Abstract
Background
Surgery is becoming more practical and effective than conservative treatment in improving the poor outcomes of patients with breast cancer liver metastasis (BCLM). However, there is no generally acknowledged set of standards for identifying BCLM candidates who will benefit from surgery.
Methods
Between January 2011 and September 2018, 67 female BCLM patients who underwent partial hepatectomy were selected for analysis in the present study. Prognostic factors after hepatectomy were determined. Univariate and multivariate analyses were performed to identify predictors of overall survival (OS) and intrahepatic recurrence-free survival (IHRFS).
Results
The 1-, 3- and 5-year OS of patients treated with surgery was 93.5%, 73.7% and 32.2%, respectively, with a median survival time of 57.59 months. The Pringle manoeuvre [hazard radio (HR) = 0.117, 95% CI0.015–0.942, p = 0.044] and an increased interval between breast surgery and BCLM diagnosis (HR0.178, 95% CI 0.037–0.869, p = 0.033) independently predicted improved overall survival for BCLM patients. The 1-, 2- and 3-year IHRFS of patients who underwent surgery was 62.8, 32.6% and 10.9%, respectively, with a median intrahepatic recurrence-free survival time of 13.47 months. Moderately differentiated tumours (HR 0.259, 95% CI 0.078–0.857, p = 0.027) and the development of liver metastasis more than 2 years after breast surgery (HR 0.270, 95% CI 0.108–0.675, p = 0.005) might be predictors of increased IHRFS.
Conclusions
An interval of more than 2 years between breast cancer surgery and liver metastasis seems to be an indication of liver surgery in BCLM patients. The Pringle manoeuvre and moderately differentiated tumours are potential predictors associated with OS and IHRFS, respectively, as benefits from liver resection. Studies with increased sample sizes are warranted to validate our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the largest contributor to mortality from malignant disease among women worldwide[1]. It is estimated that approximately 2.1 million female breast cancer cases were newly diagnosed in 2018[2]. Approximately, 25–40% of breast cancers are reported to have remote metastasis, 5% of which are classified as advanced disease at the time of initial diagnosis, leading to poor overall survival[3]. The liver is the third most common distant metastatic site after bone and lung, accounting for 7.3% of all breast cancer metastases[4]. If untreated, patients with breast cancer and liver metastasis (BCLM) have a median survival time of only 4–8 months. Despite significant achievements in systemic treatment, such as chemotherapy, antiangiogenic treatment and targeted therapy (e.g. anti-hormonal therapy for patients with luminal breast cancer and Herceptin for HER-2-positive patients), the prognosis of BCLM treated with systemic methods is still poor, with a median survival time of only 25 months[5].
Considering the poor results achieved by systemic treatment, other types of effective treatment such as surgery are urgently needed. Surgery for stage IV carcinomas such as colorectal liver metastasis has been demonstrated to be a potentially curative treatment[6], but there is no widely accepted consensus on surgical treatment for BCLM. The 4th ESO–ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 4) state that local therapy should be proposed only in very selected cases of good performance status, with limited liver involvement, no extrahepatic lesions, and demonstrated control of the disease after adequate systemic therapy[7], while the NCCN Guidelines do not mention liver resection as an option for BCLM[8]. Criteria for selecting the appropriate surgery candidates for BCLM still need to be defined.
Because isolated liver metastasis is relatively rare in breast cancer, occurring in approximately 10% of BCLM cases, the role of surgery remains controversial, and local treatment for BCLM is rarely proposed[5]. Although no randomized controlled trials have performed to confirm whether BCLM might benefit from resection of limited metastatic disease, prolonged survival was observed and reported in highly selected patients by several retrospective studies[9,10,11,12,13,14,15]. However, because of the diverse results and limited sample sizes of these studies, there is still no consensus on the selection of BCLM patients who may benefit from liver resection. Moreover, few studies have been performed with patients from Asia. With patients derived from multiple centres, this study aimed to provide further evidence to explore which patients will benefit from surgery.
Patients and methods
Study population and ethics
Between January 2011 and September 2018, we included consecutive female patients with pathologically confirmed BCLM who underwent partial radical hepatectomy at Fudan University Shanghai Cancer Center, Zhongshan Hospital or Eastern Hepatobiliary Surgery Hospital. The patients were derived from our retrospectively maintained institutional database, and each medical record was reviewed by two investigators independently to update clinical and pathological data. Before surgery, all patients signed informed consent to have their clinical information used for research purposes. The present study was approved by the Institutional Ethics Review Board of each centre.
