forced on people that lower one's quality of life. For example, it appears as if someone experiences fear or anxiety over COVID-19, so they also make or experience life changes to protect themselves (e.g., individuals fear catching COVID-19, so they stop spending time with friends or family, resulting in limited socialization), and then it is these life changes that coincide with the worsened quality of life (e.g., less socialization coincides with mental illness and isolation, resulting in lower quality of life). Thus, although it appears as if the perceived danger of COVID-19 directly negatively relates to quality of life, this study suggests that life changes fully explain this relationship, but only in those who have had COVID-19.
Theoretical implications
The results from this study support the importance of the diathesis-stress model, but only in those who have directly experienced COVID-19. Specifically, the relationship between the experiences of fear and anxiety from COVID-19 may only be related to the quality of life because of the indirect effect of the stressful life situations caused by COVID-19. Thus, this study is the first study to apply the diathesis-stress model to the COVID-19 pandemic, emphasizing that stressful life changes, especially those that happen across domains as measured in the current study, may be a variable that explains why some people who experience a great deal of perceived danger of COVID-19 simultaneously reported worse quality of life compared to those who experience less perceived danger of COVID-19. Thus, this study provides empirical evidence that researchers and clinicians may consider the stressful life changes caused by COVID-19 to potentially be a precipitating factor in their case conceptualizations.
The current study further suggests that future research may consider the importance of the various ways a pandemic affects the areas of individuals' life, creating stress and thus vulnerability to psychopathology. The current study and the CIDS validation study (Stone, 2022) suggest that a pandemic can create stressful life circumstances across multiple domains, thus increasing the vulnerability of individuals predisposed to developing psychopathology. As such, some literature may generalize that it is catching the disease during a pandemic that causes the stress, and the current study provides some evidence of that generalization by only finding the indirect effect in those who have had COVID-19. Still, researchers and clinicians must not understate the indirect effects (e.g., reduced social contact or financial insecurity) of living in a pandemic on mental health outcomes. In this sense, living during a pandemic may pose a unique and robust vulnerability to those predisposed to psychopathology because of its effects on potentially all domains of one’s life.
Study outcome & practical implications
This indirect effect has two notable practical implications. First, interventions targeting the perceived danger of COVID-19 with the hope of improving individuals' quality of life may not be as potent as remedying the effects of COVID-19 on individuals' lives directly. Interventions aimed at reducing fear and anxiety around COVID-19 may be relevant to those with mental health concerns (Bendau et al., 2021), but generally may not be as effective for improving the general public’s quality of life. Second, for those who have had COVID-19 and are experiencing difficulties with their quality of life, intervention strategies remedying the life changes from COVID-19 may result in improved quality of life. However, the evidence present in the current study is just correlative, so this implication is speculative. Unfortunately, these intervention strategies to reduce and eradicate the coronaviruses that cause COVID-19, such as masking, vaccines, lockdowns, and medicines, have been met with hesitancy and contention in the United States (Finney-Rutten et al., 2021; Nadanovsky & Dos Santos, 2020). Generally, the results of this study suggest that researchers may want to shift away from the perceived danger of COVID-19 and onto the life changes of COVID-19 in those who have had the disease.
The current study also found that the indirect effect of the perceived danger of COVID-19 on quality of life through the intervening variable of COVID-19 life changes varies as a function of having COVID-19. In the sample that reported never having COVID-19, the only significant relationship was a positive relationship between the perceived danger of COVID-19 and COVID-19 life changes. Interestingly, this effect emerged despite no significant group differences in sample size, demographics, means, and standard deviations of each subscale. Thus, the only remaining explanation is that for people who have never had COVID-19, the perceived danger of COVID-19 and quality of life are not related when specifying the hypothesized direct effects. In addition to having no significant group differences in sample size, demographics, means, or standard deviations of each subscale, this study is the first in the literature to find a group difference in these effects, making it challenging to speculate as to why these group differences occurred.
