Abstract
Background and aim
Changing terminology of non-alcoholic fatty liver disease (NAFLD) to metabolic dysfunction-associated fatty liver disease (MAFLD) is recently proposed by expert panels based on metabolic dysregulations. However, clinical evidences for the risk of cardiovascular disease (CVD) in MAFLD are limited. The aim of this study is evaluating the association of cardiovascular risk in these two terminology and subgroups of MAFLD.
Methods
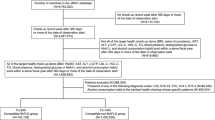
A total of 2133 individuals who underwent ultrasound and cardiac computed tomography contemporaneously were included at a single medical checkup center. Ultrasound was used to define fatty liver, and coronary artery calcification (CAC) defined a coronary artery calcium score above 0 was used to estimate the cardiovascular risk.
Results
Overall, 911 participants were diagnosed with fatty liver. In the unadjusted analysis, NAFLD (OR = 1.4, 95% confidence interval [CI] = 1.05–1.85, p = 0.019) and MAFLD (OR = 1.55, 95% CI = 1.29–1.86, p = 0.046) were significantly associated with CAC. However, in sex and age-adjusted analyses, only MAFLD was associated with CAC (adjusted OR [aOR] = 1.38, 95% CI = 1.14–1.69, p = 0.001). Of the three subgroups of MAFLD (diabetic, nondiabetic overweight/obese, and nondiabetic normal weight/lean with at least two metabolic abnormalities), only diabetic MAFLD was associated with CAC (aOR = 2.65, 95% CI = 1.98–3.55, p < 0.001). When the minimal number of metabolic risk abnormalities increased to three, nondiabetic normal-weight/lean MAFLD was associated with CAC (aOR = 1.35, 95% CI = 1.02–1.77, p = 0.034).
Conclusion
Diabetic MAFLD predicted high-risk CVD phenotypes the best. Metabolic risk abnormalities in nondiabetic MAFLD patients were independently associated with the risk of CVD. The proposed diagnostic criteria for nondiabetic MAFLD need further investigation in terms of CVD risk.


Similar content being viewed by others
Data availability
The data supporting findings of this study are available from the corresponding authors upon reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- APRI:
-
AST to platelet ratio index
- AST:
-
Serum aspartate aminotransferase
- CAC:
-
Coronary artery calcification
- CVD:
-
Cardiovascular disease
- FIB-4:
-
Fibrosis-4
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
High-density lipoprotein cholesterol
- hsCRP:
-
High-sensitivity C reactive protein
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- NFS:
-
NAFLD fibrosis score
- T2DM:
-
Type 2 diabetes mellitus
- WC:
-
Waist circumference
References
Kang SH, Lee HW, Yoo JJ, Cho Y, Kim SU, Lee TH, et al. KASL clinical practice guidelines: management of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2021;27:363–401
Muthiah MD, Sanyal AJ. Burden of disease due to nonalcoholic fatty liver disease. Gastroenterol Clin North Am. 2020;49:1–23
Toh JZK, Pan XH, Tay PWL, Ng CH, Yong JN, Xiao J, et al. A meta-analysis on the global prevalence, risk factors and screening of coronary heart disease in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2021;20:2462–2473
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Kang SH, Cho Y, Jeong SW, Kim SU, Lee JW, Korean NSG. From nonalcoholic fatty liver disease to metabolic-associated fatty liver disease: big wave or ripple? Clin Mol Hepatol. 2021;27:257–269
Lim GEH, Tang A, Ng CH, Chin YH, Lim WH, Tan DJH, et al. An observational data meta-analysis on the differences in prevalence and risk factors between MAFLD vs NAFLD. Clin Gastroenterol Hepatol. 2023;21(619–629): e7
Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021;19(2172–2181): e2176
Ciardullo S, Perseghin G. Prevalence of NAFLD, MAFLD and associated advanced fibrosis in the contemporary United States population. Liver Int. 2021;41:1290–1293
Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19(2138–2147): e2110
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American heart association committee on cardiovascular imaging and intervention, council on cardiovascular radiology and intervention, and committee on cardiac imaging. Council Clin Cardiol Circ. 2006;114:1761–1791
Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary Calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72:434–447
McEvoy JW, Blaha MJ, Defilippis AP, Budoff MJ, Nasir K, Blumenthal RS, et al. Coronary artery calcium progression: an important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56:1613–1622
Sinn DH, Kang D, Chang Y, Ryu S, Gu S, Kim H, et al. Non-alcoholic fatty liver disease and progression of coronary artery calcium score: a retrospective cohort study. Gut. 2017;66:323–329
Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J. 2011;35:561–566
Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33 Suppl 1:S62–69. https://doi.org/10.2337/dc10-S062.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–1357
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005;112:2735–2752
Lin ZH, Xin YN, Dong QJ, Wang Q, Jiang XJ, Zhan SH, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53:726–736
