Abstract
Purpose
The prognostic value of nonsentinel lymph-node (NSLN) status in breast cancer remains unclear. This study was designed to investigate the prognostic value of NSLN status in SLN-positive breast cancer.
Methods
Retrospective 873 consecutive primary breast cancer patients from a single institution who were SLN-positive and underwent axillary lymph-node dissection (ALND) were included. Patients with incomplete clinical information or loss of follow-up were excluded. Survival analysis in patients with the same number of positive LNs and patients belonging to the same American Joint Committee on Cancer (AJCC) node (N) classification was performed to establish a proposal for incorporating the NSLN status into the breast cancer staging system.
Results
The median follow-up was 41 months. Positive NSLN status was a significantly unfavorable factor for recurrence-free survival (RFS) (HR: 4.31, P < 0.001) and distant recurrence-free survival (DRFS) (HR: 3.62, P < 0.001). The survival of patients with one positive SLN and one positive NSLN (N = 97) was significantly worse than that of patients with two positive SLNs (N = 68; RFS, P = 0.011; DRFS, P = 0.027). Positive NSLN status was a significantly unfavorable factor affecting survival in patients with the AJCC N1 classification (N = 806; RFS, HR: 2.85, P = 0.002; DRFS, HR: 2.81, P = 0.004). No significant difference in survival was found between LN-negative (N = 361) and NSLN-negative AJCC N1 classification (N = 363) patients.
Conclusions
Positive NSLN status has an independent prognostic value in breast cancer patients with 1–3 positive LNs, and the NSLN status should be incorporated into the breast cancer staging system.
Similar content being viewed by others
Introduction
Sentinel lymph-node biopsy (SLNB) is a reliable standard diagnostic method in the prognostic staging of patients with breast cancer [1]. Axillary lymph-node dissection (ALND) is an effective method for local treatment of breast cancer, but is associated with a high risk of complications such as the limitation of shoulder movement, paresthesias, arm numbness, and lymphedema. SLNB not only provides an accurate assessment of histological nodal status but also has less acute and chronic morbidities than ALND [2, 3]. In recent years, SLNB has replaced ALND as a staging procedure for patients undergoing primary surgery with clinically negative lymph nodes [4,5,6].
Usually, patients with a positive sentinel lymph node (SLN) are converted to ALND because of the high risk of harboring metastatic nonsentinel lymph nodes (NSLNs). The incidence of NSLN metastases ranges from 27 to 46% when metastases are detected in one or two SLNs by SLNB and increases to as high as 70% in patients with three or more positive SLNs [4, 7, 8]. ALN (including SLNs and NSLNs) status is one of the strongest independent prognostic factors in breast cancer patients, and it guides clinical adjuvant local and systemic treatment decisions [1, 9,10,11]. However, the association between NSLN status and survival in breast cancer remains unclear. In SLN-positive breast cancer patients who underwent ALND, NSLN status may have an important predictive value for prognosis.
The aim of this study was to investigate the prognostic value of NSLN status in SLN-positive breast cancer, and especially excluded the interference of multiple positive LNs on the prognostic value of NSLN metastasis. Finally, this study was aimed to be able to offer a proposal for incorporating the NSLN status into the breast cancer staging system to improve risk stratification in patients.
Materials and methods
Patients
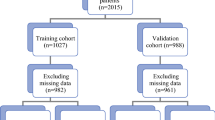
This is a retrospective study enrolled consecutive SLN-positive breast cancer patients who underwent ALND from 2010 to 2017 at Henan Provincial People’s Hospital and is not registered in any official registry. The enrollment criteria for breast cancer patients were as follows: operable single primary breast cancer; underwent both SLNB and ALND; available information on the number and status of axillary LNs (including both SLN and NSLN), and follow-up data. Patients with incomplete clinical information or loss of follow-up, specifically, SLN-positive patients who did not undergo ALND were excluded from this study. All clinical characteristics, such as tumor size, tumor grade, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2) status, SLN status, NSLN status, LN status, and adjuvant therapy, were extracted from the medical records in March 2018. We performed SLNB using methylene blue or indocyanine green alone or in combination. SLNB was performed by experienced surgeons in accordance with the standard operating procedure.