Although interpreting the structural model in the group that has never contracted COVID-19 is possible, it is merely speculative because there is no literature or between-group differences to support the conclusions. However, the data suggest that in those who have never had COVID-19, their perceived danger of COVID-19 positively coincides with the life changes from COVID-19 (e.g., someone who experiences a great deal of perceived COVID-19 danger may result in less time in socializing with others). However, the difference between groups occurs when those who have never had COVID-19 report no effects on their quality of life. Thus, in those people who have not experienced COVID-19, their life changes from COVID-19 appear to have no relationship to their quality of life when controlling for their perceived danger of COVID-19. This finding is a particularly novel finding since many studies that include mixed samples of those who have had and not had COVID-19 have found that the impact of COVID-19 on individuals' lives affects their quality of life (e.g., Bhogal et al., 2021; Kurzhals et al., 2021; Saracoglu et al., 2020), however, this study suggests that these effects are primarily driven by those who have had COVID-19.
There are some important practical implications of these findings. First, for people who have not had COVID-19, interventions focusing on alleviating fear and anxiety about COVID-19 or the life changes from COVID-19 that attempt to improve individuals' quality of life may not be as helpful as previously thought (e.g., Demirbas et al., 2021; Gönenç et al., 2022; Kurzhals et al., 2021; Saracoglu et al., 2020). Second, the significant covariances between 1) perceived danger of COVID-19 and quality of life and 2) COVID-19 life change found in the measurement model may be illusory because they disappear once each relationship is controlled for the other. Thus, in other studies involving those who have not had COVID-19, these relationships may be overstated if they are conducted in isolation of each other. Finally, the question remains of if individuals who have never had COVID-19 report similar amounts of perceived danger, life changes, and quality of life to those who have had COVID-19, yet neither perceived danger nor life changes are related to their quality of life, then what explains the variability in quality in life in those who have never had COVID-19? This question remains an area for future research.
Limitations & future directions
This study has several important limitations for which researchers can build upon in future studies. First, the most significant limitation of these data is that they are cross-sectional. Cross-sectional data collection limits our ability to predict outcomes and demonstrate a mediation effect. The data do not clarify the temporal precedence of these relationships; thus, the results may only be interpreted as a ‘snapshot’ of these relationships across individuals. Future researchers may consider detecting the effects found in this study using a longitudinal method. Second, there are some generalizability constraints from this sample, which is mostly White, cis-gender undergraduates. Future researchers may want to replicate these effects in a more representative sample or in a community setting to demonstrate the generalizability of these effects. Third, although the models demonstrated outstanding fit given the exact fit test and fit indices, there were multiple large correlational residuals in both models. The conservative route was chosen for not making modifications to the models to make them fit better, but future researchers may want to examine the effects of these modifications in more detail. Fourth, the sample size for each model is relatively small for the expectations of structural equation modeling, which recommend 5 to 10 observations per parameter estimate (Bentler & Chou, 1987; Bollen, 1989; Nunnally, 1967). The models in the current study had about three observations per parameter estimate. This small sample size may make our estimates more unstable than if there was a larger sample. Future researchers may consider collecting a larger sample size to estimate the stability of the effects found in the current study. Finally, the model for those who have had COVID-19 while controlling for the severity of their symptoms explained 50.1% of the variability in their quality of life. Although this explained variability is substantial, there are other variables not measured in the current study that may explain the remaining 49.9% of the variability (i.e., risk perceptions, personality, or health coverage). Future researchers may want to consider exploring these extraneous variables.
Conclusion
The current study aimed to explain the negative relationship between the perceived danger of COVID-19 and quality of life through COVID-19 life changes and to test if this effect occurs differently between those who have had COVID-19 and those who have not. The results confirmed my hypothesis, but only in those that have had COVID-19. This study may guide future research away from the perceived danger of COVID-19 and onto remedying life changes from COVID-19. The current study and future research in this topic area may improve individuals’ quality of life and help make living with COVID-19 more manageable in the coming years.
