Abstract
Background
Hepatocellular carcinoma is one of the most common malignancies and leading cancer-associated deaths worldwide. Ozone has been proposed as a promising therapeutic agent in the treatment of various disorders.
Purpose
The purpose of this paper is to assess the potential anticancer effects of the ozone on liver cancer cells.
Method
The liver cancer cell line of bel7402 and SMMC7721 was used in this study. Proliferation was evaluated using the CCK-8 and the colony formation assay. Wond healing assay and transwell assay without Matrigel were used to evaluate their migration ability. Flow cytometry was used for cell cycle analysis and reactive oxygen species (ROS) determination. Glutathione detection kit was used for measurement of glutathione level. Protein expression was estimated by western blot analysis.
Results
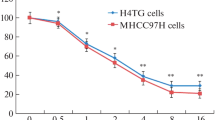
Ozone treatment inhibited liver cancer cell proliferation, colony formation. Ozone induced G2/M phase cell cycle arrest, which could be elucidated by the change of protein levels of p53, p21, Cyclin D1, cyclin B1, cdc2, and CDK4. We also found that ozone treatment inhibited migration ability by inhibiting EMT-relating protein. Ozone also induced ROS accumulation and decreased glutathione level decreased, which contributed to the inactivation of the PI3K/AKT/NF-κB pathway. Finally, we found that pre-treatment of liver cancer cells with N-acetylcysteine resisted ozone-induced effects.
Conclusions
Ozone restrains the proliferation and migration potential and EMT process of liver cancer cells via ROS accumulation and PI3K/AKT/NF-κB suppression.




Similar content being viewed by others
References
Byam J, Renz J, Millis JM. Liver transplantation for hepatocellular carcinoma. Hepatobil Surg Nutr. 2013;2(1):22–30. https://doi.org/10.3978/j.issn.2304-3881.2012.11.03.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Vogel A, Cervantes A, Chau I, Daniele B, Llovet JM, Meyer T, et al. Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(5):871–3. https://doi.org/10.1093/annonc/mdy510.
Buric J, Berjano P, Damilano M. Severe spinal surgery infection and local ozone therapy as complementary treatment: a case report. Int J Spine Surg. 2019;13(4):371–6. https://doi.org/10.14444/6050.
Zeng J, Lu J. Mechanisms of action involved in ozone-therapy in skin diseases. Int Immunopharmacol. 2018;56:235–41. https://doi.org/10.1016/j.intimp.2018.01.040.
Clavo B, Rodríguez-Esparragón F, Rodríguez-Abreu D, Martínez-Sánchez G, Llontop P, Aguiar-Bujanda D, et al. Modulation of oxidative stress by ozone therapy in the prevention and treatment of chemotherapy-induced toxicity: review and prospects. Antioxidants (Basel, Switzerland). 2019;8(12):588. https://doi.org/10.3390/antiox8120588.
Taşdöven İ, Emre AU, Ayça Gültekin F, Öner MÖ, Bakkal BH, Türkcü ÜÖ, et al. Effects of ozone preconditioning on recovery of rat colon anastomosis after preoperative radiotherapy. Adv Clin Exp Med. 2019;28(12):1683–9. https://doi.org/10.17219/acem/110329.
Clavo B, Santana-Rodríguez N, Llontop P, Gutiérrez D, Suárez G, López L, et al. Ozone therapy as adjuvant for cancer treatment: is further research warranted? Evid Based Complement Alternat Med. 2018. https://doi.org/10.1155/2018/7931849.
de Sá Junior PL, Câmara DAD, Porcacchia AS, Fonseca PMM, Jorge SD, Araldi RP, et al. The roles of ROS in cancer heterogeneity and therapy. Oxid Med Cell Longev. 2017. https://doi.org/10.1155/2017/2467940.
Wang N, Wu Y, Bian J, Qian X, Lin H, Sun H, et al. Current development of ROS-modulating agents as novel antitumor therapy. Curr Cancer Drug Tar. 2017;17(2):122–36. https://doi.org/10.2174/1568009616666160216125833.
Dröse S, Brandt U. Molecular mechanisms of superoxide production by the mitochondrial respiratory chain. Adv Exp Med Biol. 2012;748:145–69. https://doi.org/10.1007/978-1-4614-3573-0_6.
Sauer H, Wartenberg M, Hescheler J. Reactive oxygen species as intracellular messengers during cell growth and differentiation. Cell Physiol Biochem. 2001;11(4):173–86. https://doi.org/10.1159/000047804.
Sun SC, Xiao G. Deregulation of NF-kappaB and its upstream kinases in cancer. Cancer Metastasis Rev. 2003;22(4):405–22. https://doi.org/10.1023/a:1023733231406.
Scassellati C, Ciani M, Galoforo AC, Zanardini R, Bonvicini C, Geroldi C. Molecular mechanisms in cognitive frailty: potential therapeutic targets for oxygen-ozone treatment. Mech Ageing Dev. 2020;186:111210. https://doi.org/10.1016/j.mad.2020.111210.
Bocci V, Borrelli E, Travagli V, Zanardi I. The ozone paradox: ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29(4):646–82. https://doi.org/10.1002/med.20150.
