Abstract
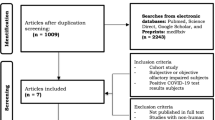
Recently acquired olfactory dysfunction (OD) has emerged as one of hallmark manifestations of the novel Corona virus disease (COVID-19), but the evolution of its spontaneous recovery has remained inconclusive, with reports of persistence of OD beyond six months of onset. We undertook this systematic review and meta-analysis with a view to generating a pooled recovery rate of COVID-19 associated olfactory dysfunctions and attempt to examine the predictors of olfactory recovery. Systematic review and meta-analysis. A systematic search of Scopus, Google Scholar, and PubMed data bases, comprising all longitudinal studies reporting the trajectory of COVID-19 related OD was carried out. The pooled recovery rate was estimated with random-effects model, and the potential heterogeneity of the subgroup sources was analyzed using meta-regression test. After the PRISMA selection process 28 studies from 16 countries were included, with a total of 5,175 OD patients, among 11,948 COVID-19 cases. The estimated global pooled recovery rate of OD was 82.7% (95% CI, 77.46%-88.04%), with a pooled median duration of OD of 11.6 days. Only 2 out of 28 studies had recovery data beyond a period of 2 months. But no significant difference was found in the recovery rate regarding the length of follow up (P = 0.840). Studies that conducted objective olfactory assessments showed significant higher recovery rate than those with subjective assessments (P = 0.001). Although ten studies (36%) reported > 90% recovery, nine studies (32%) documented persistence of OD in > 25% of their patients. Five out of 6 studies showed that hyposmia tended to show complete recovery than anosmia. Age, co-morbidities, and intra-nasal treatments had no effects. Test of homogeneity between subgroups using the Cochran’s Q test was not significant (Q = 0.69, P = 0.40). Our meta-analysis revealed high rate of early and medium term recovery of COVID-19 related OD. However, it also showed disturbing rates of persistence of OD. Anosmia tended to be predictive of residual OD than hyposmia. Age, co-morbidities, intra-nasal corticosteroid and decongestants, had no effects on OD recovery.



Similar content being viewed by others
References
World Health Organization Coronavirus disease dashboard, global situation. https://covid19.who.int/. Accessed 20 Jan 2021
Lechien JR, Chiesa-Estomba CM, Beckers E, Mustin V, Ducarme M, Journe F et al (2021) Prevalence and 6-month recovery of olfactory dysfunction: a multicentre study of 1363 COVID-19 patients. J Intern Med 290:451–461
Ibekwe TS, Fasunla AJ, Orimadegun AE (2020) Systematic review and meta-analysis of smell and taste disorders in COVID-19. OTO Open. https://doi.org/10.1177/2473974X20957975
Hannum ME, Ramirez VA, Lipson SJ, Herriman RD, Toskala AK, Lin C et al (2020) Objective sensory testing methods reveal a higher prevalence of olfactory loss in COVID-19 positive patients compared to subjective methods: a systematic review and meta-analysis. Chem Sens 45:865–874. https://doi.org/10.1093/chemse/bjaa064
Saniasiaya J, Islam MA, Abdullah B (2020) Prevalence of olfactory dysfunction in coronavirus disease 2019 (COVID-19): a meta-analysis of 27,492 patients. Laryngoscope. https://doi.org/10.1002/lary.29286
Centres for Disease Control and prevention (2021) Coronavirus self-checker. https://www.cdc.gov/coronavirus/2019-ncov/symptomstesting/symptoms.html. Accessed 20 Jan 2021
World Health Organization (2020) Health topic: coronavirus. https://www.who.int/health-topics/coronavirus#tab=tab_3. Accessed 20 Jan 2022
Ardestani SHS, Ardehali MM, Anari MR, Rahmaty B, Erfanian R, Akbari M et al (2021) The coronavirus disease 2019: the prevalence, prognosis, and recovery from olfactory dysfunction (OD). Acta Otolaryngol 141(2):171–180. https://doi.org/10.1080/00016489.2020.183639
Ramasamy K, Saniasiaya J, Gani NA (2021) Olfactory and gustatory dysfunctions as a clinical manifestation of coronavirus disease 2019 in a Malaysian tertiary center. Ann Otol Rhinol Laryngol 130:513–519. https://doi.org/10.1177/0003489420963165
