Abstract
Objective
Contouring accuracy is critical in modern radiotherapy. Several tools are available to assist clinicians in this task. This study aims to evaluate the performance of the smoothing tool in the ARIA system to obtain more consistent volumes.
Methods
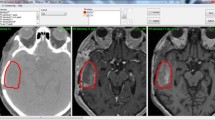
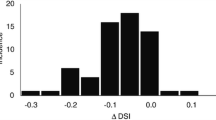
Eleven different geometric shapes were delineated in ARIA v15.6 (Sphere, Cube, Square Prism, Six-Pointed Star Prism, Arrow Prism, And Cylinder and the respective volumes at 45° of axis deviation (_45)) in 1, 3, 5, 7, and 10 cm side or diameter each. Post-processing drawing tools to smooth those first-generated volumes were applied in different options (2D-ALL vs 3D) and grades (1, 3, 5, 10, 15, and 20). These volumetric transformations were analyzed by comparing different parameters: volume changes, center of mass, and DICE similarity coefficient index. Then we studied how smoothing affected two different volumes in a head and neck cancer patient: a single rounded node and the volume delineating cervical nodal areas.
Results
No changes in data were found between 2D-ALL or 3D smoothing. Minimum deviations were found (range from 0 to 0.45 cm) in the center of mass. Volumes and the DICE index decreased as the degree of smoothing increased. Some discrepancies were found, especially in figures with cleft and spikes that behave differently. In the clinical case, smoothing should be applied only once throughout the target delineation process, preferably in the largest volume (PTV) to minimize errors.
Conclusion
Smoothing is a good tool to reduce artifacts due to the manual delineation of radiotherapy volumes. The resulting volumes must be always carefully reviewed.






Similar content being viewed by others
Data availability
Not applicable.
References
Vrtovec T, Mocnik D, Strojan P, Pernus F, Ibragimov B. Auto-segmentation of organs at risk for head and neck radiotherapy planning: from atlas-based to deep learning methods. Med Phys. 2020;47(9):e929–50.
Van Dijk LV, Van den Bosch L, Aljabar P, Peressutti D, Both S, Steenbakkers RJHM. Improving automatic delineation for head and neck organs at risk by Deep Learning Contouring. Radiother Oncol. 2020;142:115–23.
Baroudi H, Brock KK, Cao W, Chen X, Chung C, Court LE, et al. Automated contouring and planning in radiation therapy: what is ‘clinically acceptable’? Diagnostics. 2023;13:667.
Apolle R, Appold S, Bijl HP, Blanchard P, Bussink J, Faivre-Finn C, et al. Inter-observer variability in target delineation increases during adaptive treatment of head-and-neck and lung cancer. Acta Oncol. 2019;58(No. 10):1378–85.
Van der Veen J, Gulyban A, Willems S, Maes F, Nuyts S. Interobserver variability in organ at risk delineation in head and neck cancer. Radiat Oncol. 2021;16:120.
Nelms BE, Tomé WA, Robinson G, Wheeler J. Variations in the contouring of OAR: test case from a patient with oropharyngeal cancer. Int J Radiat Oncol Biol Phys. 2012;82(1):368–78.
Vinod SK, Min M, Jameson MG, Holloway LC. A review of interventions to reduce inter-observer variability in volume delineation in radiation oncology. J Med Imaging Radiat Oncol. 2016;60:393–406.
Vinod SK, Min M, Jameson MG, and Holloway LC. Uncertainties in volume delineation in radiation oncology: a systematic review and recommendations for future studies. Radiother Oncol. 2016;121(2):169–79.
Van der Veen J, Willems S, Bollen H, Maes F, Nuyts S. Interobserver variability in delineation of target volumes in head and neck cancer. Radiother Oncol. 2019;137:9–15.
González PJ, Simões R, Kiers K, Janssen TM. Explaining the dosimetric impact of contouring errors in head and neck radiotherapy. Biomed Phys Eng Express. 2022;8(5):055001.
Sadeghi S, Siavashpour Z, Vafaei Sadr A, Farzin M, Sharp R, Gholami S. A rapid review of influential factors and appraised solutions on organ delineation uncertainties reduction in radiotherapy. Biomed Phys Eng Express. 2021;7(5):052001.
Feng M, Demiroz C, Vineberg KA, Eisbruch A, Balter JM. Normal tissue anatomy for oropharyngeal cancer: contouring variability and its impact on optimization. Int J Radiat Oncol Biol Phys. 2012;84(2):e245–9.
Njeh CF. Tumor delineation: the weakest link in the search for accuracy in radiotherapy. J Med Phys. 2008;33(4):136–40.
