Abstract
Background and aims
We aimed to compare the longitudinal changes in estimated glomerular filtration rate (eGFR) in chronic hepatitis B (CHB) patients treated with entecavir (ETV) vs. tenofovir disoproxil fumarate (TDF).
Methods
This is a retrospective study of 6189 adult treatment-naïve CHB patients initiated therapy with TDF (n = 2482) or ETV (n = 3707) at 25 international centers using multivariable generalized linear modeling (GLM) to determine mean eGFR (mL/min/1.73 m2) and Kaplan–Meier method to estimate incidence of renal impairment (≥ 1 chronic kidney disease [CKD] stage worsening). We also examined above renal changes in matched ETV and TDF patients (via propensity score matching [PSM] on age, sex, diabetes mellitus [DM], hypertension [HTN], cirrhosis, baseline eGFR, and follow-up duration).
Results
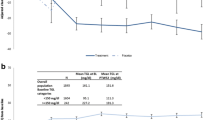
In the overall cohort (mean age 49.7 years, 66.2% male), the baseline eGFR was higher for TDF vs. ETV group (75.9 vs. 74.0, p = 0.009). PSM yielded 1871 pairs of ETV or TDF patients with baseline eGFR ≥ 60 and 520 pairs for the eGFR < 60 group. GLM analysis of the overall (unmatched) cohort and PSM cohorts revealed lower adjusted mean eGFRs in TDF (vs. ETV) patients (all p < 0.01) during 10 years of follow-up. Among PSM eGFR ≥ 60 patients, the 5-year cumulative incidences of renal impairment were 42.64% for ETV and 48.03% for TDF (p = 0.0023). In multivariable Cox regression, TDF vs. ETV (adjusted HR 1.26, 95% CI 1.11–1.43) was associated with higher risk of worsening renal function.
Conclusion
Over the 10-year study follow-up, compared to ETV, TDF was associated with a lower mean eGFR and higher incidence of renal impairment.



Similar content being viewed by others
Availability of data and materials
Data available within the article or its supplementary materials.
Code availability
Not applicable.
Abbreviations
- ALT:
-
Alanine aminotransferase
- CHB:
-
Chronic hepatitis B
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- DM:
-
Diabetes mellitus
- EASL:
-
The European Association for the Study of the Liver
- eGFR:
-
Estimated glomerular filtration rate
- ETV:
-
Entecavir
- HCC:
-
Hepatocellular carcinoma
- HTN:
-
Hypertension
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- NA:
-
Nucleos(t)ide analogs
- PSM:
-
Propensity score matching
- TAF:
-
Tenofovir alafenamide
- TDF:
-
Tenofovir disoproxil fumarate
References
Fabrizi F, Donato FM, Messa P. Association between hepatitis B virus and chronic kidney disease: a systematic review and meta-analysis. Ann Hepatol. 2017;16:21–47
Ning L, Lin W, Hu X, et al. Prevalence of chronic kidney disease in patients with chronic hepatitis B: a cross-sectional survey. J Viral Hepat. 2017;24:1043–1051
Mauss S, Berger F, Filmann N, et al. Effect of HBV polymerase inhibitors on renal function in patients with chronic hepatitis B. J Hepatol. 2011;55:1235–1240
Hong YS, Ryu S, Chang Y, et al. Hepatitis B virus infection and development of chronic kidney disease: a cohort study. BMC Nephrol. 2018;19:353
Chen YC, Su YC, Li CY, et al. A nationwide cohort study suggests chronic hepatitis B virus infection increases the risk of end-stage renal disease among patients in Taiwan. Kidney Int. 2015;87:1030–1038
Ly KN, Xing J, Klevens RM, et al. Causes of death and characteristics of decedents with viral hepatitis, United States, 2010. Clin Infect Dis. 2014;58:40–49
Rajbhandari R, Danford CJ, Chung RT, et al. HBV infection is associated with greater mortality in hospitalised patients compared to HCV infection or alcoholic liver disease. Aliment Pharmacol Ther. 2015;41:928–938
Qi X, Wang JY, Mao RC, et al. Impact of nucleos(t)ide analogues on the estimated glomerular filtration rate in patients with chronic hepatitis B: a prospective cohort study in China. J Viral Hepat. 2015;22:46–54
Chan HL, Shaikh J, Gupta S, et al. Renal function in nucleos(t)ide analog-treated patients with chronic hepatitis B: a systematic literature review and network meta-analysis. Adv Ther. 2016;33:862–875