Statistical analysis
To investigate the associations between covariates and NSLN status, the categorical variables were compared using Fisher’s exact test, and the continuous variables were compared using the Mann–Whitney U test. Univariate survival analysis was performed with the Cox proportional hazard model. To identify independent prognostic variables, the statistically significant variable identified by univariate analysis was included in the multivariate survival analysis. Recurrence-free survival (RFS) and distant recurrence-free survival (DRFS) curves were generated by the Kaplan–Meier method with log-rank tests. RFS was defined as the time from the date of pathological diagnosis to the date of local recurrence or metastasis, distant metastasis, death from nonbreast cancer cause, death from unknown cause, or death from breast cancer. DRFS was defined as the time from pathological diagnosis to the date of distant metastasis, death from nonbreast cancer cause, death from unknown cause, or death from breast cancer. At the last follow-up, patients without relapse were censored.
To further confirm that NSLN status is a prognostic factor that is independent of the number of positive LNs, we investigated the association between NSLN status and survival in patients with the same number of positive LNs. The most common case where both SLN and NSLN were positive was two total positive LNs, so the survival analysis was performed with these patients. Furthermore, survival analysis was performed with patients belonging to the same AJCC N classification (N1 and N2 + N3) to establish a proposal for incorporating the NSLN status into the breast cancer staging system.
All tests were two-sided, and the alpha level of significance was set at 5%. All statistical analyses were performed with SPSS 20 software. The present study was performed in accordance with the guidelines of the Research Ethics Committee of Henan Provincial People’s Hospital. Written informed consent was always obtained before any invasive procedure or surgery.
Results
A total of 878 consecutive SLNB-positive female breast patients who underwent ALND were treated at Breast Surgery Department, Henan Provincial People’s Hospital from January 2010 to December 2017. Of these 878 patients, four patients were excluded due to with incomplete clinical information or loss of follow-up. Consequently, 873 patients were included in this study. The clinicopathological characteristics of all 873 patients are shown in Table 1. All these patients subsequently underwent ALND; 372 patients were NSLN-negative and the other 501 patients were NSLN-positive. Positive NSLNs were more likely to be found in patients with larger tumors, more positive SLNs, more excised LNs at ALND, negative ER status, negative PR status, and positive HER2 status.
The median follow-up of this study was 41 months (ranging from 1 to 88 months). The estimated 5-year RFS and DRFS were 90.4% (95% CI: 88.0–92.8%) and 91.6% (95% CI: 89.4–93.8%), respectively. Patients with a positive NSLN status had a significantly worse RFS (unadjusted hazard ratio [HR]: 2.88; 95% CI 1.63–5.10; P < 0.001, Fig. 1a) and DRFS (unadjusted HR: 2.99; 95% CI: 1.58–5.63; P < 0.001, Fig. 1b) than those with a negative NSLN status. Furthermore, multivariate analysis revealed that a positive NSLN status was a significantly unfavorable factor for RFS (adjusted HR: 4.31, 95% CI: 2.44–7.59, P < 0.001) and DRFS (adjusted HR: 3.62, 95% CI: 2.11–6.21, P < 0.001), as were larger tumor size (RFS, HR: 1.86, 95% CI: 1.11–3.13, P = 0.019; DRFS, HR: 1.89, 95% CI: 1.06–3.36, P = 0.030) and more positive LNs (Table 2).
Survival curves according to the pathologic status of the NSLNs in all 873 breast cancer patients: a recurrence-free survival and b distant recurrence-free survival. c, d Reported survival in patients with the same number of positive lymph nodes according to NSLN status (N = 165). NSLN nonsentinel lymph node
The association between NSLN metastasis and survival in patients with the same number of positive LNs was investigated to further rule out the interference of multiple positive LNs in the negative prognostic value of NSLN metastasis. The largest group of patients with both positive SLN and positive NSLN were those patients with two positive LNs, who were, therefore, selected as the cohort for this analysis (N = 165). Survival analysis showed that the survival of patients with one positive SLN and one positive NSLN (N = 97) was significantly worse than the survival of patients with two positive SLNs (N = 68; RFS, P = 0.011, Fig. 1c; DRFS, P = 0.027, Fig. 1d).
To establish a proposal for incorporating the NSLN status into the breast cancer staging system, we performed survival analyses in patients belonging to the same American Joint Committee on Cancer (AJCC) N classification group (N1: 1–3 positive LNs; N2 + N3: 4 or more positive LNs) with a special consideration of NSLN status. In the 806 patients with 1–3 positive LNs (AJCC N1), positive NSLN was a significantly unfavorable prognostic factor for survival (RFS, P < 0.001, Fig. 2a; DRFS, P = 0.001, Fig. 2b). Multivariate analysis revealed that positive NSLN status remained a significantly negative prognostic factor for RFS (adjusted HR: 2.85; 95% CI: 1.56–5.19; P = 0.002) and DRFS (adjusted HR: 2.81; 95% CI: 1.38–5.71; P = 0.004, Table 3), independent of other staging characteristics. However, in the 67 patients with four or more positive LNs (AJCC N2 + N3), the NSLN status was no longer a prognostic factor (RFS, unadjusted HR: 3.17; 95% CI: 0.42–24.05, P = 0.264; DRFS, unadjusted HR: 2.81; 95% CI: 0.37–21.38, P = 0.317).
