Abstract
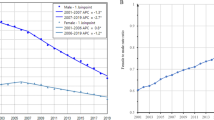
The incidence and mortality of lung cancer in women are rising, with both increasing by 124% between 2003 and 2019. The main risk factor for lung cancer is tobacco use, but indoor radon gas exposure is one of the leading causes in nonsmokers. The most recent evidence demonstrates that multiple factors can make women more susceptible to harm from these risk factors or carcinogens. For this consensus statement, the Association for Lung Cancer Research in Women (ICAPEM) invited a group of lung cancer experts to perform a detailed gender-based analysis of lung cancer. Clinically, female patients have different lung cancer profiles, and most actionable driver alterations are more prevalent in women, particularly in never-smokers. Additionally, the impact of certain therapies seems to be different. In the future, it will be necessary to carry out specific studies to improve the understanding of the role of certain biomarkers and gender in the prognosis and evolution of lung cancer.



Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21654.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
(REDECAN) REdRdC. Estimaciones de la incidencia del cáncer en España, 20212021.
Estadística INd. Defunciones según la causa de muerte 2018.
Ruano-Ravina A, Provencio M, Calvo-de-Juan V, Carcereny E, Estival A, Rodríguez-Abreu D, et al. Are there differences by sex in lung cancer characteristics at diagnosis? A nationwide study. Transl Lung Cancer Res. 2021;10(10):3902–11. https://doi.org/10.21037/tlcr-21-559.
Remon J, Reguart N, García-Campelo R, Conde E, Lucena CM, Persiva O, et al. Lung cancer in Spain. J Thorac Oncol. 2021;16(2):197–204. https://doi.org/10.1016/j.jtho.2020.09.026.
Isla D, Majem M, Vinolas N, Artal A, Blasco A, Felip E, et al. A consensus statement on the gender perspective in lung cancer. Clin Transl Oncol. 2017;19(5):527–35. https://doi.org/10.1007/s12094-016-1578-x.
Health NCfCDPaHPUOoSa. The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta: Centers for Disease Control and Prevention; 2014.
Rey J, Pérez-Ríos M, Santiago-Pérez MI, Galán I, Schiaffino A, Varela-Lema L, et al. Smoking-attributable mortality in the autonomous communities of Spain, 2017. Rev Esp Cardiol (Engl Ed). 2021. https://doi.org/10.1016/j.rec.2020.10.023.
Organization WH. WHO handbook on indoor radon: a public health perspective. Geneva: Switzerland; 2009.
Ruano-Ravina A, Varela-Lema L, García-Talavera M, García-Gómez M, González-Muñoz S, Santiago-Pérez MI, et al. Lung cancer mortality attributable to residential radon exposure in Spain and its regions. Environ Res. 2021;199:111372. https://doi.org/10.1016/j.envres.2021.111372.
Lorenzo-González M, Ruano-Ravina A, Torres-Durán M, Kelsey KT, Provencio M, Parente-Lamelas I, et al. Lung cancer and residential radon in never-smokers: a pooling study in the Northwest of Spain. Environ Res. 2019;172:713–8. https://doi.org/10.1016/j.envres.2019.03.011.
Lorenzo-Gonzalez M, Ruano-Ravina A, Torres-Duran M, Kelsey KT, Provencio M, Parente-Lamelas I, et al. Lung cancer risk and residential radon exposure: a pooling of case-control studies in northwestern Spain. Environ Res. 2020;189:109968. https://doi.org/10.1016/j.envres.2020.109968.
Lorenzo-González M, Ruano-Ravina A, Torres-Durán M, Provencio-Pulla M, Kelsey K, Parente-Lamelas I, et al. Lung cancer risk and do-it-yourself activities. A neglected risk factor for lung cancer. Environ Res. 2019;179(Pt B):108812. https://doi.org/10.1016/j.envres.2019.108812.
Barrera-Rodriguez R, Morales-Fuentes J. Lung cancer in women. Lung Cancer (Auckl). 2012;3:79–89. https://doi.org/10.2147/lctt.S37319.
