Abstract
Background
Complete resection combined with postoperative radiotherapy is ideal for skull base chordomas. The recent literature suggests that the degree of surgical resection is the most important prognostic factor.
Methods
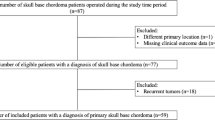
We retrospectively analyzed the clinical data of 16 patients with initial chordoma treated at our center between August 2015 and December 2021 and conducted a retrospective study on the prognosis of surgical treatment of skull base chordoma between 2013 and 2022.
Results
According to the Kaplan–Meier method, there was a significant difference in PFS between patients aged > 50 years and < 50 years, and no significant difference was observed in PFS for tumor involvement of the internal carotid artery, dura, or superior or inferior clivus. However, there was still a correlation with prognosis. As observed in the included literature, the 5-year overall survival rate was significantly higher in patients undergoing total skull base chordoma resection than in those undergoing subtotal resection (STR), which in turn was significantly higher than in those undergoing partial resection (PR). Patients undergoing subtotal resection had significantly better 5-year PFS rates than those undergoing PR.
Conclusion
Our study shows that gross total resection and STR have better survival in patients with skull base chordomas compared to PR.







Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Abbreviations
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- GTR:
-
Gross total resection
- STR:
-
Subtotal resection
- PR:
-
Partial resection
- ICA:
-
Internal carotid artery
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- RCTs:
-
Randomized controlled trials (RCTs)
- MINORS:
-
Methodological Index for Non-Randomized Studies
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- K–M:
-
Kaplan–Meier
References
Bumber Z, Krizanac S, Janjanin S, Bilic M, Bumber B. Extranotochordal extralaryngeal chordoma: a case report. Auris Nasus Larynx. 2009;36(1):116–9. https://doi.org/10.1016/j.anl.2007.12.009.
Azzopardi C, Grech R, Mizzi A. Teaching neuroimages: chordoma. Neurology. 2014;83(10):e110–1. https://doi.org/10.1212/WNL.0000000000000751.
Chibbaro S, Cornelius JF, Froelich S, et al. Endoscopic endonasal approach in the management of skull base chordomas—clinical experience on a large series, technique, outcome, and pitfalls. Neurosurg Rev. 2014;37(2):217–25. https://doi.org/10.1007/s10143-013-0503-9.
Di Maio S, Rostomily R, Sekhar LN. Current surgical outcomes for cranial base chordomas: cohort study of 95 patients. Neurosurgery. 2012;70(6):1355–60. https://doi.org/10.1227/NEU.0b013e3182446783.
Stacchiotti S, Sommer J, Chordoma Global Consensus Group. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 2015;16(2):e71–83. https://doi.org/10.1016/S1470-2045(14)71190-8.
Wang L, Tian K, Wang K, et al. Factors for tumor progression in patients with skull base chordoma. Cancer Med. 2016;5(9):2368–77. https://doi.org/10.1002/cam4.834.
Wu Z, Zhang J, Zhang L, et al. Prognostic factors for long-term outcome of patients with surgical resection of skull base chordomas—106 cases review in one institution. Neurosurg Rev. 2010;33(4):451–6. https://doi.org/10.1007/s10143-010-0273-6.
Zou MX, Lv GH, Zhang QS, Wang SF, Li J, Wang XB. Prognostic factors in skull base chordoma: a systematic literature review and meta-analysis. World Neurosurg. 2018;109:307–27. https://doi.org/10.1016/j.wneu.2017.10.010.
George B, Bresson D, Herman P, Froelich S. Chordomas: a review. Neurosurg Clin N Am. 2015;26(3):437–52. https://doi.org/10.1016/j.nec.2015.03.012.
Bai J, Li M, Shi J, et al. Mid-term follow-up surgical results in 284 cases of clival chordomas: the risk factors for outcome and tumor recurrence. Neurosurg Rev. 2022;45(2):1451–62. https://doi.org/10.1007/s10143-021-01576-4.
Ouyang T, Zhang N, Zhang Y, et al. Clinical characteristics, immunohistochemistry, and outcomes of 77 patients with skull base chordomas. World Neurosurg. 2014;81(5–6):790–7. https://doi.org/10.1016/j.wneu.2013.01.010.
Ahmed R, Sheybani A, Menezes AH, Buatti JM, Hitchon PW. Disease outcomes for skull base and spinal chordomas: a single center experience. Clin Neurol Neurosurg. 2015;130:67–73. https://doi.org/10.1016/j.clineuro.2014.12.015.
Gui S, Zong X, Wang X, et al. Classification and surgical approaches for transnasal endoscopic skull base chordoma resection: a 6-year experience with 161 cases. Neurosurg Rev. 2016;39(2):321–33. https://doi.org/10.1007/s10143-015-0696-1.
