Abstract
Background and aims
The association between fatty liver disease (FLD) and cardiovascular disease (CVD) in an Australian context has yet to be defined. The primary aim of this study was to investigate the association between FLD and 3-point major adverse cardiovascular events (MACE).
Methods
This was a longitudinal follow-up study of a randomly sampled adult cohort from regional Australia between 2001 and 2003. Baseline covariates included demographic details, anthropometry, health and lifestyle data, and laboratory tests. Non-alcoholic fatty liver disease (NAFLD) and metabolic-(dysfunction) associated fatty liver disease (MAFLD) were diagnosed in participants with fatty liver index (FLI) ≥ 60 and meeting other standard criteria. ICD-10 codes were used to define clinical outcomes linked to hospitalisations. Three-point MACE defined as non-fatal myocardial infarction (MI) and cerebrovascular accident (CVA) and CVD death.
Results
In total, 1324 and 1444 participants met inclusion criteria for NAFLD and MAFLD analysis, respectively. Over 23,577 and 25,469 person-years follow-up, NAFLD and MAFLD were independent predictors for 3-point MACE, adjusting for demographic covariates and known cardiometabolic risk factors, whilst considering non-CVD death as a competing event (NAFLD: sub-hazard ratio [sHR] 1.56, 95% confidence interval [CI 1.12–2.19]; MAFLD: sHR 1.51, 95% CI 1.11–2.06). The results held true on several sensitivity analyses.
Conclusions
Both forms of FLD increase the risk for CVD independent of traditional cardiometabolic risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD), and the revised term metabolic-(dysfunction) associated fatty liver disease (MAFLD), share key pathophysiological drivers with cardiovascular diseases (CVD), in particular insulin resistance [1]. Natural history studies have consistently demonstrated CVD to be one of the foremost causes of death in those with fatty liver disease (FLD), significantly outweighing death from advanced chronic liver disease [2, 3]. As such, there is debate about expanding the diagnostic criteria for the metabolic syndrome (MetSyn) to incorporate FLD [4].
CVD accounted for two of the top five leading causes of death amongst Australians since 1968, with death due to ischemic heart disease (IHD) consistently the principal cause over this time [5]. In 2021–22, 14.3 billion Australian dollars—close to 10% of total health care expenditure in Australia—was attributable to CVD [6]. This places a significant burden on the healthcare system, which is likely to increase with an aging population [7].
We have previously demonstrated the age- and sex-standardized prevalence of NAFLD to have increased over a 15-year period in regional Victoria, in parallel to generalized obesity [8]. This may influence the CVD prevalence into the future. However, to date, there has not been a population-based study determining the impact of FLD on incident CVD in Australia. Further, studies conducted internationally have failed to unequivocally conclude whether FLD increases the risk of CVD, in particular, fatal CVD [9,10,11].
This study aimed to determine if NAFLD and/or MAFLD independently increased the risk of CVD in a cohort from regional Victoria.
Methods
Study cohort
This is a longitudinal follow-up study from the Crossroads I (CR-1) study conducted in eight major towns in northeast regional Victoria, Australia, between June 2001 and February 2003. The methodology of this study has been previously described in detail [12]. To summarize, households were randomly selected from residential address lists and attended in-person by trained data collectors. Households were selected 1:1 from the two main regional centers and six surrounding rural shires. From each household, all residents aged ≥ 16 years were invited to complete a health questionnaire, with one adult (≥ 18 years old) from participating households invited to enter a clinic sub-study, the Crossroads Undiagnosed Disease Study (CUDS). CUDS collected comprehensive data on demographic details, anthropometry, blood pressure, and more detailed health, diet, and lifestyle questionnaires, including information on alcohol consumption and medication use. Laboratory tests were conducted including full blood examination, biochemistry, liver function tests, fasting lipid profile, fasting glucose, glycosylated hemoglobin (HbA1c) and a urine sample. Further, all people without known diabetes undertook an oral glucose tolerance test. Women who were pregnant were also excluded from undertaking an OGGT. In total, n = 1454 participated in CUDS.
