Abstract
Background
Propranolol, a non-selective beta-blocker, commonly used to prevent variceal bleed, but might precipitate circulatory dysfunction in severe ascites. Midodrine, an alpha-1 adrenergic agonist improves renal perfusion and systemic hemodynamics. Addition of midodrine might facilitate higher maximum tolerated dose (MTD) of propranolol, thereby less risk of variceal bleed in cirrhosis patients with severe ascites.
Methods
140 patients with cirrhosis and severe/refractory ascites were randomized- propranolol and midodrine (Gr.A,n = 70) or propranolol alone (Gr.B,n = 70). Primary outcome was incidence of bleed at 1 year. Secondary outcomes included ascites control, achievement of target heart rate (THR), HVPG response and adverse effects.
Results
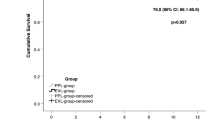
Baseline characteristics were comparable between two groups. Cumulative incidence of bleed at 1 year was lower in Gr.A than B (8.5%vs.27.1%,p-0.043). The MTD of propranolol was higher in Gr.A (96.67 ± 36.6 mg vs. 76.52 ± 24.4 mg; p-0.01) and more patients achieved THR (84.2%vs.55.7%,p-0.034). Significantly higher proportion of patients in Gr.A had complete resolution of ascites [17.1%vs.11.4%,p-0.014), diuretic tolerance (80%vs.60%,p-0.047) at higher doses(p-0.02) and lesser need for paracentesis. Patients in Gr.A also had greater reduction in variceal grade (75.7%vs.55.7%;p-0.01), plasma renin activity (54.4% from baseline) (p = 0.02). Mean HVPG reduction was greater in Gr.A than B [4.38 ± 2.81 mmHg(23.5%) vs. 2.61 ± 2.87 mmHg(14.5%),p-0.045]. Complications like post-paracentesis circulatory dysfunction and spontaneous bacterial peritonitis on follow-up were higher in Gr.B than A (22.8%vs.51.4%,p = 0.013 and 10%vs.15.7%, p = 0.03, respectively).
Conclusion
Addition of midodrine facilitates effective use of propranolol in higher doses and greater HVPG reduction, thereby preventing first variceal bleed, reduced paracentesis requirements with fewer ascites- related complications in patients with cirrhosis with severe/refractory ascites.

Similar content being viewed by others
Data availability
Study related data is available on reasonable request.
Abbreviations
- PICD:
-
Paracentesis-induced circulatory dysfunction
- ACLF:
-
Acute-on-chronic liver failure
- PHT:
-
Portal hypertension
- NSBBs:
-
Non-selective beta-blockers
- HVPG:
-
Hepatic venous pressure gradient
- ILBS:
-
Institute of Liver and Biliary Sciences
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- INR:
-
International normalization ratio
- UGIE:
-
Upper gastrointestinal endoscopy
- THR:
-
Target heart rate
- MTD:
-
Maximum tolerated dose
- SBP:
-
Systolic blood pressure
- WHVP:
-
Wedged hepatic venous pressure
- FHVP:
-
Free hepatic venous pressure
- HCC:
-
Hepatocellular carcinoma
- AKI:
-
Acute kidney injury
- AKIN:
-
Acute kidney injury network
- HE:
-
Hepatic encephalopathy
- MELD:
-
Model for end-stage liver disease
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
References
Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922–938
Bambha K, Kim WR, Pedersen R, et al. Predictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis. Gut 2008;57:814–820
de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C, et al. Baveno VII - Renewing consensus in portal hypertension. J Hepatol 2022;76(4):959–974
Serste T, Melot C, Francoz C, Durand F, Rautou PE, Valla D, et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology 2010;52:1017–1022
Kalambokis GN, Christodoulou D, Baltayiannis G, Christou L. Propranolol use beyond months increases mortality in patients with Child-Pugh C cirrhosis and ascites. Hepatology 2016;64(5):143–8