Pattankar S, Warade A, Misra BK, Deshpande RB. Long-term outcome of adjunctive Gamma Knife radiosurgery in skull-base chordomas and chondrosarcomas: an Indian experience. J Clin Neurosci. 2022;96:90–100. https://doi.org/10.1016/j.jocn.2021.12.018.
Rahme RJ, Arnaout OM, Sanusi OR, Kesavabhotla K, Chandler JP. Endoscopic approach to clival chordomas: the northwestern experience. World Neurosurg. 2018;110:e231–8. https://doi.org/10.1016/j.wneu.2017.10.146.
Roy A, Warade A, Jha AK, Misra BK. Skull base chordoma: long-term observation and evaluation of prognostic factors after surgical resection. Neurol India. 2021;69(6):1608–12. https://doi.org/10.4103/0028-3886.333474.
Zhang HK, Sun XC, Hu L, Wang JJ, Wang DH. Endonasal endoscopic resection and radiotherapy in skull base chordomas. J Craniofac Surg. 2016;27(7):e709–13. https://doi.org/10.1097/SCS.0000000000003031.
Sanusi O, Arnaout O, Rahme RJ, Horbinski C, Chandler JP. Surgical resection and adjuvant radiation therapy in the treatment of skull base chordomas. World Neurosurg. 2018;115:e13–21. https://doi.org/10.1016/j.wneu.2018.02.127.
Kim JW, Suh CO, Hong CK, et al. Maximum surgical resection and adjuvant intensity-modulated radiotherapy with simultaneous integrated boost for skull base chordoma. Acta Neurochir. 2017;159(10):1825–34. https://doi.org/10.1007/s00701-016-2909-y.
Wang L, Wu Z, Tian K, et al. Clinical features and surgical outcomes of patients with skull base chordoma: a retrospective analysis of 238 patients. J Neurosurg. 2017;127(6):1257–67. https://doi.org/10.3171/2016.9.JNS16559.
Li H, Zhang H, Hu L, Wang H, Wang D. Endoscopic endonasal resection and radiotherapy as treatment for skull base chordomas. Acta Otolaryngol. 2020;140(9):789–94. https://doi.org/10.1080/00016489.2020.1748225.
Yaniv D, Soudry E, Strenov Y, Cohen MA, Mizrachi A. Skull base chordomas review of current treatment paradigms. World J Otorhinolaryngol Head Neck Surg. 2020;6(2):125–31. https://doi.org/10.1016/j.wjorl.2020.01.008.
Williams BJ, Raper DM, Godbout E, et al. Diagnosis and treatment of chordoma. J Natl Compr Canc Netw. 2013;11(6): 726731. https://doi.org/10.6004/jnccn.2013.0089.
Fernandez-Miranda JC, Gardner PA, Snyderman CH, et al. Clival chordomas: a pathological, surgical, and radiotherapeutic review. Head Neck. 2014;36(6):892–906. https://doi.org/10.1002/hed.23415.
Fagundes MA, Hug EB, Liebsch NJ, Daly W, Efird J, Munzenrider JE. Radiation therapy for chordomas of the base of skull and cervical spine: patterns of failure and outcome after relapse. Int J Radiat Oncol Biol Phys. 1995;33(3):579–84. https://doi.org/10.1016/0360-3016(95)02014-3.
La Corte E, Broggi M, Bosio L, Danesi G, Ferroli P. Tailored surgical strategy in clival chordomas: an extraordinary selection bias that limits approach comparison. J Neurosurg Sci. 2018;62(4):519–21. https://doi.org/10.23736/S0390-5616.17.03986-8.
Campbell RG, Prevedello DM, Ditzel Filho L, Otto BA, Carrau RL. Contemporary management of clival chordomas. Curr Opin Otolaryngol Head Neck Surg. 2015;23(2):153–61. https://doi.org/10.1097/MOO.0000000000000140.
Zhou J, Yang B, Wang X, Jing Z. Comparison of the effectiveness of radiotherapy with photons and particles for chordoma after surgery: a meta-analysis. World Neurosurg. 2018;117:46–53. https://doi.org/10.1016/j.wneu.2018.05.209.
Acknowledgements
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
This Research was funded by the National Natural Science Foundation of China (82171118).
Author information
Authors and Affiliations
Contributions
WJ, YaW, ZP, and YuW conceived and designed the study. YaW, ZP, and YuW performed the analysis, HZ and RF prepared the figures and tables, YaW wrote the main manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
Ethical review and approval were waived for this study due to studies in the article are not involved humans or animals.
Informed consent
Written informed consent has been obtained from the patients to publish this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Peng, Z., Wang, Y. et al. The prognostic significance of different degrees of resection of skull base chordoma. Clin Transl Oncol 24, 2441–2452 (2022). https://doi.org/10.1007/s12094-022-02915-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-02915-7