Abstract
Background/purpose of the study
Mortality from hepatitis B virus (HBV)-related acute-on-chronic liver failure (ACLF) is high. Severe infection is the most important complication that affects the outcomes of ACLF patients. Thymosin α1 (Tα1) can improve immune imbalance and this study aimed to investigate the safety and efficacy of Tα1 treatment for HBV-related ACLF.
Methods
From 2017 to 2019, 120 patients with HBV-related ACLF were enrolled in this open-label, randomized, and controlled clinical trial (ClinicalTrial ID: NCT 03082885). The control group (N = 58) was treated with standard medical therapy (SMT) only. The experimental group (N = 56) was subcutaneously injected with 1.6 mg of Tα1 once a day for the first week and then twice a week from week 2 to week 12.
Results
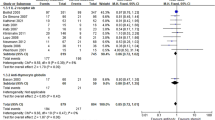
The 90-day cumulated liver transplantation free survival rate of the Tα1 group was 75.0% (95% confidence interval 63.2–86.8%) versus 53.4% (95% confidence interval 39.7–67.1%) for the SMT group (p = 0.030). No significant difference was found in the survival using competitive risk analysis. The incidences of new infection and hepatic encephalopathy in the Tα1 group were much lower than those in the SMT group (32.1% vs 58.6%, p = 0.005; 8.9% vs 24.1%, p = 0.029, respectively). Mortality from severe infection in the SMT group was higher than in the Tα1 group (24.1% vs 8.9%, p = 0.029).
Conclusion
Tα1 is safe for patients with HBV-related ACLF and significantly improves the 90-day liver transplantation-free survival rate. There may be a subgroup which may benefit from Tα1 therapy by the mechanism of preventing infection.


Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACLF:
-
Acute-on-chronic liver failure
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CI:
-
Confidence interval
- CLIF-C OF:
-
Chronic liver failure consortium organ failure
- CLIF-SOFA:
-
Chronic liver failure consortium sequential organ failure assessment
- CRP:
-
C-reactive protein
- CTL:
-
Cytotoxic T cells
- Cr:
-
Creatinine
- CT:
-
Computed tomography
- DCs:
-
Dendritic cells
- ESR:
-
Red blood cell sedimentation rate
- HBV:
-
Hepatitis B virus
- HR:
-
Hazard ratio
- Th:
-
Helper T
- INR:
-
International normalized ratio
- ITT:
-
Intent-to-treat
- MELD:
-
Model for end-stage liver disease
- MAPK:
-
Mitogen-activated protein kinases
- MRI:
-
Magnetic resonance imaging
- NK:
-
Natural killer
- NF-κB:
-
Nuclear factor-κ-gene binding
- NNT:
-
Number needed to treat
- PCT:
-
Procalcitonin
- PTA:
-
Prothrombin activity
- SAE:
-
Serious adverse events
- SMT:
-
Standard medical therapy
- TB:
-
Total bilirubin
- Tα1:
-
Thymosin α1
- TLR:
-
Toll-like receptor
- WBCs:
-
White blood cells
References
Liu XY, Hu JH, Wang HF. Analysis of prognostic factors for patients with acute-on-chronic liver failure. Chin J Hepatol. 2009;17:607–610
Garg H, Kumar A, Garg V, Sharma P, Sharma BC, Sarin SK. Clinical profile and predictors of mortality in patients of acute-on-chronic liver failure. Digest Liver Dis. 2012;44:166–171
Liu XY, Hu JH, Wang HF, Chen JM. Etiological analysis of 1977 patients with acute liver failure, subacute liver failure and acute-on-chronic liver failure. Chin J Hepatol. 2008;16:772–775
Chan AC, Fan ST, Lo CM, Liu CL, Chan SC, Nq KK, et al. Liver transplantation for acute-on-chronic liver failure. Hepatol Int. 2009;3:571–581
Lin BL, Pan CQ, Xie DY, Xie JQ, Xie SB, Zhang XH, et al. Entecavir improves the outcome of acute-on- chronic liver failure due to the acute exacerbation of chronic hepatitis B. Hepatol Int. 2013;7:460–467