a, b Reported survival in patients with 1–3 positive lymph nodes (AJCC N1 classification) according to NSLN status (N = 806). c, d Reported survival according to the following classification: Group 1, LN-negative (AJCC N0 classification group, N = 361); Group 2, 1–3 positive LNs: positive SLN but negative NSLN (AJCC N1 classification group, N = 363); Group 3, 1–3 positive LNs: both SLN and NSLN were positive (AJCC N1 classification group, N = 443); Group 4, 4 or more positive LNs (AJCC N2 + N3 group, N = 67). AJCC American Joint Committee on Cancer, NSLN nonsentinel lymph node, SLN sentinel lymph node
Taking all the above findings into account, to further verify the prognostic value of NSLN in breast cancer, additional 361 consecutive LN-negative patients who underwent ALND from 2010 to 2014 were included in the present study. Then, all 1234 patients were reclassified into four groups as follows: Group 1, LN-negative (AJCC N0 classification group, N = 361); Group 2, one to three positive LNs with positive SLNs but negative NSLNs (AJCC N1 classification group, N = 363); Group 3, one to three positive LNs with positive SLNs and NSLNs (AJCC N1 classification group, N = 443); Group 4, four or more positive LNs (AJCC N2 + N3 group, N = 67). This new classification scheme verified the significant prognostic value of NSLN status in breast cancer (RFS, P < 0.001, Fig. 2c; DRFS, P < 0.001, Fig. 2d). After adjustment for the conventional staging features in multivariate analysis, patients in Group 3 and Group 4 had a significantly worse survival than those in Group 1 (Group 3, RFS, HR: 3.15, 95% CI: 1.77–5.61, P < 0.001; DRFS, HR: 2.61, 95% CI: 1.44–4.71, P = 0.002; Group 4, RFS, HR: 7.78, 95% CI: 3.91–15.50, P < 0.001; DRFS, HR: 7.61, 95% CI: 3.78–15.34, P < 0.001, Table 4). Conversely, no significant difference in survival was found between patients in Group 2 and patients in Group 1 (RFS, HR: 1.10, 95% CI: 0.54–2.27, P = 0.792; DRFS, HR: 0.88, 95% CI: 0.41–1.91, P = 0.752, Table 4).
Discussion
The present study investigated the hypothesis that the metastasis of NSLNs has an independent prognostic value for breast cancer patients who underwent ALND and had positive SLNs. Patients with positive NSLNs had worse survival than did patients with negative NSLNs. Survival analysis in subgroup further reinforces evidence of the prognostic role of metastasis in NSLNs independent of the total number of positive LNs. Especially important in the breast cancer staging system, significant prognostic value of NSLN status was found compared to AJCC staging system.
ALND is associated with a significant morbidity and has been replaced as a staging procedure by SLNB, which has fewer negative effects [3, 12,13,14,15,16]. Management of LNs in patients with breast cancer has evolved rapidly in the recent years, and an increasingly conservative approach to axillary staging has been developed [4, 6, 17, 18]. Changes in the management of breast cancer and the selection of systemic therapy based on tumor biology and clinical characteristics raised questions regarding the accurate classification of LNs for patients with SLN metastases. An SLN is the first lymph node in the lymphatic drainage pathway of the tumor bed, so it constitutes the first site of LN involvement. Once the tumor cell breaks through the SLN barrier and migrates to LNs beyond the SLN (NSLN-positive), a higher clinical classification and worse prognosis are indicated. Clinical trials such as the American College of Surgeons Oncology Group (ACOSOG) Z0011 have shown that ALND may be safely omitted in selected clinically node-negative patients with metastasis limited to one or two SLNs [5, 7, 19,20,21]. Our study found no difference in the prognosis of NSLN-negative breast cancer patients with AJCC N1 classification and N0 classification, further validating the safety of avoiding ALND in these selected patients.
Although our results are based on a quite high number of patients, there are still some limitations in our study. For example, most cases used methylene blue or indocyanine green alone or in combination to detect sentinel lymph nodes and the weakness of retrospective nature. Our study still should be validated in the other independent cohorts.
In conclusion, our findings show that positive NSLN status has an independent prognostic value in breast cancer patients with 1–3 positive LNs, and the NSLN status should be incorporated into the conventional breast cancer staging system.
