Abstract
Objectives
To detect Cytotoxic T- Lymphocyte Antigen-4 (CTLA4) single nucleotide polymorphisms (SNPs) at +49A/G (rs231775) and -318C/T (rs5742909) positions in children with idiopathic nephrotic syndrome (INS) and also assay urinary soluble CTLA4 (sCTLA4) levels in children with minimal change disease (MCD), focal segmental glomerulosclerosis (FSGS) and steroid sensitive nephrotic syndrome (SSNS) in remission.
Methods
The study included 59 patients of INS (MCD-23, FSGS-15 and SSNS in remission-21) and 35 healthy controls. The CTLA4 SNPs profiling was done in peripheral blood mononuclear cells and urinary sCTLA4 level was assayed by ELISA kit.
Results
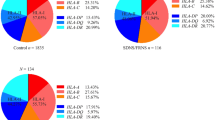
Although frequency of homozygous +49 GG (rs4553808) genotype (26.3% vs. 11.4%; p = 0.231) and G allele (52.6% vs. 40%; p = 0.216) were found to be higher in INS as compared to controls, the differences were statistically non-significant. Genotypes GG, AG, AA and alleles A and G frequencies were comparable among MCD, FSGS and controls. SNP at −318 C/T (rs5742909) did not show homozygous TT genotype both in INS as well as controls. Median urinary sCTLA4/creatinine level was significantly higher in MCD as compared to FSGS (p = 0.027), SSNS in remission (p = 0.001) and controls (p = 0.003).
Conclusions
The positive associations of +49 GG genotype and G allele in patients with nephrotic syndrome were not observed. The frequencies did not differ significantly among MCD, FSGS and controls. Urinary sCTLA4 level was significantly increased in MCD; suggesting its possible role in the pathogenesis of disease.



Similar content being viewed by others
References
Shalhoub RJ. Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet. 1974;2:556–60.
Koyama A, Fujisaki M, Kobayashi M, Igarashi M, Narita M. A glomerular permeability factor produced by human T cell hybridomas. Kidney Int. 1991;40:453–60.
Daniel V, Trautmann Y, Konrad M, Nayir A, Schärer K. T-lymphocyte populations, cytokines and other growth factors in serum and urine of children with idiopathic nephrotic syndrome. Clin Nephrol. 1997;47:289–97.
Matsumoto K, Kanmatsuse K. Elevated interleukin-18 levels in the urine of nephrotic patients. Nephron. 2001;88:334–9.
McCarthy ET, Sharma M, Savin VJ. Circulating permeability factors in idiopathic nephrotic syndrome and focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2010;5:2115–21.
Reiser J, von Gersdorff G, Loos M, et al. Induction of B7–1 in podocytes is associated with nephrotic syndrome. J Clin Invest. 2004;113:1390–7.
Garin EH, Diaz LN, Mu W, et al. Urinary CD80 excretion increases in idiopathic minimal change disease. J Am Soc Nephrol. 2009;20:260–6.
Garin EH, Mu W, Arthur JM, et al. Urinary CD80 is elevated in minimal change disease but not in focal segmental glomerulosclerosis. Kidney Int. 2010;78:296–302.
Mishra OP, Kumar R, Narayan G, et al. Toll-like receptor 3 (TLR-3), TLR-4 and CD80 expression in peripheral blood mononuclear cells and urinary CD80 levels in children with idiopathic nephrotic syndrome. Pediatr Nephrol. 2017;32:1355–61.
Lindsten T, Lee KP, Harris ES, et al. Characterisation of CTLA-4 structure and expression on human T cells. J Immunol. 1993;151:3489–99.
Linsley PS, Brady W, Urnes M, Grosmaire LS, Damle NK, Ledbetter JA. CTLA-4 is a second receptor for the B cell activation antigen B7. J Exp Med. 1991;174:561–9.
Karandikar NJ, Vanderlugt CL, Walunas TL, Miller SD, Bluestone JA. CTLA-4: a negative regulator of autoimmune disease. J Exp Med. 1996;184:783–8.
Cara-Fuentes G, Wasserfall CH, Wang H, Johnson RJ, Garin EH. Minimal change disease: a dysregulation of the podocyte CD80-CTLA-4 axis? Pediatr Nephrol. 2014;29:2333–40.
Shimada M, Araya C, Rivard C, Ishimoto T, Johnson RJ, Garin EH. Minimal change disease: a ‘ two-hit’ podocyte immune disorder? Pediatr Nephrol. 2011;26:645–9.
Mäurer M, Loserth S, Kolb-Mäurer A, et al. A polymorphism in the human cytotoxic T-lymphocyte antigen 4 (CTLA4) gene (exon 1 +49) alters T-cell activation. Immunogenetics. 2002;54:1–8.
Carr EJ, Niederer HA, Williams J, et al. Confirmation of the genetic association of CTLA4 and PTPN22 with ANCA-associated vasculitis. BMC Med Genet. 2009;10:121.
Lei C, Dongqing Z, Yeqing S, et al. Association of the CTLA-4 gene with rheumatoid arthritis in the Chinese Han population. Eur J Hum Genet. 2005;13:823–8.
Wang JJ, Shi YP, Yue H, Chun W, Zou LP. CTLA-4 exon 1 +49A/G polymorphism is associated with renal involvement in pediatric Henoch-Schönlein purpura. Pediatr Nephrol. 2012;27:2059–64.
Spink C, Stege G, Tenbrock K, Harendza S. The CTLA-4 +49GG genotype is associated with susceptibility for nephrotic kidney diseases. Nephrol Dial Transplant. 2013;28:2800–5.
Ohl K, Eberhardt C, Spink C, et al. CTLA4 polymorphisms in minimal change nephrotic syndrome in children: a case-control study. Am J Kidney Dis. 2014;63:1074–5.
Ishimoto T, Shimada M, Araya CE, Huskey J, Garin EH, Johnson RJ. Minimal change disease: a CD80 podocytopathy. Semin Nephrol. 2011;31:320–5.
Indian Pediatric Nephrology Group, Indian Academy of Pediatrics. Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr. 2008;45:203–14.
Gulati A, Bagga A, Gulati S, Mehta KP, Vijayakumar M; Indian Society of Pediatric Nephrology. Management of steroid resistant nephrotic syndrome. Indian Pediatr. 2009;46:35–47.
Ligers A, Teleshova N, Masterman T, Huang WX, Hillert J. CTLA-4 gene expression is influenced by promoter and exon 1 polymorphisms. Genes Immun. 2001;2:145–52.
Author information
Authors and Affiliations
Contributions
OPM, PC and RP: Involved in the study design, conduction, data analysis and drafting of manuscript; AS, AA: Helped in data analysis and drafting of manuscript; GN: Helped in genetic analysis; PS: Performed assay of urinary sCTLA4; VVB: Examined the histopathology of renal tissues. OPM will act as guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
The study was supported by the Institutional Grants of Department of Pediatrics, Institute of Medical Sciences and School of Biochemical Engineering, Indian Institute of Technology, Banaras Hindu University, Varanasi, India.
Rights and permissions
About this article
Cite this article
Mishra, O.P., Chhabra, P., Narayan, G. et al. Cytotoxic T- Lymphocyte Antigen-4 (CTLA4) Gene Expression and Urinary CTLA4 Levels in Idiopathic Nephrotic Syndrome. Indian J Pediatr 86, 26–31 (2019). https://doi.org/10.1007/s12098-018-2734-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-018-2734-9