Study outcome
The primary outcome for this study is to investigate if there is a difference in 3-point major adverse cardiovascular events (MACE) in those with NAFLD and MAFLD compared to those without fatty liver disease (FLD). The secondary outcomes are to determine differences in incidence of fatal CVD, 5-point MACE and atrial fibrillation (AF) in those with and without NAFLD and MAFLD, and estimate incidence of myocardial infarction (MI), cerebrovascular accident (CVA) (either hemorrhagic or ischemic), congestive cardiac failure (CCF) and unstable angina (UA) in those with FLD.
Data linkage
Longitudinal outcomes were acquired through the Centre for Victorian Data Linkage (CVDL), which is the custodian for datasets on emergency department presentation, hospital admission, and deaths registered in the state of Victoria, Australia. Data availability for emergency department presentation and death registry was from entry into CUDS, whilst hospital admission data was only available from inception of that dataset (1st July 2007). Underlying cause of death (COD) was also obtained through the Australian Bureau of Statistics. Participants were censored at first occurrence of relevant outcome or 31st October 2022, the final date for data linkage.
Study definitions
NAFLD was diagnosed in those with a Fatty Liver Index (FLI) ≥ 60 [13] in the absence of excessive alcohol consumption (≥ 210/140 g per week in men/women) and chronic viral hepatitis or alternate chronic liver disease (per self-report) [14]. MAFLD was diagnosed in those with FLI ≥ 60 and additional metabolic criteria (overweight/obesity with ethnicity-specific cut-offs for Asians, type 2 diabetes mellitus [T2DM] and/or ‘metabolic dysfunction’), irrespective of alternate cause of liver disease, per the original consensus statement [15] and as endorsed by the Asian Pacific Association for the Study of the Liver (APASL) [16].
MetSyn was diagnosed according to the harmonized criteria agreed upon by a conglomerate of expert international societies [17] as occurring in anyone meeting 3 out of the following 5 criteria: elevated waist circumference, elevated triglycerides, reduced high-density lipoprotein cholesterol (HDL-C), elevated blood pressure and elevated fasting glucose. T2DM was considered in those self-reporting existing diagnosis on administered health questionnaire or as a new diagnosis in those meeting World Health Organization and American Diabetes Association criteria [12, 18]. Dyslipidemia was defined according to lipid parameters as per the Australian Institute of Health and Welfare [19].
Baseline prevalent AF and MACE were coded per health questionnaires. Prevalent MACE included non-fatal MI, CVA, CCF and coronary revascularisation (percutaneous coronary intervention or coronary artery bypass grafting). Three-point MACE included non-fatal MI, non-fatal CVA and death due to CVD, whilst 5-point MACE also included CCF and UA [20]. Events were only considered once (e.g., if a participant had an MI and subsequent CVA, they were coded as having 3-point MACE at time of MI and censored thereafter). CVD-related death, 3- and 5-point MACE, and AF were coded according to International Statistical Classification of Disease and Related Health Problems, 10th revision (ICD-10) manual (Supplementary Table 1) and obtained through the CVDL datasets as noted above, including both primary and secondary reasons for hospitalization.
Elevated alanine aminotransferase (ALT) was considered in those with ALT ≥ 1.5 × the upper limit of normal according to gender (male 30 U/L; female 19 U/L).
Participants were excluded from analysis if there was insufficient data to evaluate FLI and further were excluded from the NAFLD analysis if they had FLI ≥ 60 and a history of excessive alcohol consumption or alternate chronic liver disease.