Li T, Kung HJ, Mack PC, Gandara DR. Genotyping and genomic profiling of non-small-cell lung cancer: implications for current and future therapies. J Clin Oncol. 2013;31(8):1039–49. https://doi.org/10.1200/jco.2012.45.3753.
Tsao AS, Scagliotti GV, Bunn PA Jr, Carbone DP, Warren GW, Bai C, et al. Scientific advances in lung cancer 2015. J Thorac Oncol. 2016;11(5):613–38. https://doi.org/10.1016/j.jtho.2016.03.012.
Jamal-Hanjani M, Wilson GA, McGranahan N, Birkbak NJ, Watkins TBK, Veeriah S, et al. Tracking the evolution of non-small-cell lung cancer. N Engl J Med. 2017;376(22):2109–21. https://doi.org/10.1056/NEJMoa1616288.
Sanchez-Vega F, Mina M, Armenia J, Chatila WK, Luna A, La KC, et al. Oncogenic signaling pathways in the cancer genome atlas. Cell. 2018;173(2):321-37.e10. https://doi.org/10.1016/j.cell.2018.03.035.
Mederos N, Friedlaender A, Peters S, Addeo A. Gender-specific aspects of epidemiology, molecular genetics and outcome: lung cancer. ESMO Open. 2020;5(Suppl 4):e000796. https://doi.org/10.1136/esmoopen-2020-000796.
Pikor LA, Ramnarine VR, Lam S, Lam WL. Genetic alterations defining NSCLC subtypes and their therapeutic implications. Lung Cancer. 2013;82(2):179–89. https://doi.org/10.1016/j.lungcan.2013.07.025.
Marin E, Teixido C, Carmona-Rocha E, Reyes R, Arcocha A, Viñolas N, et al. Usefulness of two independent DNA and RNA tissue-based multiplex assays for the routine care of advanced NSCLC patients. Cancers (Basel). 2020. https://doi.org/10.3390/cancers12051124.
Yuan Y, Liu L, Chen H, Wang Y, Xu Y, Mao H, et al. Comprehensive characterization of molecular differences in cancer between male and female patients. Cancer Cell. 2016;29(5):711–22. https://doi.org/10.1016/j.ccell.2016.04.001.
Benusiglio PR, Fallet V, Sanchis-Borja M, Coulet F, Cadranel J. Lung cancer is also a hereditary disease. Eur Respir Rev. 2021. https://doi.org/10.1183/16000617.0045-2021.
Mezquita L, Iurchenko A, Benitez JC, Baz M, Nikolaev S, Planchard D, et al. Abstract 448: High prevalence of pathogenic germline variants in patients with oncogene-driven non-small cell lung cancer. Can Res. 2021;81(13 Supplement):448. https://doi.org/10.1158/1538-7445.AM2021-448.
Mezquita L, Jové M, Nadal E, Kfoury M, Morán T, Ricordel C, et al. High prevalence of somatic oncogenic driver alterations in patients with NSCLC and Li-fraumeni syndrome. J Thorac Oncol. 2020;15(7):1232–9. https://doi.org/10.1016/j.jtho.2020.03.005.
Lincoln SE, Nussbaum RL, Kurian AW, Nielsen SM, Das K, Michalski S, et al. Yield and utility of germline testing following tumor sequencing in patients with cancer. JAMA Netw Open. 2020;3(10):e2019452. https://doi.org/10.1001/jamanetworkopen.2020.19452.
McIllmurray MB, Thomas C, Francis B, Morris S, Soothill K, Al-Hamad A. The psychosocial needs of cancer patients: findings from an observational study. Eur J Cancer Care (Engl). 2001;10(4):261–9. https://doi.org/10.1046/j.1365-2354.2001.00280.x.
Faller H, Koch U, Brähler E, Härter M, Keller M, Schulz H, et al. Satisfaction with information and unmet information needs in men and women with cancer. J Cancer Surviv. 2016;10(1):62–70. https://doi.org/10.1007/s11764-015-0451-1.