Preoperative workup
We retrieved demographic information, tumour-specific variables, clinical outcomes, and imaging characteristics for review. All of these patients were discussed by a multidisciplinary team (MDT) and considered to be suitable for hepatectomy. Patients who met the following criteria received hepatectomy: (1) good general condition and enough liver function (Child–Pugh Score level A), (2) resectable liver metastasis and (3) no extrahepatic metastases or extrahepatic metastasis has been stabilized using radiotherapy or local resection. Hormone receptor positivity was defined as ER (estrogen receptor) and/or PR (progesterone receptor) positivity. HER2-positive results were defined as IHC ≥ 3 + or FISH-based HER2 gene amplification.
Hepatic resection
Liver resection was performed according to the standard guidelines, with the aim of achieving R0 resection using a liver-sparing technique involving an ultrasonic scalpel and bipolar coagulation. Intra-operative ultrasound was carried out to define foci missed by the imaging data. The major hepatic resections were defined as those in which 3 or more Couinaud segments were removed[16, 17]. Intermittent selective vascular clamping or the Pringle manoeuvre was used, if necessary, to control intra-operative blood loss. Resected tumours were sent to the pathology department for further examination.
Postoperative outcome and follow-up
Postoperative mortality was defined as death within the first 30 days after surgery. Postoperative complication scoring was evaluated according to the Clavien–Dindo classification of surgical complications. Severe complications were defined as those ≥ grade III. Routine laboratory tests, tumour markers, and imaging evaluations (CT scan and/or MRI) were conducted one month after surgery and every 3 months thereafter.
Statistical analyses
Statistical analyses were performed using the IBM SPSS 22.0 software. Overall survival (OS) time was defined as the time between liver surgery and death, while intrahepatic recurrence-free survival (IHRFS) time was defined as the time between liver surgery and recurrence in the liver. Kaplan–Meier analysis and the Cox proportional hazards regression model were used to perform survival analysis. Multivariate analysis was performed to adjust the influence of clinical factors on outcome using the Cox model. A two-tailed p value less than 0.05 was considered statistically significant.
Results
The demographic characteristics and clinical features of the patients are shown in Table 1. A total of 73 female patients who underwent hepatic resection for BCLM between January 2011 and September 2018 were initially selected according to our defined criterion. Due to the missing information on OS (n = 6) and IHRFS (n = 16), a total of 67 and 57 patients were finally included for OS and IHRFS analysis, respectively. Only one patient had synchronous liver metastasis of breast cancer. None of the patients died within 30 days or 90 days after the surgery, and no in-hospital deaths occurred.
Overall survival after hepatic resection
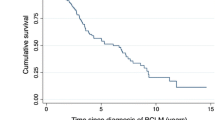
Factors associated with OS by univariate and multivariate Cox analyses are listed in Table 2. The 1-, 3- and 5-year OS for BCLM patients treated with surgery was 93.5%, 73.7% and 32.2%, with a median survival time of 57.59 months (Fig. 1a). Patients with hormone receptor-positive primary tumours had a median OS of 57.59 months, while patients with primary tumours negative for both ER and PR had a median OS of only 35.15 months (p = 0.001, Fig. 1b). Compared with a longer interval ( > 2 years), a shorter interval (≦2 years) between the breast surgery and diagnosis of BCLM was associated with poor OS (for interval ≦2 vs. > 2 years, median OS = 42.81 vs. 57.59 months, p = 0.017, Fig. 1c). Furthermore, patients who received the Pringle manoeuvre during surgery had a longer OS than those who did not, with a median OS increase from 42.81 to 57.59 months (p = 0.016, Fig. 1d).
Multivariate analysis showed a significant trend towards better survival for patients with > 2-year intervals between breast surgery and BCLM diagnosis [hazard ratio (HR) 0.178; 95% CI 0.037–0.869, p = 0.033], which was consistent with the Kaplan–Meier analysis. In line with Kaplan–Meier analysis, hepatic portal triad clamping during surgery was an independent predictor for decreased death risk for BCLM patients (HR 0.117; 95% CI 0.015–0.942, p = 0.044). Multivariate analysis was completed with a Cox proportional hazards model with adjustment for cirrhosis status, steatohepatitis status, age at liver metastasis diagnosis, tumour distribution, extrahepatic metastasis and status of axillary lymph nodes.