Statistical analysis
Categorical data are presented as frequency (percentage), with between-group differences calculated using Pearson chi-squared test or Fisher’s exact test, where appropriate. Continuous covariates are presented as median with interquartile range (IQR] or mean with standard deviation (SD) following normality assessment, with Mann–Whitney U test and independent samples t-test utilized to test hypotheses. Incidence rates are presented per 1000 person-years, with group comparisons using incidence rate ratios (IRR), or mortality rate ratio (MRR) for death. Cox proportional hazards regression analysis was used to establish if NAFLD and MAFLD were predictors of outcome on both univariate and multivariate models. Non-CVD deaths were considered as a competing risk on Cox models, except for AF whereby all-cause mortality was considered a competing risk. Results are presented as sub-hazard ratios (sHR) with 95% confidence interval (CI). Multivariate models were adjusted a priori according to demographic, lifestyle and clinical risk factors known to influence the outcome of interest [21]. In detail, Model 1 adjusted for age, gender (male as reference) and education (dichotomized with reference those who had not completed secondary school or above), Model 2 adjusted for Model 1 along with smoking status (non-smoker as reference) and diet adequacy (according to sufficient consumption of fruit and vegetables per day according to Australian guidelines [22]), and Model 3 adjusted for Model 2 as well as T2DM, hypertension, dyslipidaemia and baseline prevalent MACE. Models for AF were the same, except Model 2 was also corrected for excessive alcohol consumption and Model 3 corrected for excessive alcohol consumption and baseline prevalent AF [23]. Sensitivity analyses were conducted excluding those with baseline MACE (and baseline AF for Models investigating AF as outcome), assessing those with FLD versus those with definitively no steatosis (FLI < 30), and only including codes related to primary reason for hospitalization for longitudinal outcomes. A two-tailed p value < 0.05 is considered statistically significant. All analyses were conducted using Stata/IC version 16.1 for Windows (StataCorp, Texas, USA).
Ethics
The Crossroads study was approved by the Goulburn Valley Health Human Research Ethics Committee (GCH-3/99), whilst the current follow-up study has been approved by the Alfred Health Ethics Committee (project 310/22).
Results
Following defined exclusions, a total of n = 1324 and n = 1444 participants had evaluable data for NAFLD and MAFLD analysis, with a prevalence of 35.4% (n = 469) and 40.7% (n = 588), respectively.
Compared to those without FLD, participants with either form of FLD were more likely to be male, older, smokers or ex-smokers, overweight or obese, have MetSyn and its individual components, prevalent MACE, and be taking medication for diabetes and hypertension, but not aspirin (Table 1). Furthermore, fasting levels of glucose, HbA1c, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and triglycerides were higher in those with FLD than those without, whilst HDL-C was lower. There was no difference in prevalence of excessive alcohol consumption or viral hepatitis in those with and without MAFLD.
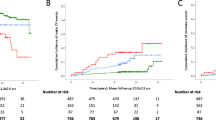
During the follow-up period, 169/1324 (12.8%) developed 3-point MACE, 249/1324 (18.8%) developed 5-point MACE, 81/1324 (6.1%) died from CVD, and 125/1324 (9.4%) developed AF in the NAFLD analysis. During the MAFLD follow-up period, 192/1444 (13.3%) developed 3-point MACE, 281/1444 (19.5%) developed 5-point MACE, 89/1444 (6.2%) died from CVD, and 145/1444 (10.0%) developed AF.
Primary outcome
Follow-up time for 3-point MACE was 23,577 and 25,469 person-years for NAFLD and MAFLD, respectively. Crude 3-point MACE incidence rates were 9.81 per 1000 person-years (95% CI 7.88–12.21) vs 5.77 per 1000 person-years (95% CI 4.69–7.11), and 10.27 per 1000 person-years (95% CI 8.47–12.46) vs. 5.76 per 1000 person-years (95% CI 4.68–7.10) for those with vs without NAFLD, and with vs without MAFLD, respectively. The IRRs were 1.70 (95% CI 1.24–2.32) and 1.78 (95% CI 1.33–2.39) respectively for NAFLD and MAFLD. Both forms of FLD were predictors of 3-point MACE on univariate analysis and on multiple models adjusting for relevant demographic and lifestyle factors (Table 2). On fully adjusted models (Table 2 and Supplementary Table 2) controlling for metabolic risk factors and baseline prevalent MACE, both forms of FLD independently predicted 3-point MACE (NAFLD: sHR 1.56 [95% CI 1.12–2.19]; MAFLD: sHR 1.51 [95% CI 1.11–2.06]). The effect size was similar for each form of FLD.
