Abstract
The World Health Organization announced on March 11, 2020 that COVID-19 could become a pandemic. COVID-19 is a contagious disease caused by the coronavirus that causes severe acute respiratory syndrome (SARS-CoV-2). Viruses usually enter the body through the mouth or nose. The virus then enters the alveoli, which are small air sacs inside the lungs. Cough, fatigue, fever, shortness of breath or breathing difficulties, and loss of smell and taste are all symptoms of COVID-19. Anosmia, also known as smell blindness, is a condition in which the ability to detect one or more smells is lost. Olfaction uses chemoreceptors to create signals that are processed in the brain and form the sense of smell in anosmia. Anosmia is recognised as a COVID-19 symptom in many countries, and some have developed "smell tests" as potential screening tools. The first level of screening, which is currently used in India, is primarily based on temperature and can result in false positives and negatives (fever as a symptom has not yet been developed although infection). One of the methods for detecting COVID-19 is an intermediate level of screening based on assessing an olfactory function, depending on the usage. This paper provides an overview of COVID-19 and its effects on the human body, as well as an overview of anosmia and how it contributes to one of the symptoms of COVID-19.
Similar content being viewed by others
Coronavirus Disease 2019 (COVID-19)
COVID 19 is a contagious disease caused by the coronavirus that causes severe acute respiratory syndrome (SARS-CoV-2) [1]. The Coronavirus Disease 2019 (COVID-19) pandemic began in Wuhan, Hubei Province, China, in December 2019 and quickly spread throughout China and then around the world. On February 12, 2020, the World Health Organization (WHO) designated the disease caused by the novel coronavirus as COVID-19.
Symptoms of COVID-19
Fever, cough, dyspnoea, sputum production, myalgia, arthralgia, headache, diarrhoea, rhinorrhoea, and sore throat, as well as new loss of smell or taste, according to the Centers for Disease Control and Prevention (CDC). Novel coronaviruses have an incubation period of two to fourteen days.
According to data from the Impact of Pre-existing Comorbidities and Therapeutic Interventions on COVID-19 and the Centers for Disease Control and Prevention Coronavirus disease (CDC) [2], Fig. 1 depicts the percentage distribution of different COVID-19 [3] symptoms.
Infection and Transmission
Coronavirus is an RNA virus of various types. 229E (alpha coronavirus), NL63 (alpha coronavirus), OC43 (beta coronavirus), HKU1 (beta coronavirus), MERS-CoV(the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS), SARS-CoV(the beta coronavirus that causes severe acute respiratory syndrome, or SARS), SARS-CoV-2(the novel coronavirus that causes coronavirus). The virus, enters the body through the mouth or nose and can affect both the upper and lower respiratory tracts (sinuses, nose, and throat). [4] The virus then travels to the air sacs (alveoli) in our lungs. COVID 19 has the greatest impact on the lungs because the virus enters host cells through the enzyme angiotensin-converting enzyme 2 (ACE2), which is abundant in type II alveolar cells [5]. Inside the alveoli, the virus connects to ACE2 receptors with its distinctive spike protein (peplomer), a special surface glycoprotein S1, and then enters the host cell. The density of ACE2 receptors in each tissue correlates with the severity of the disease in that tissue, with alveoli having the most ACE2 receptors. Some believe that lowering ACE2 activity is protective, while others believe that increasing ACE2 with angiotensin II receptor blocker medication might be protective. ACE2 is a functional SARS-CoV-2 receptor, and its distribution and expression in the nervous system suggest that SARS-CoV-2 can cause neurological manifestations through direct or indirect pathways. [6] COVID-19 is no exception to the rule that any virus's primary genetic programming is to replicate itself. Once the virus RNA enters a cell, new copies are made and the cell is killed, releasing new viruses into the alveolus. The viral infection could cause increased coagulation, cytokine storm, septic shock, multi-organ failure, and death, in addition to lung involvement and acute respiratory distress syndrome (ARDS). Respiratory failure may develop as the alveolar disease progresses, and death may result. [5] COVID-19 is a new disease, and much of the information about how it spreads is still being researched. It is more easily transmitted between people than influenza, but not as easily as measles or other diseases.