Intrahepatic recurrence-free survival after hepatic resection
Factors associated with IHRFS by univariate and multivariate Cox analyses are listed in Table 3. The 1-, 2- and 3-year IHRFS for BCLM patients treated with surgery was 62.8%, 32.6% and 10.9%, respectively, with median IHRFS time of 13.47 months (Fig. 2a). The median IHRFS was 7.20 versus 13.50 months in the comparison of laparoscopic liver resection versus open surgery group (p = 0.045, Fig. 2b). Similar to the OS analysis, the interval between breast surgery and liver metastasis diagnosis was also predictive of IHRFS, with 7.20 months versus 20.83 months in the comparison of BCLM patients with ≦2-year intervals versus those with > 2-year intervals (p = 0.032, Fig. 2c). We also concluded that BCLM patients with moderately differentiated tumours tended to have better IHRFS than those with poorly differentiated tumours (20.83 versus 8.97 months, p = 0.040, Fig. 2d), as indicated by the Kaplan–Meier analysis.
a Intrahepatic recurrence-free survival of all patients from the time of hepatic resection. b Intrahepatic recurrence-free survival based on the type of surgical approach (open or laparoscopic). c Intrahepatic recurrence-free survival based on the interval between breast surgery and liver metastasis diagnosis. d Intrahepatic recurrence-free survival based on tumour differentiation
Multivariate Cox analysis showed that a longer interval ( > 2 years) between the breast surgery and diagnosis of BCLM was associated with a decreased recurrence risk (HR 0.270; 95% CI 0.108–0.675, p = 0.005). Interestingly, multivariate Cox analysis indicated that moderately differentiated tumours were associated with decreased recurrence risk (HR 0.259, 95% CI 0.078–0.857, p = 0.027) after liver resection. BCLM patients with open surgery had a boundary trend towards decreased recurrence risk (HR 0.410, 95% CI 0.167–1.009, p = 0.052) when compared with laparoscopic surgery, but the results with borderline significance need to be validated in an increased sample size.
Discussion
Metastatic breast cancer is characterized by a systemic disease with a poor prognosis. Traditionally, surgery was considered to have limited utility in the treatment of these patients[18]. Although advanced achievement was acquired in systemic treatment (e.g. chemotherapy, hormonal therapy, and biological therapy), the survival of breast cancer patients with liver metastasis remains poor[19]. Considering the poor results achieved by systemic treatment, other types of effective treatment such as surgery need to be identified. Given the lack of consensus on liver resection for BCLM patients to date, our retrospective multicentre analysis might provide useful evidence for clinical decisions. Moreover, consistent with previous investigations[9], our data demonstrated that the 5-year OS for the BCLM patient cohort was as high as 32.2%, with a median survival time of 57.59 months, indicating that surgery was an effective way to improve prognosis for selected patients. Beyond primary sites, distant liver metastasis also presented substantial heterogeneity. Therefore, it is crucial to verify the features of suitable candidates for surgery.
Several studies have been performed on this topic, but the results are inconsistent to some extent. Hoffmann et al.[11] discovered that patients who developed liver metastases within the first 12 months had a shorter OS than those who suffered metastasis disease within a longer interval, while Caralt et al.[10] and Pocard et al.[20] noted that a 2-year interval from diagnosis to liver metastasis was the optimal cutoff discriminating the outcome of the patients well. Meanwhile, Selzner et al.[21] and Treska et al.[22] found that a disease-free interval between the treatment of the breast tumour and the diagnosis of liver metastasis shorter than 1 year or 4 years was a negative independent predictor of both OS and IHRFS, respectively. Our results showed that a relatively long interval ( > 2 years) between breast surgery and liver metastases was a predictor of both OS and IHRFS benefits from liver surgery, which was consistent with previous studies. The interval between breast surgery and liver metastases might be a reflection of the metastatic ability of primary tumours, leading to varied IHRFS and OS after liver resection, as indicated by our data. Another important factor affecting the results of surgical treatment of BCLMs is hormone receptor status. Abbott et al.[13], Treska et al.[23], and Kostov et al.[24] noticed relatively poor results in patients whose tumours were both ER and PR negative, but others, such as Adam et al.[9], reported no role of hormone receptor status in predicting postoperative outcomes. In our study, the association of both ER- negative status and PR-negative status in the primary tumour with poor OS were observed only in univariate analysis and were not significant after adjustment for other clinical factors.
