Abstract
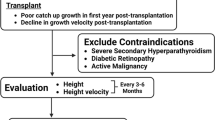
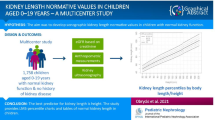
Short stature is a common presentation to pediatricians with a significant overlap between physiology and pathology. Thus, while most short children have a physiological cause, growth failure may be the only manifestation of severe underlying disease. Growth failure evaluation aims to avoid unnecessary investigations in children with a physiological cause without missing pathology. Guidelines for the evaluation of short stature allow stepwise evaluation but are limited by their resource-intense nature. An objective application of anthropometric indices and careful clinical evaluation allows rational growth failure workup. The use of height standard deviation score (SDS) for determining the need for evaluation (no evaluation above −2, follow-up between −2 to −3, and immediate workup with height below −3), corrected height SDS to identify familial short stature (above −1.5), height SDS for bone age for constitutional delay of puberty and growth (above −2), and BMI SDS for nutritional pattern growth failure (below −1) helps reduce the burden of investigations. The present review provides a framework for comprehensive growth evaluation across resource levels and settings.



Similar content being viewed by others
References
Murray PG, Clayton PE. Disorders of growth. In: Dattani M, Brook C.G.D, Eds. Brook’s clinical pediatric endocrinology, 7th Ed. Oxford: Wiley publ; 2019. p.229–33.
Bajpai A, Agarwal N. Growth failure. In: Bajpai A, Patel R, Dave C, Agarwal N, eds. MedEclasses Pediatric endocrinology. Kanpur: Grow society publ; 2019. p. 49–53.
Wit JM, Kamp GA, Oostdijk W. Towards a rational and efficient diagnostic approach in children referred for growth failure to the general paediatrician. Horm Res Paediatr. 2019;91:223–40.
Oostdijk W, Grote FK, de Muinck Keizer-Schrama SM, Wit JM. Diagnostic approach in children with short stature. Horm Res. 2009;72:206–17.
Patel R, Dave C, Agarwal N, et al. Predictive value of IAP 2015, IAP 2007 and WHO growth charts in identifying pathological short stature. Indian Pediatr. 2021;58:149–51.
Khadilkar V, Khadilkar A, Arya A, et al. Height velocity percentiles in Indian children aged 5–17 years. Indian Pediatr. 2019;56:23–8.
Patel R, Bajpai A. Growth disorders. In: Bajpai A, Eds. Practical Pediatric Endocrinology. New Delhi: IJP Publications, 2021.p.17-31
Agarwal N, Patel R. Growth failure. In: Growth Disorders. MedEClasses Online course in Pediatric Endocrinology. Available at: https://learning.growsociety.in/unit/growthfailure.Accessed on 10 July 2021
Khadilkar V, Yadav S, Agrawal KK, et al. Revised IAP growth charts for height, weight, and body mass index for 5-to 18-Year-old Indian children. Indian Pediatr. 2015;52:47–55.
Greulich WW, Pyle SJ. Radiographic atlas of skeletal development of the hand and wrist. 2nd ed. California: Stanford University Press; 1959.
Tanner JM, Healy MJR, Goldstein H, Cameron N. Assessment of skeletal maturity and prediction of adult height (TW3 method). 3rd ed. London: W.B. Saunders; 2001.
Thodberg HH. Clinical review: an automated method for determination of bone age. J Clin Endocrinol Metab. 2009;94:2239–44.
Wright CM, Cheetham TD. The strengths and limitations of parental heights as a predictor of attained height. Arch Dis Child. 1999;81:257–60.
Fine RN. Growth retardation in children with chronic renal insufficiency. Nephron. 1997;76:125–9.
Langeveld M, Hollak CE. Bone health in patients with inborn errors of metabolism. Rev Endocr Metab Disord. 2018;19:81–92.
Bhadada SK, Bhansali A, Kochhar R, et al. Does every short stature child need screening for celiac disease? J Gastroenterol Hepatol. 2008;23:e353–6.
Singh P, Sharma PK, Agnihotri A, et al. Coeliac disease in patients with short stature: a tertiary care center experience. Natl Med J India. 2015;28:176–80.
Husby S, Koletzko S, Korponay-Szabó I, et al. European society paediatric gastroenterology, hepatology and nutrition guidelines for diagnosing coeliac disease 2020. J Pediatr Gastroenterol Nutr. 2020;70:141–56.
Collett-Solberg PF, Ambler G, Backeljauw PF, et al. Diagnosis, genetics, and therapy of short stature in children: a growth hormone research society international perspective. Horm Res Paediatr. 2019;92:1–14.
Blum WF, Alherbish A, Alsagheir A, et al. The growth hormone-insulin-like growth factor-I axis in the diagnosis and treatment of growth disorders. Endocr Connect. 2018;7:R212–22.
Shen Y, Zhang J, Zhao Y, et al. Diagnostic value of serum IGF-1 and IGFBP-3 in growth hormone deficiency: a systematic review with meta-analysis. Eur J Pediatr. 2015;174:419–27.
Van Buuren S, van Dommelen P, Zandwijken GR, Grote FK, Wit JM, Verkerk PH. Towards evidence based referral criteria for growth monitoring. Arch Dis Child. 2004;89:336–41.
Gravholt CH, Andersen NH, Conway GS, et al. Clinical practice guidelines for the care of girls and women with turner syndrome: proceedings from the 2016 cincinnati international turner syndrome meeting. Eur J Endocrinol. 2017;177:G1-70.
Grimberg A, DiVall SA, Polychronakos C, et al. Guidelines for growth hormone and insulin-like growth factor–I treatment in children and adolescents: growth hormone deficiency, idiopathic short stature, and primary insulin-like growth factor-I deficiency. Horm Res Paediatr. 2016;86:361–97.
Author information
Authors and Affiliations
Contributions
RP and AB were involved in the planning, drafting, and review of the manuscript. AB is the guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, R., Bajpai, A. Evaluation of Short Stature in Children and Adolescents. Indian J Pediatr 88, 1196–1202 (2021). https://doi.org/10.1007/s12098-021-03880-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-021-03880-9