Abstract
Castleman disease is an uncommon nonneoplastic, lymphoproliferative disorder of that is associated with lymphadenopathy and nonclonal lymph nodes hyperplasia. It is further subdivided into two types: Unicentric Castleman disease and Multicentric Castleman disease. Unicentric Castleman disease is rare to be reported in patients having AIDS, because HIV infected patients most commonly presented with Multicentric Castleman disease and they mostly coinfected with HHV-8. Herein we reported a rare presentation of Unicentric Castleman disease with hyaline vascular variety evident Histopathologically as a preoperative diagnosis. The patient was initially managed conservatively and surgical excision (excisional biopsy) of the left cervical lymph node was than performed and sent for histopathology. The Immunohistochemistry findings were also consistent with the diagnosis of Castleman disease Hyaline vascular type as evident from left cervical lymph node excisional biopsy.
Similar content being viewed by others
Introduction
Castleman disease, another name of angiofollicular lymph node hyperplasia that was initially reported by Dr Benjamin Castleman in 1956 [1]. Castleman disease is described as an uncommon lymphoproliferative, nonneoplastic lymphadenopathy and nonclonal lymph node hyperplasia that can occur throughout the body [2]. Castleman disease itself is not a malignant condition; however, it is significantly associated with certain other malignancies like B-cell lymphomas and POEMS (polyneuropathy, organomegaly, endocrinopathies, monoclonal gammopathies and some skin abnormalities like pemphigus) [3].
The Castleman disease is classified is classified on the basis of morphological and histopathological patterns. Morphologically the disease is classified into unicentric and multicentric Castleman disease depending upon levels of lymph nodes involvement, and according to the histopathogenetic classification it is further classified into three subtypes such as hyaline vascular Castleman disease being common one followed by plasma cell Castleman disease, and human herpesvirus 8 associated Castleman disease [4]. Fever, night sweets, weight loss and fatigue were the most common presenting complaints associated with the Castleman disease [5, 6].
This case report is aiming to highlight a rare case of Castleman disease reported in 39 years old male presenting in department of Ear, Nose and throat (ENT) department of PNS Shifa Hospital, Karachi, Pakistan.
Case Report
We reported a case of 48-year-old female presented to the outpatient department of Ear, Nose, and Throat PNS Shifa Hospital, Karachi with presenting complaint of fever, weight loss and supraclavicular swelling more marked on left side.
Patient presented with complaint of fever that was non-documented, episodic in nature having no associated rigors and chills and weight loss of 10 kg from last 1 year. Patient also complained of a supraclavicular swelling from last 1.5 years that was slowly growing, nodular, soft to firm, non-tender, non-mobile and involving supraclavicular lymph nodes of the right and left side of the neck, with marked swelling in the left side than on the right side of the neck.
Initially, baseline investigations, erythrocyte sedimentation rate (ESR) and C-reactive protein were sent. The lab reports were showing anemic picture with hemoglobin level of 9.2, platelet count 132 and ESR of 46 with raised CRP (qualitatively). The contrast enhanced Computerized tomographic (CT) scan of neck region was performed in March, 2021. Before CECT the renal function tests were sent to rule out any pre-existing, undiagnosed renal disease, however, the renal function tests were normal and patient was proceeded for CECT. While performing CECT 5 mm axial slices were taken from base of the skull to apex and IV contrast was given.
On CECT multiple enlarged lymph nodes were seen in all cervical levels (L > R). Few of them showed internal necrosis. Largest one in left supraclavicular region showed areas of internal necrosis 3.5 × 3.4 cm (Fig. 1). Another one at right level III measured 1.0 cm in short axis and at level IB measures 1.0 cm in short axis on left side. Rest of the neck region was normal with no significant findings.
However, due to COVID-19 pandemic much of the patient follow-up was interrupted, but still patient was conservatively managed and fever was managed by paracetamol, an acetaminophen in SOS basis and Augmentin (co-amoxiclav and clavulanic acid) 675 mg OD was prescribed for initial 5 days.
In the same duration of 2 weeks patient was also counselled for Ultrasound guided fine needle aspiration cytology (FNAC) of supraclavicular lymph nodes and was performed in April, 2021. The hemorrhagic aspirate was obtained in one pass and a total of 4 slides were prepared (2 alcohol fixed and 2 air dried), Diff Quick, H&E and Pap stains were applied. The smear examination showed moderate cellularity with polymorphous population of lymphoid cells at various stages of maturation, and reactive hyperplasia was seen.
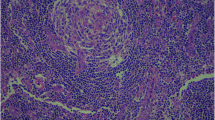
After FNAC the patient was planned for surgical excision (excisional biopsy) and patient’s workup for anesthesia fitness was started. All baseline investigations were performed and patient was optimized for surgery that was performed in July, 2021, however, during anesthesia fitness patient was also found to be Human Herpes Virus-8 (HHV-8) and HIV-positive on serological basis and special surgical protocols were followed. After surgical excision the mass was sent to histopathology that revealed lymphoid mass with atretic germinal centers traversed by penetrating hyalinized vessels. The mantel zones were thickened with lymphocytes arranged in layers imparting onion skin appearance with reactive lymphoid hyperplasia was also seen on histological examination (Fig. 2).
The Immunohistochemistry findings were also consistent with the diagnosis of Castleman disease Hyaline vascular type as evident from left cervical lymph node excisional biopsy (Table 1).
