Abstract
Introduction
Cancer patients often suffer from malnutrition and early detection and raising awareness of nutritional issues is crucial in this population.
Methods
The Spanish Oncology Society (SEOM) conducted the Quasar_SEOM study to investigate the current impact of the Anorexia–Cachexia Syndrome (ACS). The study employed questionnaires and the Delphi method to gather input from both cancer patients and oncologists on key issues related to early detection and treatment of ACS. A total of 134 patients and 34 medical oncologists were surveyed about their experiences with ACS. The Delphi methodology was used to evaluate oncologists' perspectives of ACS management, ultimately leading to a consensus on the most critical issues.
Results
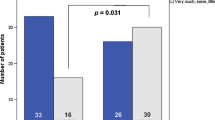
Despite widespread acknowledgement of malnutrition in cancer as a significant issue by 94% of oncologists, the study revealed deficiencies in knowledge and protocol implementation. A mere 65% of physicians reported being trained to identify and treat these patients, with 53% failing to address ACS in a timely manner, 30% not monitoring weight, and 59% not adhering to any clinical guidelines. The lack of experience was identified as the primary hindrance to the use of orexigens in 18% of cases. Furthermore, patients reported concerns and a perception of inadequate attention to malnutrition-related issues from their physicians.
Conclusion
The results of this study point to a gap in the care of this syndrome and a need to improve education and follow-up of cancer patients with anorexia-cachexia.
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy and ethical restrictions but are available from the corresponding author on reasonable request. This is to respect privacy and confidentiality agreements with the study participants while also ensuring that the data can be accessed for legitimate and ethically-approved research purposes. All requests will be reviewed to verify that they are in line with ethical guidelines and the purpose of the study before any data is released.
References
Osler W. The principles and practice of medicine. D. Appleton and Company; 1912.
Tuca A, Jimenez-Fonseca P, Gascón P. Clinical evaluation and optimal management of cancer cachexia. Crit Rev Oncol Hematol. 2013;88:625–36.
Mitch WE, Goldberg AL. Mechanisms of muscle wasting—the role of the ubiquitin–proteasome pathway. N Engl J Med Mass Med Soc. 1996;335:1897–905.
Suzuki H, Asakawa A, Amitani H, Nakamura N, Inui A. Cancer cachexia—pathophysiology and management. J Gastroenterol. 2013;48:574–94.
Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, Barone C, et al. Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget. 2017;8:79884.
Arthur ST, Van Doren BA, Roy D, Noone JM, Zacherle E, Blanchette CM. Cachexia among US cancer patients. J Med Econ. 2016;19:874–80.
Daly L, Dolan R, Power D, Ní Bhuachalla É, Sim W, Fallon M, et al. The relationship between the BMI-adjusted weight loss grading system and quality of life in patients with incurable cancer. J Cachexia Sarcopenia Muscle. 2020;11:160–8.
Martin L, Senesse P, Gioulbasanis I, Antoun S, Bozzetti F, Deans C, et al. Diagnostic criteria for the classification of cancer-associated weight loss. J Clin Oncol. 2015;33:90–9.
Lasheen W, Walsh D. The cancer anorexia–cachexia syndrome: myth or reality? Support Care Cancer. 2010;18:265–72.
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, et al. Prognostic effect of weight loss prior tochemotherapy in cancer patients. Am J Med. 1980;69:491–7.
Roeland EJ, Bohlke K, Baracos VE, Bruera E, Del Fabbro E, Dixon S, et al. Management of cancer cachexia: ASCO guideline. J Clin Oncol. 2020;38:2438–53.
Planas M, Álvarez-Hernández J, León-Sanz M, Celaya-Pérez S, Araujo K, Garcíade LA. Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES® study. Support Care Cancer. 2016;24:429–35.
Chow R, Bruera E, Chiu L, Chow S, Chiu N, Lam H, et al. Enteral and parenteral nutrition in cancer patients: a systematic review and meta-analysis. Ann Palliat Med. 2016;5:30–41.
Hawkins C. Anorexia and anxiety in advanced malignancy: the relative problem. J Hum Nutr Diet. 2000;13:113–7.
Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The memorial symptom assessment scale short form (MSAS-SF) validity and reliability. Cancer Interdiscip Int J Am Cancer Soc. 2000;89:1162–71.
Hopkinson JB, Wright DNM, McDonald JW, Corner JL. The prevalence of concern about weight loss and change in eating habits in people with advanced cancer. J Pain Symptom Manag. 2006;32:322–31.
Tanghe A, Evers G, Paridaens R. Nurses’ assessments of symptom occurrence and symptom distress in chemotherapy patients. Eur J Oncol Nurs. 1998;2:14–26.
Brown JK, Radke KJ. Nutritional assessment, intervention, and evaluation of weight loss in patients with non-small cell lung cancer. Oncol Nurs Forum. 1998;25:547–53.
Strasser F, Binswanger J, Cerny T, Kesselring A. Fighting a losing battle: eating-related distress of men with advanced cancer and their female partners. A mixed-methods study. Palliat Med. 2007;21:129–37.
Amano K, Baracos VE, Hopkinson JB. Integration of palliative, supportive, and nutritional care to alleviate eating-related distress among advanced cancer patients with cachexia and their family members. Crit Rev Oncol Hematol. 2019;143:117–23.
Holden CM. Anorexia in the terminally ill cancer patient: the emotional impact on the patient and the family. Hosp J. 1991;7:73–84.
Jones RV, Hansford J, Fiske J. Death from cancer at home: the carers’ perspective. Br Med J. 1993;306:249–51.
Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manage Sci. 1963;9:458–67.
Jimenez-Fonseca P, Carmona-Bayonas A, Calderon C, Boj JF, Font C, Lecumberri R, et al. FOTROCAN Delphi consensus statement regarding the prevention and treatment of cancer-associated thrombosis in areas of uncertainty and low quality of evidence. Clin Transl Oncol. 2017;19:1–13.
Kirbiyik F, Ozkan E. Knowledge and practices of medical oncologists concerning nutrition therapy: a survey study. Clin Nutr ESPEN. 2018;27:32–7.
Spiro A, Baldwin C, Patterson A, Thomas J, Andreyev HJN. The views and practice of oncologists towards nutritional support in patients receiving chemotherapy. Br J Cancer. 2006;95:431–4.
Muscaritoli M, Fanelli FR, Molfino A. Perspectives of health care professionals on cancer cachexia: results from three global surveys. Ann Oncol. 2016;27:2230–6.
Muscaritoli M, Corsaro E, Molfino A. Awareness of cancer-related malnutrition and its management: analysis of the results from a survey conducted among medical oncologists. Front Oncol. 2021;11:1669.
Caccialanza R, Lobascio F, Cereda E, Aprile G, Farina G, Traclò F, et al. Cancer-related malnutrition management: a survey among Italian Oncology Units and Patients’ Associations. Curr Probl Cancer. 2020;44: 100554.
Paccagnella A, Morello M, Da Mosto MC, Baruffi C, Marcon ML, Gava A, et al. Early nutritional intervention improves treatment tolerance and outcomes in head and neck cancer patients undergoing concurrent chemoradiotherapy. Support Care Cancer. 2010;18:837–45.
Lim YL, Teoh SE, Yaow CYL, Lin DJ, Masuda Y, Han MX, et al. A systematic review and meta-analysis of the clinical use of megestrol acetate for cancer-related anorexia/cachexia. J Clin Med. 2022;11:3756.
Simons J-P, Aaronson NK, Vansteenkiste JF, Ten Velde GP, Muller MJ, Drenth BM, et al. Effects of medroxyprogesterone acetate on appetite, weight, and quality of life in advanced-stage non-hormone-sensitive cancer: a placebo-controlled multicenter study. J Clin Oncol. 1996;14:1077–84.
Oberholzer R, Hopkinson JB, Baumann K, Omlin A, Kaasa S, Fearon KC, et al. Psychosocial effects of cancer cachexia: a systematic literature search and qualitative analysis. J Pain Symptom Manag. 2013;46:77–95.