Olfactory Physiology
Figure 2 depicts the physiology of olfaction. Olfaction is based on the generation of chemical signals by chemoreceptors, which are then processed by the brain to produce the sense of smell. Olfaction, or the sense of smell, is the process of creating a perception of a smell. [7] A signal is sent through the olfactory system when an odour binds to a receptor in the nose.
Odorant molecules released by a substance (such as the fragrance of a flower) stimulate special nerve cells called olfactory cells [6], which then bind to odorant receptors on the cilia of olfactory sensory neurones in the olfactory epithelium of the superior nasal cavity. The olfactory sensory neurones (OSNs), sustentacular cells, microvillar cells, olfactory (Bowman's) gland duct cells, and basal cells [15] make up this epithelial layer. OSNs are bipolar neurones with dendrites that project into the nasal cavity and form synapses in the olfactory bulb on the ipsilateral forebrain's ventral anterior aspect. Each dendritic knob of an OSN protrudes 10–30 cilia into the mucus layer. Each OSN expresses a unique OR type, and the axons of all OR-specific OSNs project to the glomeruli, where they synapse with mitral and tufted cells in the olfactory bulb [8].
Mitral and tufted cells, for example, are second-order olfactory neurones with axons that project to olfactory areas of the central nervous system (CNS). Primary olfactory brain structures include the anterior olfactory nucleus (AON), olfactory tubercle, piriform cortex (area 51), amygdala, and entorhinal cortex, while secondary olfactory brain structures include the hippocampus, hypothalamus, thalamus, orbitofrontal cortex, and insula [9]. Multimodal integration is critical for cognition and motor control, and this neural circuit feeds into it. According to a recent study, the AON uses hippocampus input to store olfactory memory. Loss of smell can be caused by any obstruction to these pathways, such as nasal congestion, nasal blockage, or nerve cell damage [6].
Anosmia
Causes and Impact of Anosmia
Anosmia, also known as smell blindness, is a condition in which one or more senses of smell are lost. Anosmia is a condition that can last for a short time or for a long time [9]. Allergies or a cold, for example, can irritate the nose's lining, resulting in temporary anosmia. Permanent loss of smell can occur as a result of more serious brain or nerve conditions, such as brain tumours or head trauma. Anosmia is a degenerative condition that affects people as they age. Anosmia is a condition that can have a significant impact on a person's quality of life, despite the fact that it is rarely fatal [9].
Because they are unable to fully taste foods, people with anosmia may lose interest in eating. As a result, weight loss or malnutrition may occur. It can also cause depression because it impairs one's ability to smell or taste pleasurable foods. Our sense of smell can have an impact on our taste buds. If we don't have a sense of smell, our taste buds can only detect a few flavours. Studies have linked OTD (olfactory / taste disorders) to COVID-19, leading to its inclusion as a symptom of COVID-19 in CDC [2, 10]. Mechanical barriers, such as allergic rhinitis, nasal masses, chronic rhinosinusitis, and nasal polyps, prevent odorants and receptors from coming into close proximity, resulting in conductive olfactory dysfunction. A combination of nasal airflow obstruction and mucosal oedema characterises this condition. Sensorineural disorders are caused by a failure of the olfactory receptors (ORs), olfactory neurones, and olfactory pathways up to the central nervous system (CNS) to process odorant stimuli (OB and olfactory brain areas). As a result, viral infections are the most common cause of sensorineural olfactory dysfunction.13. Headaches have been linked to anosmia [7].
Causes
According to a smattering of evidence, OD (olfactory dysfunction) is one of COVID-19's most common symptoms. During the COVID-19 pandemic [6], the symptoms of olfactory dysfunction drew the attention of otolaryngologists all over the world. Anosmia can be caused by a number of things, including nasal mucosa inflammation, nasal passage blockage, or temporal lobe destruction. Chronic mucosa changes in the lining of the paranasal sinus and the middle and superior turbinates cause inflammation. Chronic meningitis and neurosyphilis, which raise intracranial pressure over time, can cause it, as can ciliopathy due to primary ciliary dyskinesia in some cases. Another cause of permanent loss of smell due to damage to olfactory receptor neurones is the use of certain nasal sprays that cause nasal microcirculation vasoconstriction [9]. Anosmia is most commonly caused by nasal congestion caused by a cold, allergy, sinus infection, or poor air quality.