References
Ahmed, O., Hossain, K. N., Siddique, R. F., & Jobe, M. C. (2021). COVID-19 fear, stress, sleep quality and coping activities during lockdown, and personality traits: A person-centered approach analysis. Personality and Individual Differences, 178,. https://doi.org/10.1016/j.paid.2021.110873
Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The Fear of COVID-19 Scale: Development and Initial Validation. International Journal of Mental Health and Addiction, 20(3), 1537–1545. https://doi.org/10.1007/s11469-020
Alkire, S., Nogales, R., Quinn, N. N., & Suppa, N. (2021). Global multidimensional poverty and COVID-19: A decade of progress at risk? Social Science & Medicine, 291, 114457. https://doi.org/10.1016/j.socscimed.2021.114457
Amdal, C. D., Pe, M., Falk, R. S., Piccinin, C., Bottomley, A., Arraras, J. I., Darlington, A. S., Hofsø, K., Holzner, B., Jørgensen, N. M. H., Kulis, D., Rimehaug, S. A., Singer, S., Taylor, K., Wheelwright, S., & Bjordal, K. (2021). Health-related quality of life issues, including symptoms, in patients with active COVID-19 or post COVID-19; A systematic literature review. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation, 30(12), 3367–3381. https://doi.org/10.1007/s11136-021-02908-z
Belen, H. (2022). A longitudinal examination of the association between fear of covid-19, resilience, and mental health during covid-19 outbreak. Psychology, Health & Medicine, 1–7,. https://doi.org/10.1080/13548506.2022.2073378
Bendau, A., Kunas, S. L., Wyka, S., Petzold, M. B., Plag, J., Asselmann, E., & Ströhle, A. (2021). Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. Journal of Anxiety Disorders, 79(102377). https://doi.org/10.1016/j.janxdis.2021.102377
Bentler, P. M., & Chou, C. P. (1987). Practical Issues in Structural Modeling. Sociological Methods & Research, 16(1), 78–117. https://doi.org/10.1177/0049124187016001004
Bhogal, A., Borg, B., Jovanovic, T., & Marusak, H. A. (2021). Are the kids really alright? Impact of COVID-19 on mental health in a majority Black American sample of schoolchildren. Psychiatry Research, 304(114146). https://doi.org/10.1016/j.psychres.2021.114146
Bollen, K. A. (1989). Structural equations with latent variables. John Wiley.
Brülhart, M., Klotzbücher, V., Lalive, R., & Reich, S. K. (2021). Mental health concerns during the COVID-19 pandemic as revealed by helpline calls. Nature, 600(7887), 121–126. https://doi.org/10.1038/s41586-021-04099-6
Buran, G., & Gerçek Öter, E. (2021a). Impact of the awareness and fear of covid-19 on menstrual symptoms in women: A cross-sectional study. Health Care for Women International. https://doi.org/10.1080/07399332.2021.2004149
Buran, G., & Gerçek Öter, E. (2021b). Impact of the awareness and fear of covid-19 on menstrual symptoms in women: A cross-sectional study. Health Care for Women International, 4, 413–427. https://doi.org/10.1080/07399332.2021.2004149
Case, J. B., Winkler, E. S., Errico, J. M., & Diamond, M. S. (2021). On the road to ending the COVID-19 pandemic: Are we there yet? Virology, 557, 70–85. https://doi.org/10.1016/j.virol.2021.02.003
De los Santos, J. A. A., & Labrague, L. J. (2021). The impact of fear of COVID-19 on job stress, and turnover intentions of frontline nurses in the community: A cross-sectional study in the Philippines. Traumatology, 27(1), 52–59. https://doi.org/10.1037/trm0000294
Demirbas, N., & Kutlu, R. (2021). Effects of covid-19 fear on society’s quality of life. International Journal of Mental Health and Addiction, 1–10,. https://doi.org/10.1007/s11469-021-00550-x
Duong, C. D. (2021). The impact of fear and anxiety of covid-19 on life satisfaction: Psychological distress and sleep disturbance as mediators. Personality and Individual Differences, 178(110869). https://doi.org/10.1016/j.paid.2021.110869
Egede, L. E., Walker, R. J., Dawson, A. Z., Zosel, A., Bhandari, S., Nagavally, S., Martin, I., & Frank, M. (2022). Short-term impact of covid-19 on quality of life, perceived stress, and serious psychological distress in an adult population in the midwest united states. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation, 8, 2387–2396. https://doi.org/10.1007/s11136-022-03081-7