Gupta AA, Edelstein K, Albert-Green A, D’Agostino N. Assessing information and service needs of young adults with cancer at a single institution: the importance of information on cancer diagnosis, fertility preservation, diet, and exercise. Support Care Cancer. 2013;21(9):2477–84. https://doi.org/10.1007/s00520-013-1809-4.
Hamilton J, Kruse H, Holcomb L, Freche R. Distress and psychosocial needs: demographic predictors of clinical distress after a diagnosis of cancer. Clin J Oncol Nurs. 2018;22(4):390–7. https://doi.org/10.1188/18.Cjon.390-397.
Leung B, Laskin J, Wu J, Bates A, Ho C. Assessing the psychosocial needs of newly diagnosed patients with nonsmall cell lung cancer: identifying factors associated with distress. Psychooncology. 2019;28(4):815–21. https://doi.org/10.1002/pon.5025.
Gautam S, Poudel A. Effect of gender on psychosocial adjustment of colorectal cancer survivors with ostomy. J Gastrointest Oncol. 2016;7(6):938–45. https://doi.org/10.21037/jgo.2016.09.02.
Obispo-Portero B, Cruz-Castellanos P, Jiménez-Fonseca P, Rogado J, Hernandez R, Castillo-Trujillo OA, et al. Anxiety and depression in patients with advanced cancer during the COVID-19 pandemic. Support Care Cancer. 2022. https://doi.org/10.1007/s00520-021-06789-3.
Bernacki R, Paladino J, Neville BA, Hutchings M, Kavanagh J, Geerse OP, et al. Effect of the serious illness care program in outpatient oncology: a cluster randomized clinical trial. JAMA Intern Med. 2019;179(6):751–9. https://doi.org/10.1001/jamainternmed.2019.0077.
Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994–2003. https://doi.org/10.1001/jamainternmed.2014.5271.
Bernacki R, Hutchings M, Vick J, Smith G, Paladino J, Lipsitz S, et al. Development of the serious illness care program: a randomised controlled trial of a palliative care communication intervention. BMJ Open. 2015;5(10):e009032. https://doi.org/10.1136/bmjopen-2015-009032.
Paladino J, Kilpatrick L, O’Connor N, Prabhakar R, Kennedy A, Neal BJ, et al. Training clinicians in serious illness communication using a structured guide: evaluation of a training program in three health systems. J Palliat Med. 2020;23(3):337–45. https://doi.org/10.1089/jpm.2019.0334.
Jain N, Bernacki RE. Goals of care conversations in serious illness: a practical guide. Med Clin N Am. 2020;104(3):375–89. https://doi.org/10.1016/j.mcna.2019.12.001.
Paladino J, Koritsanszky L, Nisotel L, Neville BA, Miller K, Sanders J, et al. Patient and clinician experience of a serious illness conversation guide in oncology: a descriptive analysis. Cancer Med. 2020;9(13):4550–60. https://doi.org/10.1002/cam4.3102.
Tam V, You JJ, Bernacki R. Enhancing medical learners’ knowledge of, comfort and confidence in holding serious illness conversations. Am J Hosp Palliat Care. 2019;36(12):1096–104. https://doi.org/10.1177/1049909119857988.
Charatan F. Lung cancer death rates rise 600% in US women. BMJ. 2001;322(7289):752. https://doi.org/10.1136/bmj.322.7289.752.
Remon J, Molina-Montes E, Majem M, Lianes P, Isla D, Garrido P, et al. Lung cancer in women: an overview with special focus on Spanish women. Clin Transl Oncol. 2014;16(6):517–28. https://doi.org/10.1007/s12094-013-1137-7.
Harichand-Herdt S, Ramalingam SS. Gender-associated differences in lung cancer: clinical characteristics and treatment outcomes in women. Semin Oncol. 2009;36(6):572–80. https://doi.org/10.1053/j.seminoncol.2009.10.007.