Other Anosmia Causes Include
Polyps in the nose, Surgery or trauma to the nose and smell nerves, exposure to toxic chemicals, certain medications, heart medications, and others, cocaine abuse, and old age, like vision and hearing, can weaken one's sense of smell. Between the ages of 30 and 60, the sense of smell is at its peak, and after that, it starts to fade. Radiation treatment for head and neck cancers, and certain medical conditions [5].
Brain or Nerve Damage
Inside the nose, there are numerous receptors that send information to the brain via nerves. If any part of this pathway is damaged, anosmia can occur. Old age, brain tumours, Huntington's disease, Alzheimer's disease, hormonal problems, an underactive thyroid, medications, including some antibiotics and high blood pressure medications, multiple sclerosis, Parkinson's disease, schizophrenia, diabetes, epilepsy, exposure to chemicals that burn the inside of your nose, brain surgery, brain or head injury, malnutrition and vitamin deficiencies, and long-term radiation therapy are just a few of the conditions that can cause damage. Due to a genetic condition, some people are born without a sense of smell [6].
Anosmia in COVID-19
Apoptosis as a Mechanism of Anosmia
As seen in influenza viral components trapped in apoptotic bodies that are later phagocytized by macrophages, apoptosis is a protective host response to viral replication. ORNs are neurones because they can self-renew every 40–120 days throughout their lives. For ORNs, regulated apoptosis is a normal part of their life cycle. People do not notice olfactory changes in permanently controlled apoptosis, but ORNs' large-scale apoptosis mechanism can result in a sudden loss of smell. Immune cells and cytokines are important regulators of apoptosis [12].
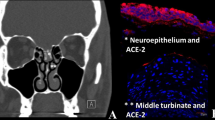
Role of ACE2 and TMPRSS2
Both ACE2 and (Type II transmembrane Serine Protease) TMPRSS2 are expressed by cells in the olfactory epithelium, a specialised tissue in the roof of the nasal cavity that houses olfactory sensory neurones and a variety of supporting cells and is responsible for odour detection. The spike protein is activated by TMPRSS2, which makes it easier for the SARS COV-2 virus to enter the body. ACE and its homolog ACE2 play a role in the synthesis of RAS bioactive components in COVID-19 (reticular activating system) [13].
Role of TNF in Anosmia
Toxic inflammatory factors (such as TNF- and IL-1) destroy the olfactory neuroepithlium, resulting in olfactory loss, particularly sensorineural olfactory loss. TNF- is a potent inflammatory mediator linked to a variety of cell types. TNF- has been shown to have an effect on olfactory neurone function. Local TNF-expression causes inflammatory infiltration, which can cause the olfactory submucosa to expand. As a result, the mechanism of anosmia in COVID-19 could be explained in this way. In patients with COVID-19, higher levels of the inflammatory cytokine TNF- were found in the olfactory epithelium, according to a study. TNF- and IL-1 are two cytokines that are involved in inflammatory diseases of the nasal mucosa and can be considered for future COVID-19 control and treatment strategies [14].
Involvement of Hypothalamus and Other Brain Areas
SARS-CoV-2 is transmitted retrogradely and spreads trans-synaptically from the nasal mucosa to higher brain regions such as the septal nuclei, entorhinal cortex, pre-pyriform cortex, amygdala, hippocampus, subiculum, thalamus, and frontal cortex via multiple projections. The virus can spread from the olfactory bulb to other parts of the brain, including the hippocampus, where it appears to spread via a trans-neuronal route before reaching the brainstem and spinal cord. These findings suggest that coronaviruses can enter the human CNS from the outside world via the olfactory nerve and OB neuro epithelium. The virus has been found in the brain and cerebrospinal fluid in clinical-pathological studies (CSF). Some studies have also shown SARS-CoV-2 RNA in brain post-mortem or in the CSF in patients with encephalopathy or encephalitis, but at very low levels [15].
