Abstract
Previous studies have investigated the impact of air pollution on health and mortality. However, there is little research on how this impact varies by individuals’ ethnicity. Using a sample of more than 2.5-million individuals aged 16 and older from the 2011 UK census linked to 10-years air pollution data, this article investigates the effect of air pollution on self-reported general health and limiting long-term illness (LLTI) in five main ethnic groups and by country of birth in UK. The association of air pollution with self-reported health and LLTI by individual’s ethnicity was examined using two levels mixed-effects generalised-linear models. Pakistani/Bangladeshi, Indian, Black/African/Caribbean, and other ethnic minorities and people born outside UK/Ireland were more likely to report poorer health and the presence of LLTI than White-group and UK/Ireland born individuals. Higher concentrations of NO2, SO2 and CO pollutants were associated with poorer self-reported health and the presence of LLTI in the UK population. Analysis by ethnicity showed a more pronounced effect of NO2, PM10, PM2.5, and CO air pollution on poor self-reported health and the presence of LLTI among ethnic minorities, mostly for people from Black/African/Caribbean origin compared to White people, and among non-UK/Ireland born individuals compared to natives. Using a large-scale individual-level census data linked to air pollution spatial data, our study supports the long-term deteriorating effect of air pollution on self-reported health and LLTI, which is more pronounced for ethnic minorities and non-natives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Air pollution has significantly increased worldwide in the last century due to industrial growth, increased population size, urbanization, and high energy consumption (Ab Manan et al., 2018; Abed Al Ahad et al., 2020a). Air pollution including nitrogen dioxide (NO2), particulate matter (PM10, with diameters of less than 10 µm and PM2.5 with a diameter of less than 2.5 µm), carbon monoxide (CO), Sulphur dioxide (SO2), and Ozone have been found to cause a wide range of acute and chronic health conditions (Ab Manan et al., 2018). Most of the literature has shown associations of short-term and long-term air pollution exposure with objective health measures such as mortality and hospitalization, especially related to cardiovascular and respiratory diseases (Abed Al Ahad et al., 2020b; Almendra et al., 2016; Atkinson et al., 2015; Beelen et al., 2014; Stafoggia et al., 2016). For instance, elevated risks of cardiovascular and respiratory mortality were reported in Istanbul-Turkey for every 10 µg/m3 increase in daily concentrations of PM10, SO2 and NO2 pollutants (Capraz et al., 2016). Poor self-rated health was also found to be associated with increased short-term exposure to air pollution, particularly with PM2.5 pollution (Goldberg et al., 2015). Additionally, self-perceived mental health including stress, depression and suicide ideation was found to be related to long-term exposure to NO2, CO, and PM10 pollution (Shin et al., 2018).
The association between air pollution and health outcomes is not direct and several socio-economic, individual, and environmental factors can modify this association. Age (elderly and children vs adults), gender, socioeconomic factors (poverty, education, unemployment, and income, among others), pre-existing chronic diseases, use of certain medications, and environmental conditions such as the winter season increase individual’s susceptibility to ambient air pollution and its associated illness (Charafeddine & Boden, 2008; Colais et al., 2012; De Sario et al., 2013; Faustini et al., 2016; Willers et al., 2016). Research in France has shown that the association between air pollution and poor self-rated health is affected by residency in more deprived areas, socio-economic insecurity, older age, and unemployment (Fleury-Bahi et al., 2015). In China, the negative effect of air pollution on self-rated health increased with low socioeconomic status (Jiao et al., 2018) and in Germany, a 40% increase in poor health was associated with job insecurity and annoyance due to air pollution (Riedel et al., 2017).
Although the association between air pollution and health, whether in terms of objective (mortality and hospitalization) or subjective (self-reported health) measures, is established in the literature, the ethnic and migrant dimension in modifying that association is lacking, particularly in research on European countries as per a recent published scoping systematic literature review (Abed Al Ahad et al., 2020b). Most of the research about the effect of air pollution on health by ethnicity have been conducted in the U.S. (Johnson & Parker, 2009; Nachman & Parker, 2012; Parker et al., 2018), which is characterised by a different ethnic composition and structure than Europe; and to the best of our knowledge, only one study investigated the effect of air pollution on respiratory health by ethnic groups in the UK (Astell-Burt et al., 2013). Our study intends to fulfil the aforementioned literature gap using a very large census-based nationally representative sample of more than 2.5 million UK individuals linked to a spatial-rich contextual 10-years air pollution data for six pollutants (NO2, SO2, PM10, PM2.5, CO, and ozone) at the local authority level. We hypothesise that the ethnic inequalities mechanisms (Socio-economic differences; Living in urban, highly polluted areas; and Genetic composition) explained in the next section of this article may contribute to a more pronounced effect of air pollution on self-reported health and LLTI among ethnic minorities and foreign-born individuals in the UK. The objectives of this study are: First, to investigate the association of ethnicity and country of birth with self-reported general health and limiting long-term illness (LLTI), adjusting for the main individuals’ socio-demographic characteristics. Second, to examine the association of exposure to long-term (10-years) NO2, SO2, PM10, PM2.5, CO, and ozone air pollution with self-reported general health and LLTI in the overall population. Finally, to study the effect of ethnicity and country of birth on the association of air pollution with self-reported health and LLTI using interaction terms between air pollution and ethnicity variables.