Finney-Rutten, L. J., Zhu, X., Leppin, A. L., Ridgeway, J. L., Swift, M. D., Griffin, J. M., St. Sauver, J. L., Virk, A., & Jacobson, R. M. (2021). Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clinic Proceedings, 96(3), 699–707. https://doi.org/10.1016/j.mayocp.2020.12.024
Fried, E. I., Papanikolaou, F., & Epskamp, S. (2022). Mental health and social contact during the COVID-19 pandemic: An ecological momentary assessment study. Clinical Psychological Science, 10(2), 340–354. https://doi.org/10.1177/21677026211017839
Gamberini, L., Mazzoli, C. A., Sintonen, H., Colombo, D., Scaramuzzo, G., Allegri, D., Tonetti, T., Zani, G., Capozzi, C., Giampalma, E., Agnoletti, V., Becherucci, F., Bertellini, E., Castelli, A., Cappellini, I., Cavalli, I., Crimaldi, F., Damiani, F., Fusari, M., … & Spadaro, S. (2021). Quality of life of COVID-19 critically ill survivors after ICU discharge: 90 days follow-up. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation, 30(10), 2805–2817. https://doi.org/10.1007/s11136-021-02865-7
Gönenç, I. M., Öztürk Özen, D., & Yılmaz Sezer, N. (2022). The relationship between fear of covid-19, quality of sexual life, and sexual satisfaction of women in turkey. International Journal of Sexual Health. https://doi.org/10.1080/19317611.2022.2058145
Handberg, C., Werlauff, U., Højberg, A.-L., & Knudsen, L. F. (2021). Impact of the COVID-19 pandemic on biopsychosocial health and quality of life among Danish children and adults with neuromuscular diseases (NMD)—Patient reported outcomes from a national survey. PLoS ONE, 16(6). https://doi.org/10.1371/journal.pone.0253715
Hayes, B., Apputhurai, P., Mikocka-Walus, A., Barreiro-de Acosta, M., Bernstein, C. N., Burgell, R., Burisch, J., Bennebroek Evertsz, F., Ferreira, N., Graff, L. A., Trindade, I. A., Gearry, R., Lo, B., Mokrowiecka, A., Moser, G., Petrik, M., Stengel, A., & Knowles, S. R. (2021). Extending the common sense model to explore the impact of the fear of covid-19 on quality of life in an international inflammatory bowel disease cohort. Journal of Clinical Psychology in Medical Settings, 1–11,. https://doi.org/10.1007/s10880-021-09823-y
Huang, F., Sun, W., Zhang, L., Lu, H., & Chen, W.-T. (2022). Depressive symptoms mediate COVID-associated stigma and quality of life: Stigma instrument validation and path analysis. Journal of Affective Disorders, 297, 269–275. https://doi.org/10.1016/j.jad.2021.10.043
Huang, L., Yao, Q., Gu, X., Wang, Q., Ren, L., Wang, Y., Hu, P., Guo, L., Liu, M., Xu, J., Zhang, X., Qu, Y., Fan, Y., Li, X., Li, C., Yu, T., Xia, J., Wei, M., Chen, L., … & Cao, B. (2021). 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study. The Lancet, 398(10302), 747–758. https://doi.org/10.1016/S0140-6736(21)01755-4
Ioannidis, P. A. (2022). The end of the COVID-19 pandemic. European Journal of Clinical Investigation, 52(6), 1–12. https://doi.org/10.1111/eci.13782
Kayis, A. R., Satici, B., Deniz, M. E., Satici, S. A., & Griffiths, M. D. (2021). Fear of covid-19, loneliness, smartphone addiction, and mental wellbeing among the turkish general population: A serial mediation model. Behaviour & Information Technology. https://doi.org/10.1080/0144929X.2021.1933181 Advance Online Publication.
Khattak, S. R., Saeed, I., Rehman, S. U., & Fayaz, M. (2020). Impact of fear of covid-19 pandemic on the mental health of nurses in pakistan. Journal of Loss and Trauma. Advanced online publication. https://doi.org/10.1080/15325024.2020.1814580
Khudaykulov, A., Changjun, Z., Obrenovic, B., Godinic, D., Alsharif, H. Z. H., & Jakhongirov, I. (2022). The fear of covid-19 and job insecurity impact on depression and anxiety: An empirical study in china in the covid-19 pandemic aftermath. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues. Advanced online publication. https://doi.org/10.1007/s12144-022-02883-9
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford Press.