Arribas L, Hurtós L, Sendrós MJ, Peiró I, Salleras N, Fort E, et al. NUTRISCORE: a new nutritional screening tool for oncological outpatients. Nutrition. 2017;33:297–303.
Ferguson M, Capra S, Bauer J, Banks M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition. 1999;15:458–64.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Muscaritoli M, Molfino A, Scala F, Christoforidi K, Manneh-Vangramberen I, De Lorenzo F. Nutritional and metabolic derangements in Mediterranean cancer patients and survivors: the ECPC 2016 survey. J Cachexia Sarcopenia Muscle. 2019;10:517–25.
Orrevall Y, Tishelman C, Herrington MK, Permert J. The path from oral nutrition to home parenteral nutrition: a qualitative interview study of the experiences of advanced cancer patients and their families. Clin Nutr. 2004;23:1280–7.
Reid J, Mc Kenna HP, Fitzsimons D, Mc Cance TV. An exploration of the experience of cancer cachexia: what patients and their families want from healthcare professionals. Eur J Cancer Care (Engl). 2010;19:682–9.
Del Fabbro E, Jatoi A, Davis M, Fearon K, Di Tomasso J, Vigano A. Health professionals’ attitudes toward the detection and management of cancer-related anorexia-cachexia syndrome, and a proposal for standardized assessment. J Community Support Oncol. 2015;13:181–7.
Sun L, Quan X-Q, Yu S. An epidemiological survey of cachexia in advanced cancer patients and analysis on its diagnostic and treatment status. Nutr Cancer. 2015;67:1056–62.
Loprinzi CL, Michalak JC, Schaid DJ, Mailliard JA, Athmann LM, Goldberg RM, et al. Phase III evaluation of four doses of megestrol acetate as therapy for patients with cancer anorexia and/or cachexia. J Clin Oncol. 1993;11:762–7.
Garcia VR, López‐Briz E, Sanchis RC, Perales JLG, Bort‐Martí S. Megestrol acetate for treatment of anorexia‐cachexia syndrome. Cochrane Database Syst Rev. 2013.
Ruiz-Garcia V, Lopez-Briz E, Carbonell-Sanchis R, Bort-Marti S, Gonzalvez-Perales JL. Megestrol acetate for cachexia–anorexia syndrome. A systematic review. J Cachexia Sarcopenia Muscle. 2018;9(3):444–52.
Acknowledgements
We thank the patients and the medical oncologists for participating and the continuous care group of the SEOM for supporting the study. Medical oncologists: José Andrés Rodríguez, Soledad Cameselle Garcia, Deborah Contreras, Marta Sotelo, Losune Guillén Blanco, Edurne Muruzábal, Laura Fernández, Maitane Ocáriz, Jorge Bartolomé, Lucía Notario, Alba Puente, Javier Bosque Moreno, Esmeralda García Torralba, Diego Iglesias Riera, Rocío Hernández-Pacheco Acosta, María García Obrero, Javier López.
Funding
The external consultant that managed the online platform for the realization of the study was funded by Viatris Pharmaceuticals S.L. The funder had no involvement in data collection, manuscript drafting, review, the decision to publish, or approval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The other authors declare that they have no conflict of interest related to the scope of this study.
Ethics declarations
This study consisted of a survey of expert opinions and no patient data were collected, so no specific independent ethical or research review or informed consent or approval was necessary.
Informed consent
The study presented in this manuscript was conducted in accordance with the Declaration of Helsinki and its later amendments. Ethical approval was obtained from the Institutional Review Board (IRB) of [Institution Name]. Prior to participation in the study, all participants were provided with detailed written and verbal information about the study's purpose, procedures, potential risks and benefits, the voluntary nature of participation, their right to withdraw from the study at any time without consequence, and the measures taken to ensure their privacy and confidentiality. Each participant provided their informed consent in written form before taking part in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Escobar, Y., Ramchandani, A., Salgado, M. et al. What do patients and oncologists think about the evaluation and management of cancer-related anorexia-cachexia? The Quasar_SEOM study. Clin Transl Oncol 25, 3479–3491 (2023). https://doi.org/10.1007/s12094-023-03212-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03212-7