Han Y, Zeng A, Liao H, et al. The efficacy and safety comparison between tenofovir and entecavir in treatment of chronic hepatitis B and HBV related cirrhosis: a systematic review and meta-analysis. Int Immunopharmacol. 2017;42:168–175
Tsai MC, Chen CH, Tseng PL, et al. Comparison of renal safety and efficacy of telbivudine, entecavir and tenofovir treatment in chronic hepatitis B patients: real world experience. Clin Microbiol Infect. 2016;22:951 e1-957 e7
Izzedine H, Launay-Vacher V, Deray G. Antiviral drug-induced nephrotoxicity. Am J Kidney Dis. 2005;45:804–817
Tanji N, Tanji K, Kambham N, et al. Adefovir nephrotoxicity: possible role of mitochondrial DNA depletion. Hum Pathol. 2001;32:734–740
Perazella MA. Tenofovir-induced kidney disease: an acquired renal tubular mitochondriopathy. Kidney Int. 2010;78:1060–1063
Kohler JJ, Hosseini SH, Hoying-Brandt A, et al. Tenofovir renal toxicity targets mitochondria of renal proximal tubules. Lab Invest. 2009;89:513–519
Lee HY, Oh H, Park CH, et al. Comparison of renal safety of tenofovir and entecavir in patients with chronic hepatitis B: Systematic review with meta-analysis. World J Gastroenterol. 2019;25:2961–2972
Rodriguez-Novoa S, Garcia-Samaniego J, Prieto M, et al. Altered underlying renal tubular function in patients with chronic hepatitis b receiving nucleos(t)ide analogs in a real-world setting: the MENTE study. J Clin Gastroenterol. 2016;50:779–789
Trinh S, Le AK, Chang ET, et al. Changes in renal function in patients with chronic HBV infection treated with tenofovir disoproxil fumarate vs entecavir. Clin Gastroenterol Hepatol. 2019;17:948-956 e1
Nguyen MH, Lim JK, Burak Ozbay A, et al. Advancing age and comorbidity in a US insured population-based cohort of patients with chronic hepatitis B. Hepatology. 2019;69:959–973
Wong GL, Wong VW, Yuen BW, et al. An aging population of chronic hepatitis B with increasing comorbidities: a territory-wide study from 2000 to 2017. Hepatology. 2020;71:444–455
Weinstein JR, Anderson S. The aging kidney: physiological changes. Adv Chronic Kidney Dis. 2010;17:302–307
Vu V, Trinh S, Le A, et al. Hepatitis B and renal function: a matched study comparing non-hepatitis B, untreated, treated and cirrhotic hepatitis patients. Liver Int. 2019;39:655–666
Amarapurkar DN, Dhawan P, Kalro RH. Role of routine estimation of creatinine clearance in patients with liver cirrhosis. Indian J Gastroenterol. 1994;13:79–82
Gines P, Schrier RW. Renal failure in cirrhosis. N Engl J Med. 2009;361:1279–1290
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL. Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;2017(67):370–398
Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599
Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva, 2015. https://www.who.int/publications/i/item/9789241549059
Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612
KDIGO. Clinical practice guideline update for the diagnosis, evaluation, prevention and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2017;2017(7):1–59
Drug full prescribing information for Viread. The Food and Drug Administration, 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022577lbl.pdf
Mak LY, Seto WK, Lai CL, et al. DNA polymerase inhibitors for treating hepatitis B: a safety evaluation. Expert Opin Drug Saf. 2016;15:383–392
Buti M, Riveiro-Barciela M, Esteban R. Tenofovir alafenamide fumarate: a new tenofovir prodrug for the treatment of chronic hepatitis b infection. J Infect Dis. 2017;216:S792–S796
Lampertico P, Buti M, Fung S, et al. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in virologically suppressed patients with chronic hepatitis B: a randomised, double-blind, phase 3, multicentre non-inferiority study. Lancet Gastroenterol Hepatol. 2020;5:441–453
Toyoda H, Leong J, Landis C, et al. Treatment and renal outcomes up to 96 weeks after tenofovir alafenamide switch from tenofovir disoproxil fumarate in routine practice. Hepatology. 2021;74:656–666
Peralta CA, Katz R, DeBoer I, et al. Racial and ethnic differences in kidney function decline among persons without chronic kidney disease. J Am Soc Nephrol. 2011;22:1327–1334
Funding
None.