Ugurlu BN, Akdogan O, Yilmaz YA, Yapar D, Ugurlu GA, Yerlikaya HS et al (2021) Quantitative evaluation and progress of olfactory dysfunction in COVID-19. Eur Arch Otorhinolaryngol 1:1–7. https://doi.org/10.1007/s00405-020-06516-4
Abdelalim AA, Mohamady AA, Elsayed RA, Elawady MA, Ghallab AF (2021) Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: A randomized controlled trial. Am J Otolaryngol 42(2):102884. https://doi.org/10.1016/j.amjoto.2020.102884
Iberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Klopfenstein T, Kadiane-Oussou NJ, Toko L, Royer P-Y, Lepiller Q, Gendrin V et al (2020) Features of anosmia in COVID-19. Med Mal Infect 50:436–439
Chung TW, Sridhar S, Zhang AJ, Chan K, Li H, Wong FK et al (2020) Olfactory dysfunction in Coronavirus disease 2019 patients: observational cohort study and systematic review. Open Forum Infect Dis 7(6):offaa99. https://doi.org/10.1093/ofid/ofaa199
Galván-Tejada CE, Herrera-García CF, Godina-González S, Villagrana-Bañuelos KE, Amaro JD, Herrera-García K et al (2020) Persistence of COVID-19 symptoms after recovery in Mexican population. Int J Environ Res Public Health 17(24):9367. https://doi.org/10.3390/ijerph17249367
Chiesa-Estomba CM, Lechien JR, Radulesco T, Michel J, Sowerby LJ, Hopkins C, Saussez S (2020) Patterns of smell recovery in 751 patients affected by the COVID-19 outbreak. Eur J Neurol 27(11):2318–2321. https://doi.org/10.1111/ene.14440
Lee Y, Min P, Lee S, Kim SW (2020) Prevalence and duration of acute loss of smell or taste in COVID-19patients. J Korean Med Sci 35(18):e174. https://doi.org/10.3346/jkms.2020.35.e174
Chary E, Carsuzaa F, Trijolet J, Capitaine A, Roncato-Saberan M, Fouet K et al (2020) Prevalence and recovery from olfactory and gustatory dysfunctions in Covid-19 infection: a prospective multicenter study. Am J Rhinol Allergy 34(5):686–693. https://doi.org/10.1177/1945892420930954
Lechien JR, Journe F, Hans S, Chiesa-Estomba CM, Mustin V, Beckers E et al (2020) Severity of anosmia as an early symptom of COVID-19 Infection may predict lasting loss of smell. Front Med 7:582802. https://doi.org/10.3389/fmed/582802
Printza A, Katotomichelakis M, Valsamidis K, Metallidis S, Panagopoulos P, Panopoulou M et al (2021) Smell and taste loss recovery time in COVID-19 patients and disease severity. J Clin Med 10:966. https://doi.org/10.3390/jcm10050966
Vaira LA, Hopkins C, Petrocelli M, Lechien JR, Chiesa-Estomba CM, Salzano G et al (2020) Smell and tasterecovery in coronavirus disease 2019patients: a 60-dayobjective and prospective study. J Laryngol Otol 134(8):703–709. https://doi.org/10.1017/S0022215120001826
Loftus PA, Roland LT, Gurrola JG, Cheung SW, Chang JL (2020) Temporal profile of olfactory dysfunction in COVID-19. OTO Open. https://doi.org/10.1177/2473974X20978133
Altundag A, Saatci O, Sanli DE, Duz OA, Sanli AN, Olmuscelik O et al (2021) The temporal course of COVID-19anosmia and relation to other clinical symptoms. Eur Arch Otorhinolaryngol 278(6):1891–1897. https://doi.org/10.1007/s00405-020-06496-5
Beltrán-Corbellini A, Chico-García JL, Martínez-Poles J, Rodríguez-Jorge F, Natera-Villalba E, Gómez-Corral J et al (2020) Acute-onset smell and taste disorders in the context of COVID-19: a pilot multicentre polymerase chain reaction based case–control study. Eur J Neurol 27(9):1738–1741. https://doi.org/10.1111/ene.14273
Neto DB, Fornazieri MA, Dib C, Di Francesco RC, Doty RL, Voegels RL et al (2021) Chemosensory dysfunction in COVID-19: prevalences, recovery rates, and clinical associations on a large Brazilian sample. Otolaryngol Head Neck Surg 164(3):512–518. https://doi.org/10.1177/0194599820954825
Paolo G (2020) Does COVID-19 cause permanent damage to olfactory and gustatory function? Med Hypotheses 143:110086. https://doi.org/10.1016/j.mehy.2020.110086
Amer MA, Elsherif HS, Abdel-Hamid AS, Elzayat S (2020) Early recovery patterns of olfactory disorders in COVID-19 patients; a clinical cohort study. Am J Otolaryngol 41(6):102725. https://doi.org/10.1016/j.amjoto.2020.102725
Gupta V, Rajanna LB, Upadhyay K, Bhatia R, Reddy NM, Malik D et al (2021) Olfactory and gustatory dysfunction in COVID-19 patients from Northern India: a cross-sectional observational study. Indian J Otolaryngol Head Neck Surg 73(2):218–225