Anosmia as a Marker of COVID-19 Infection
One of COVID-19's symptoms is anosmia. Anosmia has finally been recognised as a COVID-19 symptom in many countries, and some have even developed "smell tests" as potential screening tools.
Approximately 40% of people lose their sense of smell, have changes in how food tastes (dysgeusia), or have other problems with their normal smell and taste abilities. This symptom shows up early on in the illness. Younger people are more likely to have a problem with their sense of smell or taste, which is linked to a lower risk of medical complications. Although most people with COVID-19 do not have these symptoms, they are an uncommon symptom for other respiratory diseases, so they are used for symptom-based screening [7].
One of COVID-19's symptoms is anosmia. Several respiratory viruses can cause olfactory dysfunction after infection, which can lead to sensorineural damage. Because the olfactory bulb is an immunological organ that helps to prevent virus invasion, it also plays a role in host defence. COVID-19 produces an inflammatory product that causes olfactory loss while also interfering with viral spread into the central nervous system. In the central nervous system, olfactory receptors play a role as an alternative mode of SARS-CoV-2 entry into cells. Differences in the olfactory bulb due to sex and age may help to explain why some people are more susceptible to infection than others, as well as the role of age in disease transmission and severity. Finally, evaluation of the degree of functional impairment, central or peripheral may be useful tools to counteract COVID-19 [11].
In Wuhan, China, the first anosmia in COVID-19 patients was discovered on February 22, 2020. When the test was performed on 214 COVID-19 patients, the results were as follows: The central nervous system was affected in 53 patients (24.8%), with the most common symptoms being dizziness (36 patients [16.8%]), headache (28 patients [13.1 percent]), and impaired level of consciousness (28 patients [13.1 percent]) (16 patients [7.5 percent]). Patients with hypogeusia [(12 patients) (5.6 percent)] and hyposmia [(11 patients) (5.1 percent)] were affected by the peripheral nervous system [16].
There is new evidence for the loss of smell as a symptom of COVID-19 infection, according to ENT UK [17]. Anosmia can be caused by this in up to 40% of cases. Post-infectious loss is caused by viruses that cause the common cold, and over 200 viruses cause upper respiratory tract infections. Coronaviruses that have been previously identified are thought to account for 10–15% of cases. Significant numbers of patients with COVID-19 infection have developed anosmia/hyposmia, according to evidence from South Korea, China, and Italy. Anosmia has been reported in more than 2 out of every 3 confirmed cases in Germany. Anosmia was the most common presenting symptom in 30% of patients who tested positive in South Korea, where testing is more widespread. Furthermore, there have been an increasing number of reports of a significant increase in the number of anosmia patients. Iran has reported an increase in isolated anosmia cases, as have many other countries in the United States, France, and Northern Italy.
Many studies suggest that it predicts disease better than other well-known symptoms like fever and cough, but primary mechanisms for COVID-19 [18] patients' loss of smell are unknown. The olfactory cell types in the upper nasal cavity that are most vulnerable to infection by SARS-CoV-2 [8] have been identified by an international team of researchers led by Harvard Medical School neuroscientists.
Sensory neurones, which detect and transmit the sense of smell to the brain, are not among the cell types that are vulnerable. The findings point to nonneuronal cell infection as a possible cause of anosmia in COVID-19 patients, and they can help researchers better understand how the disease progresses [18].
Anosmia may occur in the majority of COVID-19 patients, though it is usually only temporary. COVID-19 patients are 27 times more likely to have smell loss, but only 2.2 to 2.6 times more likely to have a fever, cough, or respiratory difficulty, according to electronic health records [18]. COVID-19 anosmia may differ from anosmia caused by other viral infections, such as other coronaviruses, according to some studies [18].
COVID-19 patients recover their sense of smell much faster than anosmia caused by viral infections that directly damage olfactory sensory neurones, according to a study. Furthermore, many viruses cause temporary loss of smell by causing upper respiratory problems like a stuffy nose. However, some COVID-19 patients develop anosmia without any nasal obstruction [18].