Secondary outcomes
CVD-related death
Over 24,112 and 26,111 person-years follow-up time for NAFLD and MAFLD, crude incidence rates of CVD-related death were 4.15 per 1000 person-years (95% CI 2.98–5.78) vs 2.93 per 1000 person-years (95% CI 2.20–3.92), and 4.13 per 1000 person-years (95% CI 3.06–5.57) vs 2.93 per 1000 person-years (95% CI 2.19–3.91) for those with vs without NAFLD, and with vs without MAFLD, respectively (NAFLD MRR 1.41 [95% CI 0.88–2.24]; MAFLD MRR 1.41 [95% CI 0.91–2.18]). Neither form of FLD was a predictor for CVD death, either on univariate or multivariate analyses (Table 3).
Ischaemic heart disease was the main cause of CVD-related death in both forms of FLD (NAFLD: 16/35 [45.7%], MAFLD: 20/43 [46.5%]), with a smaller number related to cerebrovascular disease (NAFLD: 7/35 [20%], MAFLD: 8/43 [18.5%]) and the rest from other CVD-related causes.
5-point MACE
Crude incidence rates for 5-point MACE for participants with NAFLD, no NAFLD, MAFLD and no MAFLD were 13.80 per 1000 person-years (95% CI 11.44–16.65), 9.25 per 1000 person-years (95% CI 7.84–10.92), 14.54 per 1000 person-years (95% CI 12.33–17.15) and 9.24 per 1000 person-years (95% CI 7.83–10.90), respectively (NAFLD IRR: 1.49 [95% CI 1.15–1.93]; MAFLD IRR: 1.57 [95% CI 1.24–2.00]). Moreover, when testing the association between FLD and 5-point MACE, the findings were similar to the primary outcome, with both forms of FLD conferring a higher risk of 5-point MACE on univariate and multivariate analysis adjusted for baseline demographics and lifestyle factors, with a trend to significance for both forms of FLD on the fully adjusted model accounting for metabolic risk factors (Table 3). Complete results including all covariates in fully adjusted Model 3 are provided in Supplementary Table 2.
Sensitivity analyses
On sensitivity analysis, excluding participants with baseline prevalent MACE, the results held true as per the primary analysis for MAFLD and to a lesser degree NAFLD, albeit with attenuation of the effect size (Supplementary Table 3). Once more, when comparing those with FLD to those with definitively no steatosis (i.e., FLI < 30), the results held true for 3-point MACE on the fully adjusted models for NAFLD and to a lesser degree MAFLD (Supplementary Table 4). When only considering primary reason for hospitalization for defining longitudinal outcomes, the magnitude of effect for 3-point MACE was marginally reduced, whilst it was accentuated for 5-point MACE such that the result was significant for both NAFLD and MAFLD. On subgroup analysis, NAFLD and MAFLD participants with normal ALT were at a heightened risk of 3-point MACE, whilst there was no significant difference for 3-point MACE in those with elevated ALT. No subgroup was associated with increased 5-point MACE or CVD death when stratified according to normal or elevated ALT (Supplementary Table 5).