Discussion
Castleman disease is a group of diseases elaborated as a rare benign lymphoid proliferative disorder, which is clinically classified into two main types unicentric Castleman disease (UCD) and multicentric Castleman disease (MCD) [7]. UCD refers to solitary or multiple lesions in adjacent organs in a range of lesions that are limited to the same lymphoid region. MCD refers to multiple lesions involving more than two non-adjacent lymphoid regions or accompanied by other sites or organs [8]. Histopathologically, CD is further classified into 3 subtypes such as:
-
Hyaline vascular type.
-
Plasma cell type.
-
Mixed type.
There observed to be a paramount association of hyaline vascular type and UCD with significance of better prognosis with type of UCD following early surgical resection as compared to MCD that is treated chemotherapeutically with poor prognosis [8]. The hyaline-vascular type is characterized by hyaline vascular lymph follicles with expended mantle zones having concentric rings of lymphocytes forming an onion skin appearance and an interfollicular capillary proliferation with perivascular hyalinization. The plasma cell type is characterized by variable germinal center hyperplasia and mantle zone expansion with relatively preserved lymph node architecture and plasma cells proliferation. The mixed type is combination of both hyaline vascular and plasma cell type [9].
We reported herein a case of unicentric Castleman disease in a 48-year-old female G3P3 + 0 who presented with complain of fever, weight loss and supraclavicular swelling. On histopathological report of the involved lymph nodes lymphoid mass with atretic germinal centers traversed by penetrating hyalinized vessels was seen. The mantel zones were thickened with lymphocytes arranged in layers imparting onion skin appearance with reactive lymphoid hyperplasia validating the presence of hyaline vascular type of UCD. Fever, night sweets, weight loss and fatigue were the most common presenting complaints associated with the Castleman disease [5] and our patient also reported with complaint of fever, weight loss, fatigue and supraclavicular swelling from last 1.5 year. While investigating for anesthesia fitness the antibodies to HIV were also found positive that is in concordance with association of Castleman disease with HIV infection as evident from the existing literature [10].
Conclusion
Castleman disease, another name of angiofollicular lymph node hyperplasia that was initially reported by Dr Benjamin Castleman in 1956. Castleman disease is described as an uncommon lymphoproliferative, nonneoplastic lymphadenopathy and nonclonal lymph node hyperplasia that can occur throughout the body. Unicentric Castleman disease is a rare disease associated with other malignancies, though itself it is nonmalignant. Unicentric Castleman disease is a rare type of Castleman disease associated with HIV and HHV-8 infection. Our objectives were to describe a case of HIV and HHV-8 associated Unicentric Castleman disease with various radiological and histopathological correlations. All baseline investigations and Excisional biopsy were performed and findings were consistent with the diagnosis of Castleman disease of Hyaline vascular type.
References
Waterston A, Bower M (2004) Fifty years of multicentric Castleman’s disease. Acta Oncologica (Stockholm, Sweden) 43(8):698–704. https://doi.org/10.1080/02841860410002752
Liu AY, Nabel CS, Finkelman BS, Ruth JR, Kurzrock R, van Rhee F et al (2016) Idiopathic multicentric Castleman’s disease: a systematic literature review. Lancet Haematol 3(4):e163–e175. https://doi.org/10.1016/S2352-3026(16)00006-5
Marcu RD, Spinu AD, Socea B, Bodean MO, Diaconu CC, Vasilescu F et al (2018) Castleman’s disease—clinical, histological and therapeutic features. Rev Chim (Bucharest) 69(4):823–830
Haap M, Wiefels J, Horger M, Hoyer A, Müssig K (2018) Clinical, laboratory and imaging findings in Castleman’s disease: the subtype decides. Blood Rev 32(3):225–234. https://doi.org/10.1016/j.blre.2017.11.005
Wang T, Chen X, Chen W, Shi L, Liu J (2021) A retrospective study of 44 patients with head and neck Castleman’s disease. Eur Arch Oto-rhino-laryngol. https://doi.org/10.1007/s00405-021-07065-0
Gündüz E, Özdemir N, Bakanay ŞM, Karakuş S (2021) A rare lymphoproliferative disease: castleman disease. Turk J Haematol 38(4):314–320. https://doi.org/10.4274/tjh.galenos.2021.2021.0440
Cheng JL, Cui J, Wang Y, Xu ZZ, Liu F, Liang SB, Tian H (2018) Unicentric Castleman disease presenting as a retroperitoneal peripancreatic mass: a report of two cases and review of literature. World J Gastroenterol 24(34):3958–3964. https://doi.org/10.3748/wjg.v24.i34.3958
Sun X, Du Y, Zhang Y, Wang R, Hou D (2021) Unicentric Castleman disease: multidetector computed tomography classification with surgical and pathologic correlation. Quant Imaging Med Surg 11(8):3562–3568. https://doi.org/10.21037/qims-20-1033
Cronin DM, Warnke RA (2009) Castleman disease: an update on classification and the spectrum of associated lesions. Adv Anat Pathol 16(4):236–246. https://doi.org/10.1097/PAP.0b013e3181a9d4d3
Mahroug ER, Sher-Locketz C, Desmirean MS, Abayomi EA, Tomuleasa C, Grewal R (2018) Castleman’s disease in the HIV-endemic setting. Cancer Manag Res 10:4553–4563. https://doi.org/10.2147/CMAR.S175648
Funding
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human Participants and/or Animals
This case report involves a human participant. All procedures performed in the study involving human participant were in accordance with the ethical standards of the departmental research committee.
Informed Consent
The participant has consented to the submission of the case report to the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maqbool, S., Javed, A., Idrees, T. et al. Unicentric Castleman Disease: A Rare Diagnosis of Radiological and Histological Correlation. Indian J Otolaryngol Head Neck Surg 75, 975–978 (2023). https://doi.org/10.1007/s12070-022-03253-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03253-4