It is worth noting that we identified something no previous work has examined: the use of the Pringle manoeuvre increased the survival substantially and laparoscopic procedure could decrease the IHRFS. The Pringle manoeuvre, introduced to help control bleeding during hepatectomy[25, 26], may cause hypoxia in liver tissues but reduces haemorrhage enormously. Our results indicated that patients who received the Pringle manoeuvre during surgery had a longer OS, with a median OS increase from 42.81 to 57.59 months, compared with those without this procedure. The Pringle manoeuvre could simplify the procedure of liver resection, shorten operation time and, most importantly, minimize intra-operative bleeding, allowing the surgeon to remove metastatic lesions with the lowest possible risk of postoperative complications. Moreover, we found no difference in OS between laparoscopic and open surgery. Laparoscopic liver resections are safe and show more favourable outcomes than open liver surgery in selected patients[27], and in our centre, laparoscopic surgery accounted for more than 40% of cases. However, in BCLM patients, especially those with multiple metastases, it is crucial to explore the whole liver during surgery to ensure that no metastasis lesions have been missed. As a result, the more thorough inspection permitted by open surgery might be a reason for the lower recurrence risk in BCLM patients who received hepatectomy. Poorly differentiated malignancies were supposed to have a worse prognosis than well- and moderately differentiated malignancies. There were no well-differentiated tumours among the samples, and we found that patients with moderately differentiated tumours tended to have later recurrence than those with poorly differentiated tumours, while no significant difference was observed in OS between the two groups. It is reasonable to believe that poorly differentiated BCLMs were inclined to relapse early due to the high degree of malignancy. However, in the long run, it did not affect the OS, which means that further efforts will be necessary to investigate the nature of the benefit.
This study has some shortcomings: First, the missing data on IHRFS and OS decreased the sample size and the statistical power in survival analysis; second, the missing information on other clinical variables may limit the clinical applicability of the results; third, bias may have been introduced by the retrospective design of the present study.
Conclusion
Hepatectomy may lead to an improved outcome for a certain type of BCLM patient. Patients with a longer interval ( > 2 years) between breast surgery and diagnosis of BCLM seem to be more suitable for surgery. Moderately differentiated tumours were also a predictor of benefit from surgery in terms of prolonged OS and PFS. Hepatic portal triad clamping, if necessary, is recommended to improve the outcome of BCLM patients. Because of the limitations of the present study, studies with increased sample sizes and prospective design are needed to further validate our results.
References
DeSantis C, Ma J, Bryan L. Jemal A (2014) Breast cancer statistics. CA A Cancer J Clin. 2013;64(1):52–62. https://doi.org/10.3322/caac.21203.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2018. https://doi.org/10.3322/caac.21492.
Guarneri V, Conte P. Metastatic breast cancer: therapeutic options according to molecular subtypes and prior adjuvant therapy. Oncologist. 2009;14(7):645–56. https://doi.org/10.1634/theoncologist.2009-0078.
Berman AT, Thukral AD, Hwang WT, Solin LJ, Vapiwala N. Incidence and patterns of distant metastases for patients with early-stage breast cancer after breast conservation treatment. Clinical breast cancer. 2013;13(2):88–94. https://doi.org/10.1016/j.clbc.2012.11.001.
Zinser JW, Hortobagyi GN, Buzdar AU, Smith TL, Fraschini G. Clinical course of breast cancer patients with liver metastases. J Clin Oncol. 1987;5(5):773–82.
Adam R, De Gramont A, Figueras J, Guthrie A, Kokudo N, Kunstlinger F, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist. 2012;17(10):1225–399. https://doi.org/10.1634/theoncologist.2012-0121.
Cardoso F, Senkus E, Costa A, Papadopoulos E, Aapro M, Andre F, et al. 4th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 4)dagger. Ann Oncol. 2018;29(8):1634–57. https://doi.org/10.1093/annonc/mdy192.
National Comprehensive Cancer Network. (NCCN) Clinical Practice Guidelines in Oncology. Breast Cancer, Version 1. 2019. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf Accessed 14 March 2019.
Adam R, Aloia T, Krissat J, Bralet MP, Paule B, Giacchetti S, et al. Is liver resection justified for patients with hepatic metastases from breast cancer? Ann Surg. 2006;244(6):897–907. https://doi.org/10.1097/01.sla.0000246847.02058.1b (discussion -8).
Caralt M, Bilbao I, Cortes J, Escartin A, Lazaro JL, Dopazo C, et al. Hepatic resection for liver metastases as part of the "oncosurgical" treatment of metastatic breast cancer. Ann Surg Oncol. 2008;15(10):2804–10. https://doi.org/10.1245/s10434-008-0072-2.
Hoffmann K, Franz C, Hinz U, Schirmacher P, Herfarth C, Eichbaum M, et al. Liver resection for multimodal treatment of breast cancer metastases: identification of prognostic factors. Ann Surg Oncol. 2010;17(6):1546–54. https://doi.org/10.1245/s10434-010-0931-5.