References
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14(7):609–18. https://doi.org/10.1016/S1470-2045(13)70166-9.
Helms G, Kuhn T, Moser L, Remmel E, Kreienberg R. Shoulder-arm morbidity in patients with sentinel node biopsy and complete axillary dissection–data from a prospective randomised trial. Eur J Surg Oncol. 2009;35(7):696–701. https://doi.org/10.1016/j.ejso.2008.06.013.
Veronesi U, Viale G, Paganelli G, Zurrida S, Luini A, Galimberti V, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251(4):595–600. https://doi.org/10.1097/SLA.0b013e3181c0e92a.
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11(10):927–33. https://doi.org/10.1016/S1470-2045(10)70207-2.
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318(10):918–26. https://doi.org/10.1001/jama.2017.11470.
Maguire A, Brogi E. Sentinel lymph nodes for breast carcinoma: a paradigm shift. Arch Pathol Lab Med. 2016;140(8):791–8. https://doi.org/10.5858/arpa.2015-0140-RA.
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252(3):426–32. https://doi.org/10.1097/sla.0b013e3181f08f32 (discussion 32-3).
Veronesi U, Paganelli G, Viale G, Galimberti V, Luini A, Zurrida S, et al. Sentinel lymph node biopsy and axillary dissection in breast cancer: results in a large series. J Natl Cancer Inst. 1999;91(4):368–73.
Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer. 1989;63(1):181–7.
Fisher ER, Costantino J, Fisher B, Redmond C. Pathologic findings from the National surgical adjuvant breast project (Protocol 4). Discriminants for 15-year survival. National surgical adjuvant breast and bowel project investigators. Cancer. 1993;71(6):2141–50.
Jatoi I, Hilsenbeck SG, Clark GM, Osborne CK. Significance of axillary lymph node metastasis in primary breast cancer. J Clin Oncol. 1999;17(8):2334–40. https://doi.org/10.1200/JCO.1999.17.8.2334.
Giuliano AE, Jones RC, Brennan M, Statman R. Sentinel lymphadenectomy in breast cancer. J Clin Oncol. 1997;15(6):2345–50. https://doi.org/10.1200/JCO.1997.15.6.2345.
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349(6):546–53. https://doi.org/10.1056/NEJMoa012782.
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25(24):3657–63. https://doi.org/10.1200/JCO.2006.07.4062.
Rescigno J, Zampell JC, Axelrod D. Patterns of axillary surgical care for breast cancer in the era of sentinel lymph node biopsy. Ann Surg Oncol. 2009;16(3):687–96. https://doi.org/10.1245/s10434-008-0195-5.
Classe JM, Baffert S, Sigal-Zafrani B, Fall M, Rousseau C, Alran S, et al. Cost comparison of axillary sentinel lymph node detection and axillary lymphadenectomy in early breast cancer A national study based on a prospective multi-institutional series of 985 patients ‘on behalf of the Group of Surgeons from the French Unicancer Federation’. Ann Oncol. 2012;23(5):1170–7. https://doi.org/10.1093/annonc/mdr355.
Canavese G, Catturich A, Vecchio C, Tomei D, Gipponi M, Villa G, et al. Sentinel node biopsy compared with complete axillary dissection for staging early breast cancer with clinically negative lymph nodes: results of randomized trial. Ann Oncol. 2009;20(6):1001–7. https://doi.org/10.1093/annonc/mdn746.
Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006;98(9):599–609. https://doi.org/10.1093/jnci/djj158.
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305(6):569–75. https://doi.org/10.1001/jama.2011.90.
Giuliano AE, Ballman K, McCall L, Beitsch P, Whitworth PW, Blumencranz P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 randomized trial. Ann Surg. 2016;264(3):413–20. https://doi.org/10.1097/SLA.0000000000001863.
Bonneau C, Hequet D, Estevez JP, Pouget N, Rouzier R. Impact of axillary dissection in women with invasive breast cancer who do not fit the Z0011 ACOSOG trial because of three or more metastatic sentinel lymph nodes. Eur J Surg Oncol. 2015;41(8):998–1004. https://doi.org/10.1016/j.ejso.2015.04.003.
Funding
This study was supported by the “23456 Talent Project” of Henan Provincial People’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For the institutional cohorts, de-identified data were extracted from the Henan Provincial People’s Hospital Breast Cancer Database. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Si, P., Zhang, P., Chen, T. et al. Positive nonsentinel lymph nodes are associated with poor survival in breast cancer: results from a retrospective study. Clin Transl Oncol 21, 1085–1092 (2019). https://doi.org/10.1007/s12094-018-02031-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-02031-5