Koc, E. R., Demir, A. B., Topaloglu, E., Turan, O. F., & Ozkaya, G. (2022). Effects of quarantine applied during the COVID-19 pandemic on mental health and quality of life in patients with multiple sclerosis and healthy controls. Neurological Sciences, 43(4), 2263–2269. https://doi.org/10.1007/s10072-022-05901-7
Koenig, J., Kohls, E., Moessner, M., Lustig, S., Bauer, S., Becker, K., Thomasius, R., Eschenbeck, H., Diestelkamp, S., Gillé, V., Hiery, A., Rummel-Kluge, C., Kaess, M., Kaess, M., Bauer, S., Moessner, M., Koenig, J., Bonnet, S., Hammon, S., & Luntz, S. (2021). The impact of covid-19 related lockdown measures on self-reported psychopathology and health-related quality of life in german adolescents. European Child & Adolescent Psychiatry, 1–10,. https://doi.org/10.1007/s00787-021-01843-1
Kurzhals, J. K., Klee, G., Busch, H., Hagelstein, V., Zillikens, D., Terheyden, P., & Langan, E. A. (2021). The impact of the Covid-19 pandemic on quality of life in skin cancer patients. PLoS ONE, 16(8). https://doi.org/10.1371/journal.pone.0255501
Lee, S. A. (2020). Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Studies, 44(7), 393–401. https://doi.org/10.1080/07481187.2020
Lucas, P., Boyd, S., Milloy, M.-J., & Walsh, Z. (2021). Cannabis significantly reduces the use of prescription opioids and improves quality of life in authorized patients: Results of a large prospective study. Pain Medicine, 22(3), 727–739. https://doi.org/10.1093/pm/pnaa396
Mauer, V. A., Littleton, H., Lim, S., Sall, K. E., Siller, L., & Edwards, K. M. (2022). Fear of covid-19, anxiety, and social support among college students. Journal of American College Health, 1–8,. https://doi.org/10.1080/07448481.2022.2053689
Nadanovsky, P., & Dos Santos, A. P. P. (2020). Strategies to deal with the COVID-19 pandemic. Brazilian Oral Research, 34, e06err. https://doi.org/10.1590/1807-3107BOR-2020.vol34.0068err
Naghizadeh, S., & Mirghafourvand, M. (2021). Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Archives of Psychiatric Nursing, 35(4), 364–368. https://doi.org/10.1016/j.apnu.2021.05.006
Nunnally, J. C. (1967). Psychometric Theory. McGraw-Hill.
Peker, A., & Cengiz, S. (2021). Covid-19 fear, happiness and stress in adults: The mediating role of psychological resilience and coping with stress. International Journal of Psychiatry in Clinical Practice, 1–9,. https://doi.org/10.1080/13651501.2021.1937656
Rocco, I., Bonati, M., Corso, B., & Minicuci, N. (2021). Quality of life improvement in children with attention‐deficit hyperactivity disorder reduces family’s strain: A structural equation model approach. Child: Care, Health and Development, 47(5), 667–674. https://doi.org/10.1111/cch.12874
Rogers, A. M., Lauren, B. N., Woo Baidal, J. A., Ozanne, E. M., & Hur, C. (2021). Persistent effects of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life: A longitudinal study among U.S. adults. Appetite, 167, 105639. https://doi.org/10.1016/j.appet.2021.105639
Rosseel, Y. (2012). Lavaan: An R package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1–36. https://doi.org/10.18637/jss.v048.i02
Saikia, U., Dodd, M. M., Chalmers, J., Dasvarma, G., & Schech, S. (2021). COVID-19, individual wellbeing and multi-dimensional poverty in the state of South Australia. PLoS ONE, 16(6). https://doi.org/10.1371/journal.pone.0252898
Saracoglu, K. T., Simsek, T., Kahraman, S., Bombaci, E., Sezen, Ö., Saracoglu, A., & Demirhan, R. (2020). The psychological impact of COVID-19 disease is more severe on intensive care unit healthcare providers: A cross-sectional study. Clinical Psychopharmacology and Neuroscience, 18(4), 607–615. https://doi.org/10.9758/cpn.2020.18.4.607
Shoychet, G., Lenton-Brym, A. P., & Antony, M. M. (2022). The impact of COVID-19 anxiety on quality of life in Canadian adults: The moderating role of intolerance of uncertainty and health locus of control. Canadian Journal of Behavioural Science. Advanced online publication. https://doi.org/10.1037/cbs0000331
