Abstract
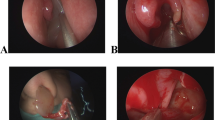
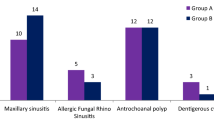
Aims: The objective of this study is to assess the effectiveness of the combined middle and inferior meatal antrostomy (MIMA) in management of patients with maxillary fungal sinusitis. Material and Methods: Design: retrospective cross sectional study. Setting and subjects: From September 2018 to March 2021, fifty-five patients with non-invasive maxillary fungal sinusitis, who underwent transnasal endoscopic combined MIMA. Methods: The study compared patients’ pre- and post-operative subjective symptoms, including nasal obstruction, discharge, facial pain or pressure, halitosis, anosmia, and other non-specific symptoms. Endoscopic characteristics of recurrent fungal maxillary sinusitis and postoperative complications were also observed. Closure of the IMA site was evaluated at three and six months post-surgery and patients were categorized into three groups based on closure degree. Results: All clinical symptoms, including nasal discharge, nasal obstruction, nasal pruritus, anosmia, halitosis, sneezing, facial pain, ophthalmic and otologic symptoms, were resolved over six months after combined MIMA in majority of cases (94 − 100%). After three and six months, the postoperative endoscopic evaluation revealed recurrent fungal maxillary sinusitis in 1.8% and 5.4% of cases, respectively. Partial stenosis of the inferior antrostomy was observed in 7.2% and 16% of cases, while complete stenosis was noted in 3.6% and 7.2% of cases after three months and six months. Conclusions: The combined MIMA is effective and has better outcomes than the medial meatal antrostomy approach alone without additional operative time.



Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this article.
References
Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, Kita H, Marple B, Panda N, Vlaminck S, Kauffmann-Lacroix C et al (2009) Fungal rhinosinusitis. Laryngoscope 119:1809–1818
Deshazo RD (1998) Fungal sinusitis. Am J Med Sci 316:39–45
Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Klossek JM (2006) Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989–2002. Med Mycol 44:61–67
Grosjean P, Weber R (2007) Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol 264:461–470
Pagella F, Matti E, De Bernardi F, Semino L, Cavanna C, Marone P, Farina C, Castelnuovo P (2007) Paranasal sinus fungus ball: diagnosis and management. Mycoses 50:451–456
Nomura K, Asaka D, Nakayama T, Okushi T, Matsuwaki Y, Yoshimura T, Yoshikawa M, Otori N, Kobayashi T, Moriyama H (2013) Sinus fungus ball in the japanese population: clinical and imaging characteristics of 104 cases. Int J Otolaryngol 2013:731640
Liu X, Liu C, Wei H, He S, Dong S, Zhou B, Zhang L, Li Y (2020) A retrospective analysis of 1,717 paranasal sinus fungus ball cases from 2008 to 2017. Laryngoscope 130:75–79
Kim JS, So SS, Kwon SH (2017) The increasing incidence of paranasal sinus fungus ball: a retrospective cohort study in two hundred forty-five patients for fifteen years. Clin Otolaryngol 42:175–179
Sonbay Yılmaz ND, Afyoncu C, Ensari N, Yıldız M, Gür ÖE (2021) The effect of the mother’s participation in therapy on children with vocal fold nodules. Annals of Otology Rhinology & Laryngology 130:1263–1267
Sawatsubashi M, Murakami D, Umezaki T, Komune S (2015) Endonasal endoscopic surgery with combined middle and inferior meatal antrostomies for fungal maxillary sinusitis. J Laryngol Otol 129(Suppl 2):S52–55
Choi Y, Kim B-H, Kang S-H, Yu MS (2019) Feasibility of minimal Inferior Meatal Antrostomy and Fiber-Optic Sinus exam for fungal sinusitis. Am J Rhinol Allergy 33:634–639
Klossek J-M, Serrano E, Péloquin L, Percodani J, Fontanel J-P, Pessey J-J (1997) Functional endoscopic sinus surgery and 109 mycetomas of Paranasal Sinuses. Laryngoscope 107:112–117
Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Karkas A, Klossek JM (2005) Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology 43:34–39
Albu S, Gocea A, Necula S (2011) Simultaneous inferior and middle meatus antrostomies in the treatment of the severely diseased maxillary sinus. Am J Rhinol Allergy 25:e80–e85
Sawatsubashi M (2018) Endoscopic Surgical Procedures for Fungal Maxillary Sinusitis: how to do it, a review. Int J Otolaryngol Head Neck Surg 07:287–297
Ding L, Na g, Lou Z (2022) Extended middle meatal antrostomy via antidromic extended medial wall for the treatment of fungal maxillary sinusitis. BMC Surg 22:287
Lund VJ (1988) Inferior meatal antrostomy. Fundamental considerations of design and function. J Laryngol Otol Suppl 15:1–18
Tani A, Tada Y, Miura T, Suzuki T, Nomoto M, Saijo H, Ono M, Ogawa H, Omori K (2011) Surgical Approach for Maxillary Fungal Sinusitis. Nihon Bika Gakkai Kaishi (Japanese Journal of Rhinology) 50:26–30
Suzuki M, Matsumoto T, Yokota M, Toyoda K, Nakamura Y (2019) Transnasal inferior meatal antrostomy with a mucosal flap for post-caldwell-luc mucoceles in the maxillary sinus. J Laryngol Otol 133:674–677
Acknowledgements
None.
Funding
No funding was used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
Ethical committee approved the study proposal.
Informed Consent
Informed Consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van Ngo, C., Nguyen, H., Aklinski, J. et al. The Combined Middle and Inferior Antrostomy for Fungal Maxillary Sinusitis Treatment. Indian J Otolaryngol Head Neck Surg 75, 2850–2855 (2023). https://doi.org/10.1007/s12070-023-03863-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03863-6