Abstract
Objective
To understand epidemiology of the neonatal and infant deaths in predominant areas of two tribal districts of Gujarat.
Methods
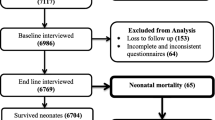
A secondary analysis of pregnancy and mortality surveillance data was done to understand the causes and determinants of infant deaths in predominant tribal areas of two districts of Gujarat, India from 2015 to 2018. All pregnancies, their outcomes, and infant deaths were prospectively registered. A verbal autopsy tool was used to understand the cause of death.
Result
A total of 25,130 live births were recorded; 20,994 (83.5%) deliveries occurred at the hospital. Total 1,309 infant deaths (IMR - 52.08/1,000 live births) and 879 neonatal deaths (NMR - 34.97/1,000 live births) occurred during the program duration. The odds of infant deaths was high among male child aOR - 1.5 (CI:1.3–1.7, p < 0.001), born to illiterate/primary educated mother aOR - 1.2 (1.03–1.4, 0.013), born at home or on the way aOR - 1.4 (1.1–1.8, 0.003), born with low birth weight (< 2.5 kg), aOR - 3.7 (3.2–4.3, < 0.001), born preterm (< 37 wk) aOR - 1.9 (1.7–2.2, < 0.001), and born twins aOR - 1.5 (1–2.1, 0.037) in comparison to female child, born to secondary/or above educated mother, born in hospital, born normal weight (>= 2.5 kg), born full-term (>= 37 wk), and born single, respectively. The asphyxia/respiratory distress syndrome (RDS) 282 (56%), sepsis/pneumonia and asphyxia/RDS 188 (63%), and sepsis/pneumonia 281 (65%) were leading cause of death among 0–3 d, 4–28 d, and 29–365 d infant deaths.
Conclusion
There is a need to improve quality of intrapartum and postpartum care. Additionally, sepsis detection among infants and referral by community health workers also need to be improved to reduce infant mortality due to sepsis.

Similar content being viewed by others
Data Availability
Dataset is available at: https://www.dropbox.com/s/y6obgqzj12tqsik/Dataset1.xlsx?dl=0. The personally identifiable information has been removed.
References
World Health Organization. Sustainable development goals.World Health Organization.Available at: https://www.who.int/health-topics/sustainable-development-goals#tab=tab_1. Accessed on 29 Aug 2020.
Registrar General, India, Minitsry of Home Affairs, GOI. SRS Bulletin - Sample Registration System. 2014. Available at: https://censusindia.gov.in/vital_statistics/SRS_Bulletins/SRS%20Bulletin%20-Sepetember%202014.pdf. Accessed on 18 Feb 2022.
Office of the Registrar General, India, GOI. SRS Bulletin- Sample Registration System. 2019. Available at: http://censusindia.gov.in/vital_statistics/SRS_Bulletins/SRS_Bulletin-Rate-2017-_May_2019.pdf. Accessed on 26 Aug 2020.
Ministry of Health & Family Welfare and Ministry of Tribal Affairs, GOI. Report of the expert committee on tribal health. Tribal Health in India - Bridging the gap and roadmap for the future. 2014. Available at: http://nhm.gov.in/nhm_components/tribal_report/Executive_Summary.pdf. Accessed on 28 Aug 2020.
Bhatia M, Dwivedi LK, Ranjan M, Dixit P, Putcha V. Trends, patterns and predictive factors of infant and child mortality in well-performing and underperforming states of India: A secondary analysis using National Family Health Surveys. BMJ Open. 2019;9:e023875.
Shah PP, Modi DK, Shah SP, Desai SA. Effect of maternity schemes on place of delivery in a tribal block of Gujarat. Indian J Community Med. 2013;38:118–20.
Kutty VR, Shah P, Modi D, Shah S, Ramanathan M, Archana AR. Reducing neonatal mortality in Jhagadia block, Gujarat: We need to go beyond promoting hospital deliveries. J Trop Pediatr. 2013;59:49–53.
Modi D, Desai S, Dave K, et al. Cluster randomized trial of a mHealth intervention “ImTeCHO” to improve delivery of proven maternal, neonatal, and child care interventions through community-based Accredited Social Health Activists (ASHAs) by enhancing their motivation and strengthening supervision in tribal areas of Gujarat, India: study protocol for a randomized controlled trial. Trials. 2017;18:270.
Modi D, Dholakia N, Gopalan R, et al. mHealth intervention “ImTeCHO” to improve delivery of maternal, neonatal, and child care services-A cluster-randomized trial in tribal areas of Gujarat, India. PLoS Med. 2019;16:e1002939.
Modi D, Saha S, Vaghela P, et al. Costing and cost-effectiveness of a mobile health intervention (ImTeCHO) in improving infant mortality in tribal areas of Gujarat, India: cluster randomized controlled trial. JMIR MHealth UHealth. 2020;8:e17066.