Megele R, Riemenschneider MJ, Dodoo-Schittko F, Feyrer M, Kleindienst A. Intra-tumoral treatment with oxygen-ozone in glioblastoma: a systematic literature search and results of a case series. Oncol Lett. 2018;16(5):5813–22. https://doi.org/10.3892/ol.2018.9397.
Teke K, Ozkan TA, Cebeci OO, Yilmaz H, Keles ME, Ozkan L, et al. Preventive effect of intravesical ozone supplementation on n-methyl-n-nitrosourea-induced non-muscle invasive bladder cancer in male rats. Exp Anim Tokyo. 2017;66(3):191–8. https://doi.org/10.1538/expanim.16-0093.
Simonetti V, Quagliariello V, Franzini M, Iaffaioli RV, Maurea N, Valdenassi L. Ozone exerts cytoprotective and anti-inflammatory effects in cardiomyocytes and skin fibroblasts after incubation with doxorubicin. Evid Based Complement Altern Med. 2019. https://doi.org/10.1155/2019/2169103.
Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov. 2009;8(7):579–91. https://doi.org/10.1038/nrd2803.
Chiu J, Dawes IW. Redox control of cell proliferation. Trends Cell Biol. 2012;22(11):592–601. https://doi.org/10.1016/j.tcb.2012.08.002.
Liu Y, Fan D. Ginsenoside Rg5 induces G2/M phase arrest, apoptosis and autophagy via regulating ROS-mediated MAPK pathways against human gastric cancer. Biochem Pharmacol. 2019;168:285–304. https://doi.org/10.1016/j.bcp.2019.07.008.
Kosmider B, Loader JE, Murphy RC, Mason RJ. Apoptosis induced by ozone and oxysterols in human alveolar epithelial cells. Free Radical Biol Med. 2010;48(11):1513–24. https://doi.org/10.1016/j.freeradbiomed.2010.02.032.
Selivanova G. Wild type p53 reactivation: from lab bench to clinic. Febs Lett. 2014;588(16):2628–38. https://doi.org/10.1016/j.febslet.2014.03.049.
Cj S, Jm R. Living with or without cyclins and cyclin-dependent kinases. Gene Dev. 2004;18(22):2699–711. https://doi.org/10.1101/gad.1256504.
Hydbring P, Malumbres M, Sicinski P. Non-canonical functions of cell cycle cyclins and cyclin-dependent kinases. Nat Rev Mol Cell Biol. 2016;17(5):280–92. https://doi.org/10.1038/nrm.2016.27.
Ge P, Ji X, Ding Y, Wang X, Fu S, Meng F, et al. Celastrol causes apoptosis and cell cycle arrest in rat glioma cells. Neurol Res. 2010;32(1):94–100. https://doi.org/10.1179/016164109X12518779082273.
Ning N, Liu S, Liu X, Tian Z, Jiang Y, Yu N, et al. Curcumol inhibits the proliferation and metastasis of melanoma via the miR-152-3p/PI3K/AKT and ERK/NF-κB signaling pathways. J Cancer. 2020;11(7):1679–92. https://doi.org/10.7150/jca.38624.
DiDonato JA, Mercurio F, Karin M. NF-κB and the link between inflammation and cancer. Immunol Rev. 2012;246(1):379–400. https://doi.org/10.1111/j.1600-065X.2012.01099.x.
Park MH, Hong J. Roles of NF-κB in cancer and inflammatory diseases and their therapeutic approaches. Cells-Basel. 2016;5(2):15. https://doi.org/10.3390/cells5020015.
Markopoulos G, Roupakia E, Tokamani M, Alabasi G, Sandaltzopoulos R, Marcu K, et al. Roles of NF-κB signaling in the regulation of miRNAs impacting on inflammation in cancer. Biomedicines. 2018;6(2):40. https://doi.org/10.3390/biomedicines6020040.
Chen S, Sun KX, Feng MX, Sang XB, Liu BL, Zhao Y. Role of glycogen synthase kinase-3β inhibitor AZD1080 in ovarian cancer. Drug Design Dev Ther. 2016;10:1225–32. https://doi.org/10.2147/DDDT.S102506.
Gedaly R, Galuppo R, Daily MF, Shah M, Maynard E, Chen C, et al. Targeting the Wnt/β-catenin signaling pathway in liver cancer stem cells and hepatocellular carcinoma cell lines with FH535. PLoS ONE. 2014;9(6):e99272. https://doi.org/10.1371/journal.pone.0099272.
Tokés AM, Kulka J, Paku S, Szik A, Páska C, Novák PK, et al. Claudin-1, -3 and -4 proteins and mRNA expression in benign and malignant breast lesions: a research study. Breast Cancer Res. 2005;7(2):R296–305. https://doi.org/10.1186/bcr983.
Strouhalova K, Přechová M, Gandalovičová A, Brábek J, Gregor M, Rosel D. Vimentin intermediate filaments as potential target for cancer treatment. Cancers. 2020;12(1):184. https://doi.org/10.3390/cancers12010184.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interest.
Ethical approval
This study did not involve human participants and animals.
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Zeng, T., Tang, S. et al. Medical ozone induces proliferation and migration inhibition through ROS accumulation and PI3K/AKT/NF-κB suppression in human liver cancer cells in vitro. Clin Transl Oncol 23, 1847–1856 (2021). https://doi.org/10.1007/s12094-021-02594-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02594-w