Mechanisms Underlying Ethnic Inequalities in Health in the Context of Exposure to Air Pollution
In order to better understand the effect of ethnicity and country of birth on the association between air pollution and health, it is important to provide an overview about the mechanisms underlying ethnic inequalities in health in the UK. Literature in this field has shown that ethnic minorities exhibit poorer self-reported health in comparison to the White group which was mainly explained by three conditions: 1) Socio-economic differences; 2) Living in urban, highly polluted areas; and 3) Genetic composition. We hypothesise that these mechanisms may contribute to a more pronounced effect of air pollution on health and LLTI for ethnic minorities and foreign-born individuals in the UK.
Socio-economic differences between ethnic groups are considered one of the most important determinants of ethnic inequality in health (Fischbacher et al., 2014). Many studies show that ethnic minorities have poor health due to the fact that they live in more disadvantaged communities and have lower socio-economic status as well as poor housing conditions and healthcare coverage as compared to the majority of population (Egede, 2006; Pearce et al., 2006; Su et al., 2011). In the UK, the poorest health is often reported by Bangladeshi and Pakistani ethnic groups, followed by Caribbeans and Indians (Cézard et al., 2020; Nazroo, 2003). However, when socio-economic factors such as educational attainment, occupation, social class, income, and household tenure, are controlled for these observed differences by ethnic groups are significantly reduced (Cézard et al., 2020; Evandrou et al., 2016). A study conducted in Sweden showed that people of Turkish origin were less likely to report poor health as compared to the native Swedish people, once economic resources and educational level had been accounted for (Wiking et al., 2004). Evidence from the US also points to the socio-economic dimension as the main contributor to the observed health disparities between the “White” and “Black” population (Assari, 2017; Lanting et al., 2005). This supports the importance of socio-economic factors in shaping the ethnic inequalities in health. However, the interaction of different socio-economic factors and the validity of their measurement among different ethnic groups remains controversial. Besides ethnic origin, ethnic inequalities in health can be also examined through the lens of migration. In England and Scotland, immigrants were shown to have lower levels of limiting long-term illness as compared to people born in those countries (Wallace & Kulu, 2014). Mortality from all causes was also shown to be lower for immigrants in England and Wales (Wallace & Kulu, 2015). This could be explained by the “healthy migrant effect”: immigrants who leave their countries of origin tend to be healthier than those who stay in the country of origin and the population in the destination country (Cézard et al., 2020; Wallace & Kulu, 2014). Yet over time, immigrants assimilate to the culture and living habits of the destination country, a process named as “acculturation”, gradually exhibiting health behaviours related to their diet, smoking, and alcohol consumption similar to that of the native population (Abraído-Lanza et al., 2005). Therefore, the mortality/health advantage of immigrants does not extend to their descendants who tend to have poorer health than their parents. Despite the “healthy migrant effect”, a study conducted in 11 European countries showed contradictory results in people aged 50 and above whereby migrants reported poorer health than the native population (Solé-Auró & Crimmins, 2008).
Living in urban, highly polluted areas and cities, near major roads increases the exposure to air pollution resulting mostly from traffic exhaust (Zhang & Batterman, 2013). Ethnic minorities and immigrants often choose to live in urban areas and major cities due to better working opportunities, and shorter commuting distances and transportation expenses (Lucas et al., 2019). Additionally, ethnic minorities often live in the less expensive social housing (houses offered by local authorities) rather than private housing. Social housing is frequently located in ethnic concentration neighbourhoods, in more deprived highly populated areas, or near main roads (van Ham & Manley, 2009). Thus, a more pronounced effect of air pollution on health is expected among ethnic minorities in comparison to the majority of the population who have more financial resources and inheritance tenure to move away from major cities.