Sahoo PR, Sahu M, Surapaneni PS, Maiti A, Vankamamidi R, Panda N et al (2021) Evolution of olfactory and gustatory dysfunctions in COVID-19 patients in India. Eur Arch Otorhinolaryngol 278:2875–2881. https://doi.org/10.1007/s00405-020-06563
Gorzkowski V, Bevilacqua S, Charmillon A, Jankowski R, Gallet P, Rumeau C (2020) Evolution of olfactory disorders in COVID-19 patients. Laryngoscope 130(11):2667–2673. https://doi.org/10.1002/lary.28957
Iannuzzi L, Salzo AE, Angarano G, Palmieri VO, Portincasa P, Saracino A et al (2020) Gaining back what is lost: Recovering the sense of smell in mild to moderate patient safter COVID-19. Chem Sens 45(9):875–8819. https://doi.org/10.1093/chemse/bjaa066
Kosugi EM, Lavinsky J, Romano FR, Fornazieri MA, Luz-Matsumoto GR, Lessa MM et al (2020) Incomplete and laterecovery of suddenolfactorydysfunction in COVID-19. Braz J Otorhinolaryngol 86(4):490–496. https://doi.org/10.1016/j.bjorl.2020.05.001
Patel A, Charani E, Ariyanayagam D, Abdulaal A, Denny SJ, Mughal N et al (2020) New-onsetanosmia and ageusia in adultpatientsdiagnosed with SARS-CoV-2 infection. Clin Microbiol Infect 26(9):1236–1241. https://doi.org/10.1016/j.cmi.2020.05.026
Karthikeyan P, Sivanand N, Vijayan N, Latheef MN (2021) A clinical study of smell disorders in COVID-19 patients in a tertiary care hospital in pondicherry: a cross sectional study. Indian J Otolaryngol Head Neck Surg 13:1–6. https://doi.org/10.1007/s12070-021-02499-8
Jain A, Kumar L, Kaur J, Baisla T, Goyal P, Pandey AK et al (2020) Olfactory and taste dysfunction in coronavirus disease 2019 patients: its prevalence and outcomes. J Laryngol Otol. https://doi.org/10.1017/S0022215120002467
Boscutti A, Delvecchio G, Pigoni A, Cereda G, Ciappolino V, Bellani M et al (2021) Olfactory and gustatory dysfunctions in SARS-CoV-2 infection: a systematic review. Brain Behav Immun Health. https://doi.org/10.1016/j.bbih.2021.100268
Brann D, Tsukahara T, Weinreb C, Lipovsek M, Von Den Berge K, Gong B et al (2020) Non-neural expression of SARS-CoV-2 entry genes in the olfactory epithelium suggests mechanisms underlying COVID-19 associated anosmia. Sci Adv. https://doi.org/10.1126/sciadv.abc5801
Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 203(2):631–7
Sungnak W, Huang N, Bécavin C (2020) SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med 26:681–687. https://doi.org/10.1038/s41591-020-0868-6
Alipoor SD, Mortaz E, Varahram M, Garssen J, Adcock IM (2021) The immunopathogenesis of neuroinvasive lesions of SARS-CoV-2 infection in COVID-19 patients. Front Neurol 12:697079. https://doi.org/10.3389/fneur.697079
Dubé M, Coupanec LA, Wong AHM, Rini JM, Desforges M, Talbot PJ (2018) Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol. https://doi.org/10.1128/JVI.00404-18
Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S (2018) Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol 82:7264–7275
Lechien JR, Chiesa-Estomba CM, Hans S, Saussez S (2021) Pathophysiologicalmechanisms and management of patients with long-time anosmiarelated to COVID-19. J Intern Med 290(2):464–465. https://doi.org/10.1111/joim.13257
Walker A, Pottinger G, Scott A, Hopkins C (2020) Anosmia and loss of smell in the era of covid-19. BMJ 370:m2808
Isidori AM, Arnaldi G, Boscaro M, Falorni A, Giordano R et al (2020) COVID-19 infection and glucocorticoids: update from the Italian society of endocrinology expert opinion on steroid replacement in adrenal insufficiency. J Endocrinol Invest. https://doi.org/10.1007/s40618-020-01266-w
Bousquet J, Akdis C, Jutel M (2020) Intranasal corticosteroids in allergic rhinitis in COVID-19 infected patients: an ARIA-EAACI statement. Allergy 75(10):2440–2444. https://doi.org/10.1111/all.14302
Funding
No funding was received for conducting this study or to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Orji, F.T., Akpeh, J.O. & Okolugbo, N.E. Recovery Patterns of COVID-19 Related Smell Disorders: An Analysis of the Available Evidence. Indian J Otolaryngol Head Neck Surg 75, 4179–4189 (2023). https://doi.org/10.1007/s12070-023-04005-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04005-8