Management for Diagnosis
Tests for Diagnosis of COVID-19
The WHO has published many testing protocols for this disease.
Screening Tests: Screening tests are used to identify people who are potentially contagious so that precautions can be taken to prevent further transmission [19] like temperature checks. rRT-PCR method: The real-time reverse transcription-polymerase chain reaction method of testing is the gold standard (rRT-PCR) [5]. rRT-PCR viral load and Anosmia: Patients with asymptomatic or mild SARS-CoV-2 infection and a higher viral load took longer to show negative qPCR results, according to some findings. As a result, a high qPCR value can be used as one of the diagnoses for COVID-19 early detection [20]. Rapid Antigen Tests: Rapid Antigen Tests are immunoassays that detect the presence of a specific viral antigen and are frequently used to diagnose respiratory pathogens. [21] TATA CRISPR Test: The Tata Group has announced the Tata CRISPR test, which was developed by the CSIR-IGIB 'Feluda' laboratory (Council of Scientific and Industrial Research-Institute of Genomics and Integrative Biology) The test has a sensitivity of 96 percent and specificity of 98 percent for detecting the coronavirus. The method used is an indigenously developed CRISPR technology for detecting the SARS-CoV-2 virus's genomic sequence [21].
Tests for Diagnosis of Anosmia
Smell Test
Doctors test a person's sense of smell by placing common fragrant substances (such as asafoetida, coffee bean, and clove oil) in his or her nostril. The smell is recognised by the individual. Using standardised commercial smell test kits [22], the sense of smell can also be tested more formally.
Smell Exercises
Along with many physiotherapy techniques smell exercises like, odour differentiation exercises, exercises in guessing and naming different odours, exercises in differentiating odour intensity, exercises in searching the source of smell can be done to increase sensitivity of smell [23].
Instrumental Techniques
It's difficult to quantify the loss of smell. Your doctor may order additional tests, such as CT (computed tomography) scans (which use X-rays), based on your current symptoms, examining your nose, performing a complete physical examination, and asking about your health history. A CT scan may be required to give the doctor a better view of the area). X-rays of the skull, MRI (magnetic resonance imaging) scans (which use radio waves), A nasal endoscopy is used to examine the inside of the nose [6].
Treatment of Anosmia
Medical Treatment
Treatment is determined by the underlying cause. If you lose your sense of smell as a result of a cold, allergy, or sinus infection, it usually goes away on its own after a few days. If the anosmia does not go away, you should see a doctor [8]. Sinus infections and mucous membrane irritation can be treated with nasal sprays, steam inhalation, antibiotics, and, in some cases, surgery. Even after successful sinusitis treatment, the sense of smell does not always return [24].
Nasal obstruction can also cause a loss of smell, which can be treated by removing the obstruction. Nasal polyps, nasal septum straightening, and sinus clearing are just a few examples. Anosmia caused by a nasal polyp may also be treated with steroids [6], as corticosteroids may increase the severity.
Stem Cell Therapy in Anosmia
Treatment is determined by the underlying cause. If you lose your sense of smell as a result of a cold, allergy, or sinus infection, it usually goes away on its own after a few days. If the anosmia does not go away, you should see a doctor [6]. Sinus infections and mucous membrane irritation can be treated with nasal sprays, steam inhalation, antibiotics, and, in some cases, surgery. Even after successful sinusitis treatment, the sense of smell does not always return [25].
Nasal obstruction can also cause a loss of smell, which can be treated by removing the obstruction. Nasal polyps, nasal septum straightening, and sinus clearing are just a few examples. Anosmia caused by a nasal polyp may also be treated with steroids [6], as corticosteroids may increase the severity Mice who received stem cell therapy responded normally to an unpleasant odour, whereas mice who did not received stem cell therapy did not. The ACE2 receptors are expressed by less than 2% of stem cells in the nasal epithelium, leaving plenty of room to restore the sense of smell [26]. Basal cells, sustentecular cells, and other supporting cells can be used as a precursor for stem cell therapy, which divides to produce new receptor neurones. The ability to regenerate olfactory receptor cells, successfully produce new neurones, and restore function in the mature central nervous system is a natural phenomenon. According to a rodent study, this renewal can take up to 6 to 8 weeks.