Cassera MA, Hammill CW, Ujiki MB, Wolf RF, Swanstrom LL, Hansen PD. Surgical management of breast cancer liver metastases. HPB. 2011;13(4):272–8. https://doi.org/10.1111/j.1477-2574.2010.00282.x.
Abbott DE, Brouquet A, Mittendorf EA, Andreou A, Meric-Bernstam F, Valero V, et al. Resection of liver metastases from breast cancer: estrogen receptor status and response to chemotherapy before metastasectomy define outcome. Surgery. 2012;151(5):710–6. https://doi.org/10.1016/j.surg.2011.12.017.
Dittmar Y, Altendorf-Hofmann A, Schule S, Ardelt M, Dirsch O, Runnebaum IB, et al. Liver resection in selected patients with metastatic breast cancer: a single-centre analysis and review of literature. J Cancer Res Clin Oncol. 2013;139(8):1317–25. https://doi.org/10.1007/s00432-013-1440-2.
Ruiz A, Sebagh M, Wicherts DA, Castro-Benitez C, van Hillegersberg R, Paule B, et al. Long-term survival and cure model following liver resection for breast cancer metastases. Breast Cancer Res Treat. 2018;170(1):89–100. https://doi.org/10.1007/s10549-018-4714-1.
Ng KK, Vauthey JN, Pawlik TM, Lauwers GY, Regimbeau JM, Belghiti J, et al. Is hepatic resection for large or multinodular hepatocellular carcinoma justified? Results from a multi-institutional database. Ann Surg Oncol. 2005;12(5):364–73. https://doi.org/10.1245/ASO.2005.06.004.
Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, et al. Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery. 2000;127(5):512–9. https://doi.org/10.1067/msy.2000.105294.
Pivot X, Asmar L, Hortobagyi GN, Theriault R, Pastorini F, Buzdar A. A retrospective study of first indicators of breast cancer recurrence. Oncology. 2000;58(3):185–90. https://doi.org/10.1159/000012098.
Eichbaum MH, Kaltwasser M, Bruckner T, de Rossi TM, Schneeweiss A, Sohn C. Prognostic factors for patients with liver metastases from breast cancer. Breast Cancer Res Treat. 2006;96(1):53–62. https://doi.org/10.1007/s10549-005-9039-1.
Pocard M, Pouillart P, Asselain B, Salmon R. Hepatic resection in metastatic breast cancer: results and prognostic factors. Eur J Surg Oncol. 2000;26(2):155–9. https://doi.org/10.1053/ejso.1999.0761.
Selzner M, Morse MA, Vredenburgh JJ, Meyers WC, Clavien PA. Liver metastases from breast cancer: long-term survival after curative resection. Surgery. 2000;127(4):383–9.
Treska V, Cerna M, Liska V, Treskova I, Narsanska A, Bruha J. Surgery for breast cancer liver metastases—factors determining results. Anticancer Res. 2014;34(3):1281–6.
Treska V, Cerna M, Kydlicek T, Treskova I. Prognostic factors of breast cancer liver metastasis surgery. Arch Med Sci AMS. 2015;11(3):683–5. https://doi.org/10.5114/aoms.2015.52376.
Kostov DV, Kobakov GL, Yankov DV. Prognostic factors related to surgical outcome of liver metastases of breast cancer. J Breast Cancer. 2013;16(2):184–92. https://doi.org/10.4048/jbc.2013.16.2.184.
Pringle JHV. Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg. 1908;48(4):541–9.
Makuuchi M, Mori T, Gunven P, Yamazaki S, Hasegawa H. Safety of hemihepatic vascular occlusion during resection of the liver. Surg Gynecol Obstet. 1987;164(2):155–8.
Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg. 2013;257(2):205–13. https://doi.org/10.1097/SLA.0b013e31827da7fe.
Acknowledgements
This work was jointly supported by the National Natural Science Foundation of China (81874182, 81874056, 81372314, 81272393), the National Key Project of China (2017ZX10203204-007–004), the Public Health Bureau Foundation of Shanghai (201840019), and the Research Talent Foundation of Fudan University Shanghai Cancer Center (YJRC1604). We thank Yifeng Sun, Chenchen Liu, Lei Cheng, Weiqi Xu and Luxi Ye for their help.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained for all patients before surgery, and the Fudan University Shanghai Cancer Center, Zhongshan Hospital or Eastern Hepatobiliary Surgery Hospital Ethics Committee gave ethical approval to perform this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
He, X., Zhang, Q., Feng, Y. et al. Resection of liver metastases from breast cancer: a multicentre analysis. Clin Transl Oncol 22, 512–521 (2020). https://doi.org/10.1007/s12094-019-02155-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02155-2