Shi F, Zhang JY, Zeng Z, Tien P, Wang FS. Skewed ratios between CD3+ T cells and monocytes are associated with poor prognosis in patients with HBV-related acute-on-chronic liver failure. Biochem Biophys Res Commun. 2010;402:30–36
Zhang GL, Xie DY, Lin BL, Xie C, Ye YN, Peng L, et al. Imbalance of interleukin-17-producing CD4 T cells/regulatory T cells axis occurs in remission stage of patients with hepatitis B virus-related acute-on-chronic liver failure. J Gastroen Hepatol. 2013;28:513–521
Fernández J, Acevedo J, Weist R, Gustot T, Amoros A, Deulofeu C, et al. Bacterial and fungal infections in acute-on-chronic liver failure: prevalence, characteristics and impact on prognosis. Gut. 2018;67:1870–1880
Rout G, Jadaun SS, Ranjan G, Kedia S, Gunjan D, Nayak B, et al. Prevalence, predictors and impact of bacterial infection in acute on chronic liver failure patients. Digest Liver Dis. 2018;50:1–7
Linderoth G, Jepsen P, Schonheyder HC, Johnsen SP, Sorensen ST. Short-term prognosis of community-acquired bacteremia in patients with liver cirrhosis or alcoholism: a population-based cohort study. Alcohol Clin Exp Res. 2006;30:636–641
Mücke MM, Rumyantseva T, Mücke VT, Schwarzkopf K, Joshi S, Kempf VAJ, et al. Bacterial infection-triggered acute-on-chronic liver failure is associated with increased mortality. Liver Int. 2018;38:645–653
Sarin SK, Choudhury A, Sharma MK, Maiwall R, Mahtab MAI, Rahman S, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int. 2019;13:353–390
Ye YN, Gao ZL. Three shock hypotheses that may induce liver failure. Chin J Hepatol. 2009;17:638–640
Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghöner A, Vidacek D, Siewert E, et al. Patients with acute on chronic liver failure display ‘sepsis-like’ immune paralysis. J Hepatol. 2005;42:195–201
Xing T, Li L, Cao H, Huang J. Altered immune function of monocytes in different stages of patients with acute on chronic liver failure. Clin Exp Immunol. 2007;147:184–188
Wu X, Jia J, You H. Thymosin alpha1 treatment in chronic hepatitis B. Expert Opin Biol Ther. 2015;15(Suppl 1):S129–S132
Camerini R, Garaci E. Historical review of thymosin α 1 in infectious diseases. Expert Opin Biol Ther. 2015;15(Suppl 1):S117–S127
Garaci E, Pica F, Matteucci C, Gaziano R, D’Agostini C, Miele MT, et al. Historical review on thymosin α1 in oncology: preclinical and clinical experiences. Expert Opin Biol Ther. 2015;15(Suppl 1):S31–S39
Yao Q, Doan LX, Zhang R, Bharadwaj U, Li M, Chen C. Thymosin-α1 modulates dendritic cell differentiation and functional maturation from human peripheral blood CD14+ monocytes. Immunol Lett. 2007;110:110–120
Zhang Y, Chen H, Li YM, Zeng SS, Chen YG, Li LJ, et al. Thymosin α1- and ulinastatin-based immunomodulatory strategy for sepsis arising from intra-abdominal infection due to carbapenem-resistant bacteria. J Infect Dis. 2008;198:723–730
Liu F, Wang HM, Wang T, Zhang YM, Zhu X. The efficacy of thymosin α1 as immunomodulatory treatment for sepsis: a systematic review of randomized controlled trials. BMC Infect Dis. 2016;16:488
Li C, Bo L, Liu Q, Jin F. Thymosin alpha1 based immunomodulatory therapy for sepsis: a systematic review and meta-analysis. Int J Infec Dis. 2015;33:90–96
Sarin SK, Kedarisetty CK, Abbas Z, Amarapurkar D, Bihari C, Chan ACY, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the study of the liver (APASL) 2014. Hepatol Int. 2014;8:453–471
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, CMA; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, CMA. Diagnostic and Treatment Guidelines for Liver Failure in China (2012). Chin J Clin Infect Pis 2012;5:321–7.