CVD during follow-up
Over the follow-up period, incident MI occurred in 64/1217 (5.3%), incident CVA in 45/1217 (3.7%), incident CCF in 81/1217 (6.7%) and incident UA in 42/1217 (3.5%) in the NAFLD analysis, whilst the rates in the MAFLD analysis were 78/1324 (5.9%) for incident MI, 49/1324 (3.7%) for incident CVA, 83/1324 (7.0%) for incident CCF and 50/1324 (3.8%) for incident UA. Considering incident non-fatal CVD events individually, MI and CCF were the most common to occur in both forms of FLD (MI—NAFLD: 4.87 per 1000 person-years [95% CI 3.57–6.63], MAFLD: 5.11 per 1000 person-years [95% CI 3.84–6.79]; CCF—NAFLD: 6.87 per 1000 person-years [5.28–8.92], MAFLD: 5.21 per 1000 person-years [3.93–6.92]), followed by CVA and lastly UA (Table 4). The proportion of events amongst each FLD was similar.
Atrial fibrillation
Incidence rates for atrial fibrillation were 6.73 per 1000 person-years (95% CI 5.17–8.77) vs 4.57 per 1000 person-years (95% CI 3.62–5.78), and 7.47 per 1000 person-years (95% CI 5.96–9.37) vs 4.57 per 1000 person-years (95% CI 3.61–5.77) for those with vs without NAFLD, and those with vs without MAFLD; NAFLD IRR: 1.47 [95% CI 1.01–2.13], MAFLD IRR: 1.64 [95% CI 1.17–2.30]). Neither NAFLD nor MAFLD was associated with a higher risk of AF on any multivariable model (Table 3 and Supplementary Tables 3–5).
Discussion
To date, the influence of FLD—whether NAFLD or MAFLD—on CVD outcomes in Australia has not been established. In this seminal study of a randomly sampled cohort of adults from a major regional center in Australia with over 20 years of follow-up time, we have demonstrated that both forms of FLD carry about a 50% increased risk of 3-point MACE after correction for known CVD risk factors and have a similar influence over 3-point MACE as each other. Almost half the CVD-related deaths in participants with FLD were due to IHD, and non-fatal MI incidence was more common than incident CVA.
FLD and CVD have shared pathophysiology related to the MetSyn, obesity and insulin resistance. Putative factors implicating FLD as an independent risk factor for CVD include a systemic pro-inflammatory state, oxidative stress, abnormal lipid metabolism and direct atherogenicity linked to steatohepatitis itself [24, 25]. Unlike traditional cardiometabolic risk factors of hypertension, dyslipidemia and T2DM, there is currently no approved pharmacotherapy for FLD available across the Asia–Pacific region, which has implications for how modifiable a factor FLD is when considering global CVD risk.
Along with extrahepatic malignancy, CVD has consistently been demonstrated to be the foremost cause of death amongst people with FLD [2, 3]. Meta-analyses investigating the association of NAFLD with CVD have established NAFLD to independently increase the risk of non-fatal CVD, but the impact on fatal CVD has drawn contrasting results [9,10,11]. As such, our finding that NAFLD increases the risk of 3-point MACE—a combined outcome of non-fatal and fatal CVD—but not fatal CVD, and with a trend toward significance for 5-point MACE, is in keeping with the existing literature. It may be that the current study was insufficiently powered to detect differences between groups for fatal CVD. Notably, published meta-analyses are under-represented by studies from Oceania, with no study included from this region, but rather include studies primarily originating from the US, Europe and Asia. This is relevant given the differences in ethnic, cultural, and environmental factors, as well as access to health care, between geographic regions, which could impact the outcome.
Since the FLD nomenclature has shifted, there has been interest in whether the altered diagnostic criteria could have a bearing on clinical outcomes. This is particularly relevant to the proposed change from NAFLD to MAFLD, with the latter allowing for additional aetiologies of chronic liver disease. In the current study, the association between NAFLD and MAFLD and CVD outcomes was near identical, whether investigating 3- or 5-point MACE, or CVD death. The prevailing published reports have not reliably established a difference between the varying forms of FLD, with one large study from Korea suggesting MAFLD but not NAFLD to increase CVD death [26]; however this not being borne out in studies from the US [27, 28]. Trichotomizing FLD to those who meet both NAFLD and MAFLD diagnoses and comparing them to those with MAFLD-only and NAFLD-only, appears to signal differences between groups; MAFLD-only participants carry the highest risk, whilst NAFLD-only participants have the lowest risk that is comparable to the non-FLD population [26, 29, 30]. However, this finding is inconclusive, with other authors finding no difference between groups [27, 28, 31]. We were unable to stratify participants from our cohort in the same manner, as all but a single NAFLD participant met the MAFLD diagnosis. As such, this warrants further investigation, particularly given the complex association between alcohol consumption and CVD [32].