Garenne M, Fauveau V. Potential and limits of verbal autopsies. Bull World Health Organ. 2006;84:164.
Ranjan M, Dwivedi LK, Mishra R, et al. Infant mortality differentials among the tribal and non-tribal populations of Central and Eastern India. Int J Popul Stud. 2017;2:26–43.
Narwal R, Gram L. Has the rate of reduction in infant mortality increased in India since the launch of National Rural Health Mission? Analysis of time trends 2000–2009 with projection to 2015. Int J MCH AIDS. 2013;2:139–52.
Rai SK, Kant S, Srivastava R, et al. Causes of and contributors to infant mortality in a rural community of North India: Evidence from verbal and social autopsy. BMJ Open. 2017;7:e012856.
Million Death Study Collaborators, Bassani DG, Kumar R, Awasthi S, et al. Causes of neonatal and child mortality in India: A nationally representative mortality survey. Lancet. 2010;376:1853–60.
Peterson S, Nsungwa-Sabiiti J, Were W, et al. Coping with paediatric referral – Ugandan parents’ experience. Lancet. 2004;363:1955–6.
Pagel C, Prost A, Hossen M, et al. Is essential newborn care provided by institutions and after home births? Analysis of prospective data from community trials in rural South Asia. BMC Pregnancy Childbirt. 2014;14:99.
Malhotra S, Zodpey SP, Vidyasagaran AL, et al. Assessment of essential newborn care services in secondary-level facilities from two districts of India. J Health Popul Nutr. 2014;3:130–41.
Fadel SA, Ram U, Morris SK, et al. Facility delivery, postnatal care and neonatal deaths in India: nationally-representative case-control studies. 2015;10:e0140448.
Ministry of Health & Family Welfare, GOI. Operational Guidelines: Use of Gentamicin by ANMs for management of sepsis in young infants under specific situations. 2014. Available at: http://tripuranrhm.gov.in/Guidlines/2606201401.pdf. Accessed on 18 Feb 2022.
World Health Organization. GUIDELINE: managing possible serious bacterial infection in young infants when referral is not feasible. 2015. Available at: https://www.who.int/publications/i/item/9789241509268. Accessed on 18 Feb 2022.
Goyal N, Rongsen-Chandola T, Sood M, et al. Management of possible serious bacterial infection in young infants closer to home when referral is not feasible: Lessons from implementation research in Himachal Pradesh, India. PLoS One. 2020;15:e0243724.
SEWA Rural. Report on family centered safe motherhood and newborn care project. 2014. Available at: https://sewarural.org/sewa/wp-content/uploads/2014/08/Safe-motherhood-and-New-Born-Care-Book-1.pdf. Accessed on 18 Feb 2022.
International Institute for Population Sciences. District Level Household and Facility Survey 2007–08. India: New Delhi; 2010. Available at: http://rchiips.org/pdf/india_report_dlhs-3.pdf. Accessed on 18 Feb 2022.
National Health Systems Resource Centre. ASHA: Which way forward...? Executive Summary - Evaluation of ASHA Programme. 2011. Available at: https://nhm.gov.in/images/pdf/communitisation/asha/Studies/Evaluation_of_ASHA_Program_2010-11_Report.pdf. Accessed on 18 Feb 2022.
Acknowledgements
The authors thank all respondents for their support; data collection team, supervisors and other staff for their contribution; Dr. C. Palnivel for his guidance and support during statistical analysis; Ms. Shradha Patel for English grammar proofreading.
Funding
The study was funded by Indian Council of Medical Research (Grant ID number 5/7/589/Gujarat/ 2011-RCH, website: https://www.icmr.nic.in/), the John D. and Catherine T. MacArthur Foundation (Grant number G-108398–0, website: https://www.macfound.org/), and Department of Maternal, Neonatal, Child and Adolescent Health at the World Health Organization (Grant number MCA-00615, website: https://www.who.int/maternal_child_adolescent/en/). All grants were awarded to the principal investigator PS from SEWA Rural. The funders had no role in study design, data collection and analysis, decision to publish, or preparations of the manuscript.
Author information
Authors and Affiliations
Contributions
KD involved in monitoring of the data collection, performed analysis of the data and drafted the manuscript; DM, PS, SD conceptualized the study, finalized the study design, oversaw the data collection progress, and critically reviewed and revised the manuscript; All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. PS will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Approval
Permission was obtained from the “SEWA-Rural Institutional Ethics Committee” to do this study as a nested study, part of ImTeCHO cluster randomized trial.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dave, K., Shah, P., Desai, S. et al. Epidemiology of Infant Deaths in Predominant Tribal Areas of Two Districts of Gujarat: Results of Pregnancy and Mortality Surveillance Program. Indian J Pediatr 89, 776–784 (2022). https://doi.org/10.1007/s12098-022-04123-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04123-1