Møller S. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417
Sarin SK, Kumar A, Almeida JA, Chawla YK, Fan ST, Garg H, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int. 2009;3:269–282
Wu X, Shi Y, Zhou J, Sun Y, Piao H, Jiang W, et al. Combination of entecavir with thymosin alpha-1 in HBV-related compensated cirrhosis: a prospective multicenter randomized open-label study. Expert Opin Biol Ther. 2018;18(sup1):61–69
Yang X, Chen Y, Zhang J, Tang T, Kong Y, Ye F, et al. Thymosin α1 treatment reduces hepatic inflammation and inhibits hepatocyte apoptosis in rats with acute liver failure. Exp Ther Med. 2018;15:3231–3238
Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld AB. The diagnostic accuracy of procalcitonin for bacteraemia: a systematic review and meta-analysis. Clin Microbiol Infect. 2015;21:474–481
Anand D, Das S, Ray S, Bhargava S, Srivastava LM. Interrelationship between procalcitonin and organ failure in sepsis. Indian J Clin Biochem. 2014;29:93–96
Leli C, Ferranti M, Moretti A, Al Dhahab ZS, Cenci E, Mencacci A. Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections. Dis Markers. 2015;2015:1–8
Li S, Rong H, Guo Q, Chen Y, Zhang G, Yang J. Serum procalcitonin levels distinguish Gram-negative bacterial sepsis from Gram-positive bacterial and fungal sepsis. J Res Med Sci. 2016;21:39
Chien RN, Lin CY, Yeh CT, Liaw YF. Hepatitis B virus genotype B is associated with better response to thymosin α1 therapy than genotype C. J Viral Hepatitis. 2006;13:845–850
Iino S, Toyota J, Kumada H, Kiyosawa K, Kakumu S, Sata M, et al. The efficacy and safety of thymosinalpha-1 in Japanese patients with chronic hepatitis B; results from a randomized clinical trial. J Viral Hepatitis. 2005;12:300–306
Acknowledgements
We thank all the patients participated in this research. We thank Professor Jian-rong He (Guangzhou Women and Children’s Medical Center) for directing us in data statistics. We thank Yu-xin Yang and Jin-xiu Cao for help in proofreading the manuscript.
Funding
This research was supported by the following funding sources: National Natural Science Foundation of China (82070612, 81901940); National Science and Technology Major Project of China(2018ZX10302204, 2017ZX10203201003); Natural Science Foundation of Guangdong Province (2021A1515010306); The Guangzhou Major Project in collaborative innovation of industry (1561000157).
Author information
Authors and Affiliations
Contributions
B-lL, J-fC, S-rC, Z-yL, H-jC, S-qZ, W-zW, JX, D-nL, JZ and Y-bZ performed clinical study; B-lL and Z-lG provided financial support for this work; B-lL designed the study; J-fC and B-lL performed the analysis and interpretation of the data; J-fC and B-lL wrote and edited the manuscript. The corresponding authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
In this study, Sciclone pharmaceuticals, as the Marketing Authorization Holder of Tα-1 in China, reported SAEs to the drug and regulatory and health authorities after being informed by investigators. Sciclone did not play any role in the design, conduct or funding of this study. The authors have no conflict of interest to declare.
Ethical approval
This study conformed strictly to the Ethical Guidelines of the 1975 Declaration of Helsinki. The study protocol was approved by the Ethics Committee on Clinical Trials of the Third Affiliated Hospital of Sun Yat-sen University in 2016. This study is registered at ClinicalTrials.gov (NCT 03082885). Informed consent was obtained from all patients for being included in the study.
Consent for publication
Consent for publication was obtained from all co-authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, Jf., Chen, Sr., Lei, Zy. et al. Safety and efficacy of Thymosin α1 in the treatment of hepatitis B virus-related acute-on-chronic liver failure: a randomized controlled trial. Hepatol Int 16, 775–788 (2022). https://doi.org/10.1007/s12072-022-10335-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10335-6