Kim SG, Larson JJ, Lee JS, Therneau TM, Kim WR. Beneficial and harmful effects of nonselective beta blockade on acute kidney injury in liver transplant candidates. Liver Transpl 2017;23(6):733–740
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65(1):310–335
Angeli P, Volpin R, Piovan D, Bortoluzzi A, Craighero R, Bottaro S, et al. Acute effects of the oral administration of midodrine, an alpha-adrenergic agonist, on renal hemodynamics and renal function in cirrhotic patients with ascites. Hepatology 1998;28:937–943
Kalambokis G, Fotopoulos A, Economou M, Pappas K, Tsinos EV. Effects of a 7 day treatment with midodrine in nonazotemic cirrhotic patients with and without ascites. J Hepatol 2007;46:213–221
Singh V, Dheerendra PC, Singh B, Nain CK, Chawla D, Sharma N, et al. Midodrine versus albumin in the prevention of paracentesis-induced circulatory dysfunction in cirrhotics: a randomized pilot study. Am J Gastroenterol 2008;103:1399–1405
Kumar A, Sharma P, Sarin SK. Hepatic venous pressure gradient measurement: time to learn! Indian J Gastroenterol 2008;27(2):74–80
Wong F. Acute kidney injury in liver cirrhosis: new definition and application. Clin Mol Hepatol 2016;22(4):415–422
Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: Final report of the working party at the 11thWorld Congresses of Gastroenterology, Vienna, 1998. Hepatology 2002;35(3):716–721
Llovet JM, Ducreux M, Lencioni R, et al. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer 2012;48(5):599–641
Lay CS, Tsai Y-T, Teg C-Y, et al. Endoscopic variceal ligation in prophylaxis of first variceal bleeding in cirrhotic patients with high-risk esophageal varices. Hepatology 1997;25:1346–1350
Pascal J-P, Cales P. Multicenter study group. Propranolol in the pre-vention of first upper gastrointestinal tract hemorrhage in patients with cir rhosis of the liver and esophageal varices N Engl J Med 1987;317:856–61
The Italian Multicenter Project for Propranolol in Prevention of Bleeding Propranolol for prophylaxis of bleeding in cirrhotic patients with large varices: a multicenter, randomized clinical trial. Hepatology 1988;8(1) 1–5
Sarin SK. Long term management of oesophageal varices. Drugs 1992;44(Suppl 2):56–69
Premkumar M, Rangegowda D, Vyas T, Khumuckham JS, Shasthry SM, Thomas SS, et al. Carvedilol combined with ivabradine improves left ventricular diastolic dysfunction, clinical progression, and survival in cirrhosis. Clin Gastroenterol 2020;54(6):561–568
Sersté T, Francoz C, Durand F, Rautou PE, Melot C, Valla D, et al. Beta-blockers cause paracentesis-induced circulatory dysfunction in patients with cirrhosis and refractory ascites: a cross-over study. J Hepatol 2011;55(4):794–799
Turco L, Villanueva C, La Mura V, García-Pagán JC, Reiberger T, Genescà J, et al. Lowering portal pressure improves outcomes of patients with cirrhosis, with or without ascites: a meta-analysis. Clin Gastroenterol Hepatol 2020;18(2):313–327.e6
Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med 1999;340(13):988–993
Funding
None.
Author information
Authors and Affiliations
Contributions
AR, AJ, RM, CV,VA, and SKS – :conceptualization, review, analysis, and editing of manuscript. AR, and AJ – original draft preparation. SKS: – conceptualization, review and editing of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Abhijeet Ranjan, Ankur Jindal, Rakhi Maiwall, Chitranshu Vashishtha, Rajan Vijayaraghavan, Vinod Arora, Shiv K Sarin: none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ranjan, A., Jindal, A., Maiwall, R. et al. Midodrine plus propranolol versus propranolol alone in preventing first bleed in patients with cirrhosis and severe ascites: a randomized controlled trial. Hepatol Int (2024). https://doi.org/10.1007/s12072-024-10687-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12072-024-10687-1