Tamaki N, Kurosaki M, Huang DQ, Loomba R. Noninvasive assessment of liver fibrosis and its clinical significance in nonalcoholic fatty liver disease. Hepatol Res. 2022;52(6):497–507. https://doi.org/10.1111/hepr.13764
Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40:3018–3030
EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–1402
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology. 2018;67:328–357
Kim D, Choi SY, Park EH, Lee W, Kang JH, Kim W, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology. 2012;56:605–613
Chang Y, Ryu S, Sung KC, Cho YK, Sung E, Kim HN, et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: evidence from the Kangbuk Samsung Health Study. Gut. 2019;68:1667–1675
Kim SH, Park HY, Lee HS, Jung KS, Lee MH, Jhee JH, et al. Association between non-alcoholic fatty liver disease and coronary calcification depending on sex and obesity. Sci Rep. 2020;10:1025
Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: Generalized estimating equation approach. Hepatol Res. 2021;51:1115–1128
Lassale C, Tzoulaki I, Moons KGM, Sweeting M, Boer J, Johnson L, et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J. 2018;39:397–406
Ampuero J, Aller R, Gallego-Duran R, Banales JM, Crespo J, Garcia-Monzon C, et al. The effects of metabolic status on non-alcoholic fatty liver disease-related outcomes, beyond the presence of obesity. Aliment Pharmacol Ther. 2018;48:1260–1270
Kanwal F, Kramer JR, Li L, Dai J, Natarajan Y, Yu X, et al. Effect of metabolic traits on the risk of cirrhosis and hepatocellular cancer in nonalcoholic fatty liver disease. Hepatology. 2020;71:808–819
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554
Henson JB, Simon TG, Kaplan A, Osganian S, Masia R, Corey KE. Advanced fibrosis is associated with incident cardiovascular disease in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2020;51:728–736
Moreno-Del Castillo MC, Sanchez-Rodriguez A, Hernandez-Buen Abad JJ, Aguirre-Valadez J, Ruiz I, Garcia-Buen Abad R, et al. Importance of evaluating cardiovascular risk and hepatic fibrosis in patients with newly diagnosed nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:997–999
Baratta F, Pastori D, Angelico F, Balla A, Paganini AM, Cocomello N, et al. Nonalcoholic fatty liver disease and fibrosis associated with increased risk of cardiovascular events in a prospective study. Clin Gastroenterol Hepatol. 2020;18(2324–2331): e2324
Niikura T, Imajo K, Ozaki A, Kobayashi T, Iwaki M, Honda Y, et al. Coronary artery disease is more severe in patients with non-alcoholic steatohepatitis than fatty liver. Diagnostics (Basel). 2020;10:129
Park JG, Jung J, Verma KK, Kang MK, Madamba E, Lopez S, et al. Liver stiffness by magnetic resonance elastography is associated with increased risk of cardiovascular disease in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2021;53:1030–1037
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2935–2959
Funding
JGP receives funding supported by the 2022 Yeungnam University Research Grant. RL receives funding support from NCATS (5UL1TR001442), NIDDK (U01DK061734, U01DK130190, R01DK106419, R01DK121378, R01DK124318, P30DK120515), NHLBI (P01HL147835), and NIAAA (U01AA029019).
Author information
Authors and Affiliations
Contributions
JGP and SYP is guarantor of integrity of the entire study. JGP designed the study and partially supervised by RL. All authors except RL collected data, which were reviewed by GJP, and analyzed by GJP based on the statistical analysis plan. GJP, MKG, and YLR drafted the manuscript, which was critically revised by SYP. All authors were responsible for collecting and interpretation of the data and approved the final version of manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
RL serves as a consultant for Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myer Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse bio, Hightide, Inipharm, Intercept, Inventiva, Ionis, Janssen Inc., Madrigal, Metacrine, Inc., NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, and Viking Therapeutics. In addition, his institution has received grant support from Allergan, Astrazeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Genfit, Gilead, Intercept, Inventiva, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Pfizer, and Sonic Incytes. He is also co-founder of Liponexus, Inc.
Ethical approval
This study was performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki as revised in 2013. The study protocol was approved by the institutional review board of the study center (IRB No. KNUH-2021-07-057-001). The requirement for informed consent from the study participants was waived by the ethics committee because of the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kang, M.K., Lee, Y.R., Jang, S.Y. et al. Impact of metabolic factors on risk of cardiovascular disease in nondiabetic metabolic dysfunction-associated fatty liver disease. Hepatol Int 17, 626–635 (2023). https://doi.org/10.1007/s12072-023-10517-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10517-w