Fu JB, Kau TY, Severson RK, Kalemkerian GP. Lung cancer in women: analysis of the national surveillance, epidemiology, and end results database. Chest. 2005;127(3):768–77. https://doi.org/10.1378/chest.127.3.768.
Antonoff MB, David EA, Donington JS, Colson YL, Litle VR, Lawton JS, et al. Women in thoracic surgery: 30 years of history. Ann Thorac Surg. 2016;101(1):399–409. https://doi.org/10.1016/j.athoracsur.2015.11.014.
Fibla JJ, Molins L, Quero F, Izquierdo JM, Sánchez D, Hernández J, et al. Perioperative outcome of lung cancer surgery in women: results from a Spanish nationwide prospective cohort study. J Thorac Dis. 2019;11(4):1475–84. https://doi.org/10.21037/jtd.2019.03.30.
Tong BC, Kosinski AS, Burfeind WR Jr, Onaitis MW, Berry MF, Harpole DH Jr, et al. Sex differences in early outcomes after lung cancer resection: analysis of the Society of Thoracic Surgeons General Thoracic Database. J Thorac Cardiovasc Surg. 2014;148(1):13–8. https://doi.org/10.1016/j.jtcvs.2014.03.012.
Eisenstein M. New lung-cancer drugs extend survival times. Nature. 2020;587(7834):S10–2. https://doi.org/10.1038/d41586-020-03154-y.
Drilon A, Oxnard GR, Tan DSW, Loong HHF, Johnson M, Gainor J, et al. Efficacy of selpercatinib in RET fusion-positive non-small-cell lung cancer. N Engl J Med. 2020;383(9):813–24. https://doi.org/10.1056/NEJMoa2005653.
Li BT, Smit EF, Goto Y, Nakagawa K, Udagawa H, Mazières J, et al. Trastuzumab deruxtecan in HER2-mutant non-small-cell lung cancer. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2112431.
Paik PK, Felip E, Veillon R, Sakai H, Cortot AB, Garassino MC, et al. Tepotinib in non-small-cell lung cancer with MET Exon 14 skipping mutations. N Engl J Med. 2020;383(10):931–43. https://doi.org/10.1056/NEJMoa2004407.
Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–38. https://doi.org/10.1056/NEJMoa1704795.
Planchard D, Besse B, Groen HJM, Hashemi SMS, Mazieres J, Kim TM, et al. Phase 2 study of dabrafenib plus trametinib in patients with BRAF V600E-mutant metastatic NSCLC: updated 5-year survival rates and genomic analysis. J Thorac Oncol. 2022;17(1):103–15. https://doi.org/10.1016/j.jtho.2021.08.011.
Shaw AT, Riely GJ, Bang YJ, Kim DW, Camidge DR, Solomon BJ, et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): updated results, including overall survival, from PROFILE 1001. Ann Oncol. 2019;30(7):1121–6. https://doi.org/10.1093/annonc/mdz131.
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25. https://doi.org/10.1056/NEJMoa1713137.
Wolf J, Seto T, Han JY, Reguart N, Garon EB, Groen HJM, et al. Capmatinib in MET Exon 14-mutated or MET-amplified non-small-cell lung cancer. N Engl J Med. 2020;383(10):944–57. https://doi.org/10.1056/NEJMoa2002787.
Drilon A, Moreno V, Patel J, Lassen UN, Solomon B, Rosen L, et al. 1289P Efficacy and safety of larotrectinib in patients with tropomyosin receptor kinase (TRK) fusion lung cancer. Ann Oncol. 2020;31:S834. https://doi.org/10.1016/j.annonc.2020.08.1603.
Drilon A, Paz-Ares L, Doebele RC, Farago AF, Liu SV, Chawla SP, et al. 543P Entrectinib in NTRK fusion-positive NSCLC: updated integrated analysis of STARTRK-2, STARTRK-1 and ALKA-372-001. Ann Oncol. 2020;31:S474–5. https://doi.org/10.1016/j.annonc.2020.08.657.
