Abstract
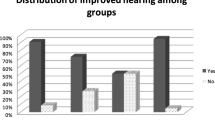
The aim of the study was to assess the role of mastoidectomy with type 1 tympanoplasty in the management of paediatric patients with poor contralateral ear status and to evaluate the prognostic factors that may influence the success outcome of type 1 tympanoplasty. A prospective study of 112 paediatric patients from 4 to 12 years of age. All patients in the study had bilateral ear perforations. They were randomly assigned to undergo either type 1 tympanoplasty (group 1, n = 56) or type 1 tympanoplasty with mastoidectomy (group 2, n = 56). The outcomes between the two groups were compared at 12 months postoperative period. The outcomes evaluated were: 1. anatomical condition of the tympanic membrane, 2. functional improvement in hearing (≥ 10 db), 3. air-filled middle ear space without atelectasis or otitis media with effusion, 4. overall outcome. The outcomes were also compared in both the surgical groups for patients who were ≤ 8 years (n = 51) and > 8 years (n = 61) of age. Prognostic factors for success outcome for type 1 tympanoplasty were evaluated. The prognostic factors considered were age at the time of surgery, age groups, duration of the disease prior to surgery, previous adenoidectomy, mechanism of perforation, location of perforation, size of the perforation, type of ear surgery performed (tympanoplasty with or without mastoidectomy). The success outcome in anatomical condition of the tympanic membrane was significantly higher in mastoidectomy group (p = 0.015) but was not significantly different in those ≤ 8 years and > 8 years (p = 0.112, p = 0.064 respectively).There was no difference in the functional improvement in hearing in both the surgical groups for all patients, ≤ 8 years and > 8 years (p = 0.188 p = 0.061, p = 0.865 respectively). Mastoidectomy group showed significantly higher success outcome for air-filled middle ear space without atelectasis or OME for all patients, ≤ 8 years and > 8 years (p < 0.001, p = 0.004, p = 0.041 respectively).Overall success was significantly higher in mastoidectomy group for all patients and ≤ 8 years (p = 0.040, p = 0.012 respectively),but not significantly different for > 8 years (p = 0.592).Out of the prognostic factors considered for success only the type of ear surgery performed showed as a better predictor for success (AUC = 0.606, p = 0.046). Cortical mastoidectomy done along with type 1 tympanoplasty in paediatric patients with poor contralateral ear showed statistically significant higher overall success outcome. Although mastoidectomy done with type 1 tympanoplasty showed better success outcome in patients above 8 years, it was not statistically significant. Except the type of ear surgery performed, none of the prognostic factors considered could influence the success outcome. Our study recommends mastoidectomy to be combined with type 1 tympanoplasty in paediatric patients aged ≤ 8 years with poor contralateral ear status to enhance the overall success outcome.

Similar content being viewed by others
Data Availability
Data collected and documented while individual patients included in the study were treated at military hospitals.