Testing of Anosmia in COVID-19 Patients
Olfactory function was assessed in all participants using either questionnaires like Did you have a decreased sense of smell before the start of COVID-19 pandemic, do you have a partial or complete loss of sense of smell, for how long has your decreases sense of smell persisted [29] or by the butanol threshold test (BTT). Patients with COVID-19 and abnormal olfaction were further evaluated using the smell identification test (SIT), sinus imaging, and nasoendoscopy [20].
Even though Sinusitis and olfactory cleft obstruction were absent in most COVID- 19 patients, 12 of 18 (67%) reported olfactory symptoms and OD was confirmed in 6 patients by BTT and SIT. Immunohistochemically analysis of nasal biopsy has revealed the presence of CD68 + macrophages harbouring severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antigens in the stroma. Olfactory dysfunction persisted in 2 patients despite clinical recovery [20].
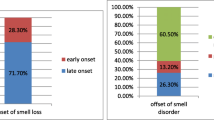
According to Olfactory Dysfunction in COVID-19 Patients: Prevalence and Prognosis for Recovering Sense of Smell shows the anosmia and hyposmia in patients with COVID-19, broken down by sex and inpatient vs outpatient status [9]. The results tell us that Among COVID-19-positive patients, 26 of 44 patients with COVID-19 reported olfactory dysfunction, including 19 of 23 outpatients and 7 of 20 inpatients.
Conclusion
Anosmia is one of the symptoms of COVID-19 patient, which can occur independently or with other symptoms. Recently tried out to find out the anosmia at the beginning of COVID19, but today there is no specific procedure or test methods available to detect in advance and also pathogenesis is not well understood. In-depth studies are needed to explore clinical features and pathogenesis of COVID-19 patient with Anosmia. Otolaryngologists should be understood of anosmia to avoid delaying the diagnosis of COVID-19 and thus contributing to an epidemic.
References
Meng X, Deng Y, Dai Z, Meng Z (2020) COVID-19 and anosmia: A review based on up-to-date knowledge. Am J Otolaryngol 41(5):102581
CDC. Symptoms of COVID-19 [Internet]. Centers for Disease Control and Prevention. 2022 [cited 2022 Apr 6]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
Callender LA, Curran M, Bates SM, Mairesse M, Weigandt J, Betts CJ (2020) The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front Immunol. https://doi.org/10.3389/fimmu.2020.01991
Human Coronavirus Types [Internet]. Cdc.gov. 2021 [cited 2022 Apr 6]. Available from: https://www.cdc.gov/coronavirus/types.html.
Routley N. Visualizing What COVID-19 Does to Your Body. 2020 Apr 10; Available from: https://www.visualcapitalist.com/visualizing-what-covid-19-does-to-your-body/
Anosmia: Symptoms, causes, and treatments [Internet]. WebMD. [cited 2022 Apr 6]. Available from: https://www.webmd.com/brain/anosmia-loss-of-smell
D’Ascanio L, Pandolfini M, Cingolani C, Latini G, Gradoni P, Capalbo M et al (2021) Olfactory dysfunction in COVID-19 patients: prevalence and prognosis for recovering sense of smell. Otolaryngol Head Neck Surg 164(1):82–86. https://doi.org/10.1177/0194599820943530
Han AY, Mukdad L, Long JL, Lopez IA (2020) Anosmia in COVID-19: mechanisms and significance. Chem Senses 45(6):423–428. https://doi.org/10.1093/chemse/bjaa040
Loss of smell (anosmia) [Internet]. Yale Medicine. 2020 [cited 2022 Apr 6]. Available from: https://www.yalemedicine.org/conditions/smell-and-taste-disorders