Kumar S, Holloway L, Boxer M, Yap ML, Chlap P, Moses D, et al. Variability of gross tumour volume delineation: MRI and CT based tumour and lymph node delineation for lung radiotherapy. Radiother Oncol. 2022;167:292–9.
De la Pinta C, García LaTorre R, Martínez-Lorca A, Fernández E, Hernanz R, Martín M, et al. Interobserver variability in gross tumor volume contouring in non-spine bone metastases. J Clin Transl Res. 2022;8(6):465–9.
Giaj-Levra N, Figlia V, Cuccia F, Mazzola R, Nicosia L, Ricchetti F, et al. Reduction of inter-observer differences in the delineation of the target in spinal metastases SBRT using an automatic contouring dedicated system. Radiat Oncol. 2021;16:197.
Lorenzen EL, Kallehauge JF, Byskov CS, Dahlrot RH, Haslund CA, Guldberg TL, et al. A national study on the inter-observer variability in the delineation of organs at risk in the brain. Acta Oncol. 2021;60(11):1548–54.
White I, Hunt A, Bird T, Settatree S, Soliman H, McQuaid D, et al. Interobserver variability in target volume delineation for CT/MRI simulation and MRI-guided adaptive radiotherapy in rectal cancer. Br J Radiol. 2021;94:20210350.
Chang X, Deng W, Wang X, Zhou Z, Yang J, Guo W, et al. Interobserver variability in target volume delineation in definitive radiotherapy for thoracic esophageal cancer: a multi-center study from China. Radiat Oncol. 2021;16:102.
Kim KS, Cheong KH, Kim K, Koo T, Koh HK, Chang JH, et al. Interobserver variability in clinical target volume delineation in anal squamous cell carcinoma. Sci Rep. 2021;11:2785.
Gkika E, Tanadini-Lang S, Kirste S, Holzner PA, Neeff HP, Rischke HC, et al. Interobserver variability in target volume delineation of hepatocellular carcinoma. Strahlenther Onkol. 2017;193(10):823–30.
Onal C, Cengiz M, Guler OC, Dolek Y, Ozkok S. The role of delineation education programs for improving interobserver variability in target volume delineation in gastric cancer. Br J Radiol. 2017;90:20160826.
Piva C, Genovesi D, Filippi AR, Balducci M, Barra S, Buglione M, et al. Interobserver variability in clinical target volume delineation for primary mediastinal B-cell lymphoma. Pract Radiat Oncol. 2015;5:383–9.
Eminowicz G, McCormack M. Variability of clinical target volume delineation for definitive radiotherapy in cervix cancer. Radiother Oncol. 2015;117:542–7.
Guo B, Li J, Wang W, Xu M, Shao Q, Zhang Y, et al. Interobserver variability in the delineation of the tumour bed using seroma and surgical clips based on 4DCT scan for external-beam partial breast irradiation. Radiat Oncol. 2015;10:66.
Genovesia D, Cèfaroa GA, Trignania M, Vinciguerraa A, Augurioa A, Di Tommaso M, et al. Interobserver variability of clinical target volume delineation in soft-tissue sarcomas. Cancer/Radiothér. 2014;18:89–96.
Caravatta L, Macchia G, Mattiucci GC, Sainato A, Cernusco NLV, Mantello G, et al. Inter-observer variability of clinical target volume delineation in radiotherapy treatment of pancreatic cancer: a multi-institutional contouring experience. Radiat Oncol. 2014;9:198.
Trignani M, Argenone A, Di Biase S, Musio D, Merlotti A, Ursino S, et al. Inter‑observer variability of clinical target volume delineation in definitive radiotherapy of neck lymph node metastases from unknown primary. A cooperative study of the Italian Association of Radiotherapy and Clinical Oncology (AIRO) Head and Neck Group. La Radiologia Medica. 2019;124(7):682–92.
Lim JY, Leech M. Use of auto-segmentation in the delineation of target volumes and organs at risk in head and neck. Acta Oncol. 2016;55(7):799–806.
Aliotta E, Nourzadeh H, Siebers J. Quantifying the dosimetric impact of organ-at-risk delineation variability in head and neck radiation therapy in the context of patient setup uncertainty. Phys Med Biol. 2019;64:135020.
Funding
The authors received no specific funding for their participation in this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethical approval (Research involving human participants and animals)
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marruecos Querol, J., Jurado-Bruggeman, D., Lopez-Vidal, A. et al. Contouring aid tools in radiotherapy. Smoothing: the false friend. Clin Transl Oncol (2024). https://doi.org/10.1007/s12094-024-03420-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12094-024-03420-9