Stamatis, C. A., Broos, H. C., Hudiburgh, S. E., Dale, S. K., & Timpano, K. R. (2022). A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. British Journal of Clinical Psychology, 61(2), 385–404. https://doi.org/10.1111/bjc.12351
Stone, B. M. (2022). Development and Validation of the COVID-19 Impact Domain Scale (CIDS). preprint manuscript, ResearchGate. https://doi.org/10.13140/RG.2.2.24552.75529
Sugawara, D., Masuyama, A., & Kubo, T. (2021). Socioeconomic impacts of the covid-19 lockdown on the mental health and life satisfaction of the japanese population. International Journal of Mental Health and Addiction. Advanced online publication. https://doi.org/10.1007/s11469-020-00461-3
Suhail, A., Dar, K. A., & Iqbal, N. (2022). COVID-19 related fear and mental health in Indian sample: The buffering effect of support system. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues, 41(1), 480–491. https://doi.org/10.1007/s12144-021-01694-8
Trucco, E. M., Fallah-Sohy, N., Hartmann, S. A., Cristello, J. V., Comer, J. S., & Sutherland, M. T. (2022). The impact of covid-19 experiences on adolescent internalizing problems and substance use among a predominantly latinx sample. Journal of Youth and Adolescence, 51(5), 821–831. https://doi.org/10.1007/s10964-022-01593-6
Vilca, L. W., Chávez, B. V., Fernández, Y. S., Caycho-Rodríguez, T., & White, M. (2022). Impact of the fear of catching covid-19 on mental health in undergraduate students: A predictive model for anxiety, depression, and insomnia. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues. Advanced online publication. https://doi.org/10.1007/s12144-021-02542-5
West, S. G., Finch, J. F., & Curran, P. J. (1995). Structural equation models with nonnormal variables: Problems and remedies. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Sage Publications Inc.
World Health Organization. (1996). WHOQOL-Bref : Introduction, administration, scoring and generic version of the assessment: Field trial version, December 1996. World Health Organization. Retrieved April 11, 2022, from https://apps.who.int/iris/handle/10665/63529
World Health Organization. (2022). Who coronavirus (COVID-19) dashboard. World Health Organization. Retrieved April 6, 2022, from https://covid19.who.int/
Yenen, E. T., & Çarkit, E. (2021). Fear of covid-19 and general self-efficacy among Turkish teachers: Mediating role of perceived social support. Current Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues.Advanced online publication. https://doi.org/10.1007/s12144-021-02306-1
Zuckerman, M. (1999). Diathesis-stress models. In M. Zuckerman, Vulnerability to psychopathology: A biosocial model (pp. 3–23). American Psychological Association. https://doi.org/10.1037/10316-001
Author information
Authors and Affiliations
Contributions
The first author confirms that he is the sole contributor to the current work.
Corresponding author
Ethics declarations
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
This study was approved by the Institutional Review Board at Southern Illinois University.
Consent to participate
Participants read and agreed to an informed consent document and were debriefed at the end of the study.
Consent to publish
The authors affirm that human research participants provided informed consent for the publication of their anonymized data.
Open practice statement
The data, scripts, and materials for this paper are available on the OSF (https://osf.io/3yqtv/?view_only=f3800dc28cf74f739b46ac8c0296ad9a). This study was not pre-registered.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stone, B.M. The explanatory ability of COVID-19 life changes on quality of life: A comparison of those who have had and not had COVID-19. Curr Psychol 43, 13923–13934 (2024). https://doi.org/10.1007/s12144-022-03504-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03504-1