Whilst this is the first description of the association between various forms of FLD and CVD outcomes in a well-characterized randomly sampled cohort of adults from Australia with a long follow-up time, there are limitations to the current study. The cohort was from a single regional area in Australia, which impacts the generalizability of the results to metropolitan locations. However, the concordance in results of the current study with the literature from overseas cohorts with disparate ethnic and socioeconomic backgrounds, increases the external validity of the result. Second, although physical activity—a known lifestyle factor impacting CVD outcomes—was measured in the current cohort at baseline, the data were missing for ~ 30% of participants. Given there was no detectable difference between the FLD and non-FLD groups in amount of physical activity participation per week, this was excluded from the multivariate models. Given BMI and waist circumference are integral in calculating FLI, these too were omitted from multivariable models. Neither homeostatic model assessment for insulin resistance nor high-sensitivity C-reactive protein were measured in participants, which form part of the diagnostic criteria for MAFLD, however, this is unlikely to have significantly influenced the result. Further, the predominant sampled participants for this study are likely to represent a healthy bias. Finally, inherent to all data linkage studies, there is a risk of misattribution/miscoding or missing outcomes, including if participants moved outside the state of Victoria during follow-up.
In conclusion, both NAFLD and MAFLD are associated with a 50% increased risk of 3-point MACE, independent of well-recognized cardiometabolic risk factors. Public health programs are required to ensure that FLD is considered when establishing individuals’ CVD risk profile and CVD outcomes need to be explored when investigating the efficacy of novel FLD pharmacotherapeutic agents.
Data availability
Data may be available upon reasonable request to the corresponding author and following approval by the Victorian Department of Health for outcome data, given linked data is stored on a secure virtual network.
References
Marchesini G, Brizi M, Morselli-Labate AM, Bianchi G, Bugianesi E, McCullough AJ, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107(5):450–455
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113–121
Lazo M, Hernaez R, Bonekamp S, Kamel IR, Brancati FL, Guallar E, et al. Non-alcoholic fatty liver disease and mortality among US adults: prospective cohort study. BMJ. 2011;343: d6891
Fu CE, Yong JN, Ng CH, Nah B, Chew NWS, Chin YH, et al. The prognostic value of including non-alcoholic fatty liver disease in the definition of metabolic syndrome. Aliment Pharmacol Ther. 2023;57(9):979–987
ABS. Causes of Death, Australia: ABS; 2022 [cited 2024 5 April]. Available from: https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/latest-release.
AIHW. Expenditure on cardiovascular disease 2023 [cited 2024 5 April]. Available from: https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/impacts/expenditure-cvd.
AIHW. Older Australians 2023 [cited 2024 5 April]. Available from: https://www.aihw.gov.au/reports/older-people/older-australians/contents/demographic-profile.
Vaz K, Kemp W, Majeed A, Lubel J, Magliano DJ, Glenister KM, et al. Non-alcoholic fatty liver disease prevalence in Australia has risen over 15 years in conjunction with increased prevalence of obesity and reduction in healthy lifestyle. J Gastroenterol Hepatol. 2023;38(10):1823–1831
Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J Hepatol. 2016;65(3):589–600
Wu S, Wu F, Ding Y, Hou J, Bi J, Zhang Z. Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: A systematic review and meta-analysis. Sci Rep. 2016;6:33386
Mantovani A, Csermely A, Petracca G, Beatrice G, Corey KE, Simon TG, et al. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6(11):903–913
Simmons D, McKenzie A, Eaton S, Shaw J, Zimmet P. Prevalence of diabetes in rural Victoria. Diabetes Res Clin Pract. 2005;70(3):287–290
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202–209
Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14(6):889–919
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S19–S40
AIHW. Risk factors to health: Abnormal blood lipids (dyslipidaemia) 2017 [cited 2022 12 December]. Available from: https://www.aihw.gov.au/reports/biomedical-risk-factors/risk-factors-to-health/contents/abnormal-blood-lipids-dyslipidaemia.