Author information
Authors and Affiliations
Contributions
Study concept: MHN. Study supervision: MFY and MHN. Study design: LYM, JH, MFY, MHN. Data analysis: JH and MHN. Drafting of the article: LYM, JH, MFY, MHN. Data collection, data interpretation, review and/or revision of the manuscript: all authors. All authors identified have critically reviewed the paper and approve the final version of this paper, including the authorship statement.
Corresponding authors
Ethics declarations
Conflict of interest
CYP: Consulting/ Advisory board member: Abbvie, Bristol Myers Squibb, Gilead Sciences, Roche. DQH: Research grant: Exxon Mobil-NUS Fellowship, NMRC Research Training Fellowship. HT: Research grant: Gilead Sciences, Intercept, Target; Consulting/ advisory board: Gilead Sciences; Speaker fees: Gilead Sciences; Stock ownership: Gilead Sciences. GLHW: Research grant: Gilead Sciences; Consulting/ advisory board: Gilead Sciences, Janssen; Speaker fees: Abbott, Abbvie, Bristol Myers Squibb, Gilead Sciences. DHL: Research grant: Bristol Myers Squibb Korea, Gilead Sciences (Korea), Janssen Korea, Korea Pharma. EO: Speaker fees: Gilead Sciences. CYD: Speaker fees: Abbvie, Merck Sharp and Dohme, Gilead Sciences, Roche, Bristol Myers Squibb. WLC: Consulting: Gilead Sciences, Abbvie, Bristol Myers Squibb, Merck Sharp and Dohme, PharmaEssentia; Speaker fees: Gilead Sciences, Abbvie, Bristol Myers Squibb, Merck Sharp and Dohme, PharmaEssentia. MLY: Research grant: Abbott, Bristol Myers Squibb, Gilead Sciences, Merck Sharp and Dohme; Consulting: Abbvie, Abbott, Ascletis, Bristol Myers Squibb, Gilead Sciences, Merck Sharp and Dohme, Roche; Speaker fees: Abbvie, Abbott, Bristol Myers Squibb, Gilead Sciences, Merck Sharp and Dohme, IPSEN. MFY: Research funding: Assembly Biosciences, Arrowhead Pharmaceuticals, Bristol Myer Squibb, Fujirebio Incorporation, Gilead Sciences, Merck Sharp and Dohme, Springbank Pharmaceuticals, Sysmex Corporation; advisory board member: Abbvie, Arbutus Biopharma, Assembly Biosciences, Bristol Myer Squibb, Dicerna Pharmaceuticals, GlaxoSmithKline, Gilead Sciences, Janssen, Merck Sharp and Dohme, Clear B Therapeutics, Springbank Pharmaceuticals. MHN: Research grant: Gilead, Vir; Consulting/advisory board: Novartis, Spring Bank, Janssen, Gilead, Exact Sciences, Eli Lilly. All other authors have disclosed no personal conflict of interests in regards to the content of this paper.
Ethics approval
The study was conducted in accordance with the ethics principles of the Declaration of Helsinki in 1975, as revised in 2008, and was approved by the Institutional Review Board of Stanford University and at each participating institution.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mak, LY., Hoang, J., Jun, D.W. et al. Longitudinal renal changes in chronic hepatitis B patients treated with entecavir versus TDF: a REAL-B study. Hepatol Int 16, 48–58 (2022). https://doi.org/10.1007/s12072-021-10271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10271-x