Skoulidis F, Li BT, Dy GK, Price TJ, Falchook GS, Wolf J, et al. Sotorasib for lung cancers with KRAS p.G12C mutation. N Engl J Med. 2021;384(25):2371–81. https://doi.org/10.1056/NEJMoa2103695.
Nakagawa K, Nagasaka M, Felip E, Pacheco J, Baik C, Goto Y, et al. OA04.05 trastuzumab deruxtecan in HER2-Overexpressing metastatic non-small cell lung cancer: interim results of DESTINY-Lung01. J Thorac Oncol. 2021;16(3):S109–10. https://doi.org/10.1016/j.jtho.2021.01.285.
Devarakonda S, Li Y, Martins Rodrigues F, Sankararaman S, Kadara H, Goparaju C, et al. Genomic profiling of lung adenocarcinoma in never-smokers. J Clin Oncol. 2021;39(33):3747–58. https://doi.org/10.1200/jco.21.01691.
Govindan R, Ding L, Griffith M, Subramanian J, Dees ND, Kanchi KL, et al. Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell. 2012;150(6):1121–34. https://doi.org/10.1016/j.cell.2012.08.024.
Gitlitz BJ, Novello S, Vavalà T, Bittoni M, Sable-Hunt A, Pavlick D, et al. The genomics of young lung cancer: comprehensive tissue genomic analysis in patients under 40 with lung cancer. JTO Clin Res Rep. 2021;2(7):100194. https://doi.org/10.1016/j.jtocrr.2021.100194.
Sacher AG, Dahlberg SE, Heng J, Mach S, Jänne PA, Oxnard GR. Association between younger age and targetable genomic alterations and prognosis in non-small-cell lung cancer. JAMA Oncol. 2016;2(3):313–20. https://doi.org/10.1001/jamaoncol.2015.4482.
Bria E, Milella M, Cuppone F, Novello S, Ceribelli A, Vaccaro V, et al. Outcome of advanced NSCLC patients harboring sensitizing EGFR mutations randomized to EGFR tyrosine kinase inhibitors or chemotherapy as first-line treatment: a meta-analysis. Ann Oncol. 2011;22(10):2277–85. https://doi.org/10.1093/annonc/mdq742.
Freire AC, Basit AW, Choudhary R, Piong CW, Merchant HA. Does sex matter? The influence of gender on gastrointestinal physiology and drug delivery. Int J Pharm. 2011;415(1–2):15–28. https://doi.org/10.1016/j.ijpharm.2011.04.069.
Groenland SL, Geel DR, Janssen JM, de Vries N, Rosing H, Beijnen JH, et al. Exposure-response analyses of anaplastic lymphoma kinase inhibitors crizotinib and alectinib in non-small cell lung cancer patients. Clin Pharmacol Ther. 2021;109(2):394–402. https://doi.org/10.1002/cpt.1989.
Corral J, Mok TS, Nakagawa K, Rosell R, Lee KH, Migliorino MR, et al. Effects of dose modifications on the safety and efficacy of dacomitinib for EGFR mutation-positive non-small-cell lung cancer. Future Oncol. 2019;15(24):2795–805. https://doi.org/10.2217/fon-2019-0299.
Patel SA, Herynk MH, Cascone T, Saigal B, Nilsson MB, Tran H, et al. Estrogen promotes resistance to bevacizumab in murine models of NSCLC. J Thorac Oncol. 2021;16(12):2051–64. https://doi.org/10.1016/j.jtho.2021.07.007.
Wakelee HA, Wang W, Schiller JH, Langer CJ, Sandler AB, Belani CP, et al. Survival differences by sex for patients with advanced non-small cell lung cancer on Eastern Cooperative Oncology Group trial 1594. J Thorac Oncol. 2006;1(5):441–6.
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–50. https://doi.org/10.1056/NEJMoa061884.
Holm B, Mellemgaard A, Skov T, Skov BG. Different impact of excision repair cross-complementation group 1 on survival in male and female patients with inoperable non-small-cell lung cancer treated with carboplatin and gemcitabine. J Clin Oncol. 2009;27(26):4254–9. https://doi.org/10.1200/jco.2008.18.8631.