Bosco E, Hsueh L, McConeghy KW, Gravenstein S, Saade E. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol. 2021;21(1):241
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808
NHMRC. Australian dietary guidelines 2016 [cited 2022 12 December]. Available from: https://www.eatforhealth.gov.au.
Elliott AD, Middeldorp ME, Van Gelder IC, Albert CM, Sanders P. Epidemiology and modifiable risk factors for atrial fibrillation. Nat Rev Cardiol. 2023;20(6):404–417
Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69(9):1691–1705
Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341–1350
Yoo TK, Lee MY, Kim SH, Zheng MH, Targher G, Byrne CD, et al. Comparison of cardiovascular mortality between MAFLD and NAFLD: A cohort study. Nutr Metab Cardiovasc Dis. 2023;33(5):947–955
Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021;75(6):1284–1291
Huang Q, Zou X, Wen X, Zhou X, Ji L. NAFLD or MAFLD: Which Has Closer Association With All-Cause and Cause-Specific Mortality?-Results From NHANES III. Front Med (Lausanne). 2021;8: 693507
Zhang YC, Lyu ZY, Ma B, Li LM, Wang W, Sheng C, et al. A new risk stratification strategy for fatty liver disease by incorporating MAFLD and fibrosis score in a large US population. Hepatol Int. 2022;16(4):835–845
Lee H, Lee YH, Kim SU, Kim HC. Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2021;19(10):2138–2147
Kim KS, Hong S, Ahn HY, Park CY. Metabolic Dysfunction Associated Fatty Liver Disease and Mortality A Population-Based Cohort Study. Diabetes Metab J. 2023;47:220–231
Piano MR. Alcohol’s Effects on the Cardiovascular System. Alcohol Res. 2017;38(2):219–241
Acknowledgements
The authors acknowledge the Australian Government Department of Health and Aged Care Rural Health Multidisciplinary Training Programme. We thank the Baker International Diabetes Institute for their support during Crossroads I. This research is supported by an Australian Government Research Training Program (RTP) scholarship. The authors would like acknowledge the Victorian Department of Health as the source of admitted VAED, emergency VEMD, non-admitted VINAH and cost VCDC datasets for this study, and the Centre for Victorian Data Linkage (Victorian Department of Health) for the provision of data linkage.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. None.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the following: (1) conceptualization and design of the study (KV, SKR), or acquisition of data (KV, DM, LB, DS), or analysis and interpretation of data (all authors), (2) drafting of the article (KV, SKR) or revising it critically for important intellectual content (all authors), (3) final approval of the version to be submitted (all authors). KV is the guarantor for this article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no relevant financial or non-financial conflict of interests to disclose.
Ethical approval
The Crossroads study was approved by the Goulburn Valley Health Human Research Ethics Committee (GCH-3/99), whilst the current follow-up study has been approved by the Alfred Health Ethics Committee (project 310/22).
Informed consent
Participants in the Crossroads study provided informed consent to participate. Individual informed consent for the current study on outcomes was waived by the Alfred Health Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vaz, K., Kemp, W., Majeed, A. et al. NAFLD and MAFLD independently increase the risk of major adverse cardiovascular events (MACE): a 20-year longitudinal follow-up study from regional Australia. Hepatol Int (2024). https://doi.org/10.1007/s12072-024-10706-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12072-024-10706-1