References
Lau T, Tos M (1986) Tympanoplasty in children. An analysis of late results. Am J Otol 7(1):55–59
Sarkar S, Roychoudhury A, Roychaudhuri BK (2009) Tympanoplasty in children. Eur Arch Otorhinolaryngol 266(5):627–633
Hardman J, Muzaffar J, Nankivell P, Coulson C (2015) Tympanoplasty for chronic tympanic membrane perforation in children: systematic review and meta-analysis. Otol Neurotol 36(5):796–804
Lau T, Tos M (1988) When to do tympanoplasty in children? PediatrOtol 40:156–161
Martin C, Karkas A, Prades J-M (2017) Tubotympanic system functioning. Eur Ann Otorhinolaryngol Head Neck Dis 134(3):177–184
Seibert JW, Danner CJ (2006) Eustachian tube function and the middle ear. OtolaryngolClin N Am 39(6):1221
Alper CM et al (2011) Role of the mastoid in middle ear pressure regulation. The Laryngoscope 121(2):404–408
Doyle WJ (2007) The mastoid as a functional rate-limiter of middle ear pressure change. Int J Pediatr Otorhinolaryngol 71(3):393–402
Di Martino EF (2013) Eustachian tube function tests: an update. HNO 61(6):467–476
van Heerbeek N, Ingels KJ, Snik AF, Zielhuis GA (2001) Reliability of manometric eustachian tube function tests in children. Otol Neurotol 22(2):183–187
Todd NW (2000) There are no accurate tests for eustachian tube function. Arch Otolaryngol Neck Surg 126(8):1041–1042
Ashry Y, Ward BK, Poe DS (2017) Can we use the status of one ear to predict Eustachian tube function of the contralateral ear? The Laryngoscope 127(7):1491–1492
McGrew BM, Jackson CG, Glasscock ME III (2004) Impact of mastoidectomy on simple tympanic membrane perforation repair. The Laryngoscope 114(3):506–511
Eliades SJ, Limb CJ (2013) The role of mastoidectomy in outcomes following tympanic membrane repair: a review. The Laryngoscope 123(7):1787–1802
Bluestone CD (2004) Studies in otitis media: Children’s Hospital of Pittsburgh-University of Pittsburgh progress report—2004. The Laryngoscope 114(S105):1–26
Proctor B (1991) Chronic otitis media and mastoiditis. Otolaryngology 2:1366–1368
Brodsky L (1989) Modern assessment of tonsils and adenoids. PediatrClin N Am 36(6):1551–1569
Umapathy N, Dekker PJ (2003) Myringoplasty: is it worth performing in children? Arch Otolaryngol Neck Surg 129(10):1053–1055
Bluestone CD, Rood SR, Swarts JD (1998) Anatomy and physiology of the eustachian tube. Otolaryngol Head Neck Surg, pp 3003–3025
Verhoeff M, van der Veen EL, Rovers MM, Sanders EA, Schilder AG (2006) Chronic suppurative otitis media: a review. Int J Pediatr Otorhinolaryngol 70(1):1–12
Morris PS, Leach AJ (2009) Acute and chronic otitis media. Pediatr Clin 56(6):1383–1399
Baklaci D, Guler I, Kuzucu I, Kum RO, Ozcan M (2018) Type 1 tympanoplasty in pediatric patients: a review of 102 cases. BMC Pediatr 18(1):1–6
Agrawal A, Bhargava P (2017) Comparative evaluation of tympanoplasty with or without mastoidectomy in treatment of chronic suppurative otitis media tubotympanic type. Indian J Otolaryngol Head Neck Surg 69(2):172–175
Dispenza F, Mistretta A, Gullo F, Riggio F, Martines F (2021) Surgical management of retraction pockets: does mastoidectomy have a role? Int Arch Otorhinolaryngol 25(1):e12–e17. https://doi.org/10.1055/s-0040-1709196
Ramakrishnan A, Panda NK, Mohindra S, Munjal S (2011) Cortical mastoidectomy in surgery of tubotympanic disease. Are we overdoing it? The Surgeon 9(1):22–26
Baz MR (2020) Effect of cortical mastoidectomy on audiological outcomes in mucosal chronic otitis media. Al-Azhar Int Med J 1(1):258–263
Yoon TH, Park S-K, Kim JY, Pae KH, Ahn JH (2007) Tympanoplasty, with or without mastoidectomy, is highly effective for treatment of chronic otitis media in children. Acta Otolaryngol (Stockh) 127(sup558):44–48
Funding
This research did not receive any specific Grant from any funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
All medical and surgical interventions performed in this study involving the human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Written informed consent was obtained from all individual patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guthikonda, M.R., Gude, A. & Naga, R. Role of Mastoidectomy with Type 1 Tympanoplasty in Paediatric Patients with Poor Contralateral Ear Status. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 631–638 (2022). https://doi.org/10.1007/s12070-021-02457-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02457-4