Nikolos F, Thomas C, Bado I, Gustafsson J. ERβ sensitizes NSCLC to chemotherapy by regulating DNA damage response. Mol Cancer Res. 2018;16(2):233–42. https://doi.org/10.1158/1541-7786.Mcr-17-0201.
Berkel C, Cacan E. Estrogen- and estrogen receptor (ER)-mediated cisplatin chemoresistance in cancer. Life Sci. 2021;286:120029. https://doi.org/10.1016/j.lfs.2021.120029.
Lund-Iversen M, Scott H, Strøm EH, Theiss N, Brustugun OT, Grønberg BH. Expression of estrogen receptor-α and survival in advanced-stage non-small cell lung cancer. Anticancer Res. 2018;38(4):2261–9. https://doi.org/10.21873/anticanres.12470.
Nikolos F, Thomas C, Rajapaksa G, Bado I, Gustafsson J. ERβ regulates NSCLC phenotypes by controlling oncogenic RAS signaling. Mol Cancer Res. 2014;12(6):843–54. https://doi.org/10.1158/1541-7786.Mcr-13-0663.
Rubin JB, Lagas JS, Broestl L, Sponagel J, Rockwell N, Rhee G, et al. Sex differences in cancer mechanisms. Biol Sex Differ. 2020;11(1):17. https://doi.org/10.1186/s13293-020-00291-x.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38. https://doi.org/10.1038/nri.2016.90.
Araujo JM, Rosas G, Belmar-López C, Raez LE, Rolfo CD, Schwarz LJ, et al. Influence of sex in the molecular characteristics and outcomes of malignant tumors. Front Oncol. 2021;11:752918. https://doi.org/10.3389/fonc.2021.752918.
Conforti F, Pala L, Bagnardi V, Viale G, De Pas T, Pagan E, et al. Sex-based heterogeneity in response to lung cancer immunotherapy: a systematic review and meta-analysis. J Natl Cancer Inst. 2019;111(8):772–81. https://doi.org/10.1093/jnci/djz094.
Velez MA, Burns TF, Stabile LP. The estrogen pathway as a modulator of response to immunotherapy. Immunotherapy. 2019;11(13):1161–76. https://doi.org/10.2217/imt-2019-0024.
Conforti F, Pala L, Bagnardi V, De Pas T, Martinetti M, Viale G, et al. Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol. 2018;19(6):737–46. https://doi.org/10.1016/s1470-2045(18)30261-4.
Conforti F, Pala L, Pagan E, Corti C, Bagnardi V, Queirolo P, et al. Sex-based differences in response to anti-PD-1 or PD-L1 treatment in patients with non-small-cell lung cancer expressing high PD-L1 levels. A systematic review and meta-analysis of randomized clinical trials. ESMO Open. 2021;6(5):100251. https://doi.org/10.1016/j.esmoop.2021.100251.
Wallis CJD, Butaney M, Satkunasivam R, Freedland SJ, Patel SP, Hamid O, et al. Association of patient sex with efficacy of immune checkpoint inhibitors and overall survival in advanced cancers: a systematic review and meta-analysis. JAMA Oncol. 2019;5(4):529–36. https://doi.org/10.1001/jamaoncol.2018.5904.
Ye Y, Jing Y, Li L, Mills GB, Diao L, Liu H, et al. Sex-associated molecular differences for cancer immunotherapy. Nat Commun. 2020;11(1):1779. https://doi.org/10.1038/s41467-020-15679-x.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359(6371):91–7. https://doi.org/10.1126/science.aan3706.
Acknowledgements
The authors are grateful for the editorial assistance of Marta Bosch of HealthCo Trials (Madrid, Spain) in the drafting of this manuscript.