Nakagawara K, Masaki K, Uwamino Y, Kabata H, Uchida S, Uno S et al (2020) Acute onset olfactory/taste disorders are associated with a high viral burden in mild or asymptomatic SARS-CoV-2 infections. Int J Infect Dis. https://doi.org/10.1016/j.ijid.2020.07.034
Gori A, Leone F, Loffredo L, Cinicola BL, Brindisi G, De Castro G et al (2020) COVID-19-related anosmia: The olfactory pathway hypothesis and early intervention. Front Neurol 11:956. https://doi.org/10.3389/fneur.2020.00956
Le Bon SD, Horoi M (2020) Is anosmia the price to pay in an immune-induced scorched-earth policy against COVID-19? Med Hypothes. https://doi.org/10.1016/j.mehy.2020.109881
Bosso M, Thanaraj TA, Abu-Farha M, Alanbaei M, Abubaker J, Al-Mulla F (2020) The two faces of ACE2: the role of ACE2 receptor and its polymorphisms in hypertension and COVID-19. Mol Ther Method Clin Dev. https://doi.org/10.1016/j.omtm.2020.06.017
Torabi A, Mohammadbagheri E, Akbari Dilmaghani N, Bayat A-H, Fathi M, Vakili K et al (2020) Proinflammatory cytokines in the olfactory mucosa result in COVID-19 induced anosmia. ACS Chem Neurosci 11(13):1909–1913
Lop Gros J, Iglesias Coma M, González Farré M, Serra PC (2020) Olfactory dysfunction in COVID-19, a review of the evidence and implications for pandemic management. Acta Otorrinolaringol Engl Ed. https://doi.org/10.1016/j.otoeng.2020.04.002
Piret J, Boivin G (2020) Pandemics throughout history. Front Microbiol. https://doi.org/10.3389/fmicb.2020.631736
How COVID-19 causes loss of smell [Internet]. Harvard.edu. [cited 2022 Apr 6]. Available from: https://hms.harvard.edu/news/how-covid-19-causes-loss-smell
CDC. Guidance for antigen testing for SARS-CoV-2 for healthcare providers testing individuals in the community [Internet]. Centers for Disease Control and Prevention. 2022 [cited 2022 Apr 6]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html
Chung TW-H, Sridhar S, Zhang AJ, Chan KH, Li HL, Wong FKC et al (2020) Olfactory dysfunction in coronavirus disease 2019 patients: Observational cohort study and systematic review. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofaa199
India’s first CRISPR Covid-19 test, developed by the Tata Group and CSIR-IGIB, approved for use in India [Internet]. Gov.in. [cited 2022 Apr 6]. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1656770
Wagner T, Shweta F, Murugadoss K, Awasthi S, Venkatakrishnan AJ, Bade S et al (2020) Augmented curation of clinical notes from a massive EHR system reveals symptoms of impending COVID-19 diagnosis. Elife. https://doi.org/10.7554/eLife.58227
MSD Manuals. The Nose. 2022.
Marciniak-Firadza R (2021) The sense of smell in logopaedic theory and practice. Logopaedica Lodziensia. https://doi.org/10.18778/2544-7238.05.08
Cooper KW, Brann DH, Farruggia MC, Bhutani S, Pellegrino R, Tsukahara T et al (2020) COVID-19 and the chemical senses: supporting players take center stage. Neuron 107(2):219–233. https://doi.org/10.1016/j.neuron.2020.06.032
Kurtenbach S, Goss GM, Goncalves S, Choi R, Hare JM, Chaudhari N et al (2019) Cell-based therapy restores olfactory function in an inducible model of hyposmia. Stem Cell Rep 12(6):1354–1365. https://doi.org/10.1016/j.stemcr.2019.05.001
Lewis R. Sniffing out stem cells behind COVID-skewed olfaction [Internet]. The Niche. 2020 [cited 2022 Apr 6]. Available from: https://ipscell.com/2020/08/sniffing-out-stem-cells-behind-covid-skewed-olfaction/
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shamsundara, M., Jayalakshmi, L. Anosmia—An Effect of COVID-19 Infection-Review. Indian J Otolaryngol Head Neck Surg 75 (Suppl 1), 815–821 (2023). https://doi.org/10.1007/s12070-022-03401-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03401-w