Funding
ICAPEM acknowledges the financial support for this project in the form of unrestricted collaboration in the logistics from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly and Company, Janssen, MSD, Novartis, Pfizer, and Roche.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study concept and design. All authors participated in the writing of the first draft of the manuscript, commented on the following draft versions and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
N Viñolas declares no conflict of interest. L Mezquita has not received any funding related to the content of this paper. J Corral has received education grants, provided consultation, attended advisory boards, and/or provided lectures for Amgen, AstraZeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Hoffmann-La Roche, Janssen-Cilag, Merck Sharp & Dohme, Pfizer, Sanofi, and Takeda Pharmaceutical Company. J Corral declares no conflict of interest. M Cobo has received consultancy or advisory roles from AstraZeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli Lilly and Company, Janssen-Cilag, Kyowa, Merck Sharp & Dohme, Novartis, Pfizer, Roche, Sanofi, and Takeda Pharmaceutical Company; has received research funding from Bristol-Myers Squibb; and has made speaking and public presentations on behalf of AstraZeneca, Boehringer-Ingelheim, Roche, Bristol-Myers Squibb, Eli Lilly and Company, Janssen-Cilag, Kyowa, Merck Sharp & Dohme, Novartis, Novocure, Pierre Fabre, Sanofi, and Takeda Pharmaceutical Company. F Gil-Moncayo declares no conflict of interest. L Paz-Ares has not received any funding related to the content of this paper. J Remon has not received any funding related to the content of this paper. M Rodríguez has received consultant fees from Abex and AstraZeneca. She has also received a grant from Intuitive Surgical not related to the current manuscript. A Ruano has not received any funding related to the content of this paper. He has received public funds to conduct research on lung cancer from different competitive grants awarded by the Instituto de Salud Carlos III and other public entities. E Conde has received research funding from Eli Lilly and Company, Roche, and Thermo Fisher Scientific and honoraria, consulting and/or travel support from AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Janssen-Cilag, Merck Sharp & Dohme, Pfizer, Roche, and Takeda Pharmaceutical Company. M Majem has received consultancy or advisory roles from AstraZeneca, Bristol-Myers Squibb, Boehringer-Ingelheim, Helsinn Therapeutics, Janssen Oncology, Merck Sharp & Dohme, Novartis, Pierre Fabre, Pfizer, Roche, Sanofi, and Takeda Pharmaceutical Company; research funding from AstraZeneca, Bristol-Myers Squibb, and Roche; and travel and accommodations expenses from AstraZeneca, Eli Lilly and Company, and Roche. P Garrido has received consultancy or advisory services from AbbVie, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly and Company, GlaxoSmithKline, Janssen-Cilag, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and Takeda Pharmaceutical Company and has made speaking and public presentations on behalf of Amgen, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Janssen-Cilag, Medscape, Merck Sharp & Dohme, Novartis, Pfizer, Roche, Takeda Pharmaceutical Company, and TouchTime. E Felip has received grants or research funding contracts related to Oncology Innovation from Merck Healthcare KGaA and Fundación Merck Salud; consulting fees from Amgen, AstraZeneca, Bayer, BerGenBio, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly and Company, GlaxoSmithKline, Hoffmann-La Roche, Janssen-Cilag, Merck Serono, Merck Sharp & Dohme, Novartis, Peptomyc, Pfizer, Sanofi, and Takeda Pharmaceutical Company; and payment or honoraria for lectures, presentations, speakers bureaus, manuscripts writing or educational events from Amgen, AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Hoffmann-La Roche, Janssen-Cilag, Medical Trends, Medscape, Merck Serono, Merck Sharp & Dohme, PeerVoice, Pfizer, Sanofi, Takeda Pharmaceutical Company, and Touch Oncology. E Felip is an independent member of the board of Grifols. D Isla has not received any funding related to the content of this paper. J de Castro has not received any funding related to the content of this paper.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Viñolas, N., Mezquita, L., Corral, J. et al. The role of sex and gender in the diagnosis and treatment of lung cancer: the 6th ICAPEM Annual Symposium. Clin Transl Oncol 26, 352–362 (2024). https://doi.org/10.1007/s12094-023-03262-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03262-x