The genetic composition of some ethnic groups can place them at a health disadvantage. For example, South Asians including Pakistani, Bangladeshi and Indians are at a higher risk for coronary heart diseases due to their evolutionary history of adaptation to “surviving under periodic famine and low energy intake” conditions leading to the formation of “insulin resistance syndrome” (Nazroo, 1998). Thalassaemia and sickle cell diseases are more common among people from countries with a historically higher prevalence of Malaria (Stronks et al., 2013). Nevertheless, the association between genetic profile for certain ethnic groups and diseases is not direct and interactions between genes and environment referred to as “epigenetics” might increase the susceptibility for certain diseases including hypertension and diabetes (Webster et al., 2013). Therefore, genes among certain ethnic groups might have been exposed to mutations due to certain interactions with the environment rather than the genetic factor itself. For instance, higher risk for tuberculosis among people from South Asia might be related to polymorphisms in the vitamin D receptor that evolved based on a specific gene-environment interaction pathway (Chaturvedi, 2001).
Methods
Study Design and Population
A cross-sectional design was employed using a sample of the most recent available UK census microdata from 2011 (Note: the 2021 UK census data is not available at the present). The 2011 micro-census data is publicly available by the UK Data Archive under the terms of the Open Government Licence (National-Records-of-Scotland, 2011; Northern-Ireland-Statistics-and-Research-Agency, 2011; Office-for-National-Statistics, 2011); and it contains information on the individuals’ socio-demographic characteristics (e.g. age, gender, household deprivation, ethnic groups, country of birth, type of work industry, marital status, and educational qualification), self-reported health, LLTI and the local authority of the individual’s place of residence. It also contains information on whether individuals have changed their local authority of residence in the year preceding the census date. Local authorities with populations below 120,000 individuals are aggregated with neighbouring local authorities and used as an indication of the individual’s place of residence, amounting for a total of 296 local authorities/aggregate local authorities across the UK. The policy of the UK Data Archive does not allow the release of individual’s address/postcode to researchers for confidentiality reasons.
Census data are available on a five-percent random sample of individuals in England and Wales (N = 2,848,149), Scotland (N = 267,072), and Northern Ireland (N = 91,783). The three datasets were then merged into one with a total sample of 3,207,004 individuals. Of the total, we excluded 600,277 children aged below 16 and 32,367 adult individuals that had missing data for self-reported general health; resulting in a final sample of 2,574,360 individuals aged 16 and above.
Variables and Measurements
Health-Related Outcomes
This study included two health outcomes:
-
1)
Self-reported general health is an ordinal variable that measures how individuals perceive their general health in the last 12 months preceding the census date: 1 = very good health, 2 = good health, 3 = fair health, 4 = bad health, and 5 = very bad health.
-
2)
Self-reported LLTI captures the existence of long-term health problems such as disability, obesity, cardiovascular and respiratory diseases, and being anxious or depressed, that have limited individuals’ daily activities over the last 12 months preceding the census date. It was originally coded as a categorical variable (1 = day to day activities limited a lot, 2 = day to day activities limited a little, 3 = day to day activities not). Given that most individuals (79%) reported that daily activities were not limited, we recoded the variable into a binary format with 0 = day to day activities not limited and 1 = day to day activities were limited.
Air Pollution
Annual air pollution data (combining all sources of air pollution including industrial/combustion processes and road traffic) were downloaded from the “Department for Environment Food and Rural Affairs” website (Department-for-Environment-Food-and-Rural-Affairs, 2020). These are raster data estimated using air dispersion models at a spatial resolution of 1 × 1 km UK National Grid for NO2, SO2, PM10, PM2.5, CO and ozone pollutants and are available for a period of ten years (2002 through 2011). An exception was ozone where data were available from 2003 to 2011 and CO where data were available from 2002 to 2010. Data are given as raster cells of mean annual concentrations of air pollution, measured in µg/m3 for NO2, SO2, PM10, and PM2.5 pollutants, while CO was measured in mg/m3 and ozone as the number of days per year where the daily maximum 8-h mean concentrations exceeds 120 µg/m3.
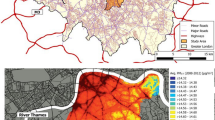
To link the 1 × 1 km spatial air pollution data to the 2011 census data at the local authority level, we calculated the mean concentration for each pollutant from all the raster cells that fell within each local authority. We did so for each pollutant and for each year (2002 through 2011) across the local authorities (Office-for-National-Statistics et al., 2011). A map showing the local authorities in the UK (council areas in Scotland) and an enlarged subset of 20 local authorities in the south-east of UK with an example of NO2 concentrations at 1 × 1 km grid for the year of 2011 was used to illustrate this process (Fig. 1). For local authorities with populations below 120,000 persons that are aggregated with neighbouring local authorities in the 2011 census data, the average air pollution concentrations were computed across the aggregated areas. Next, the average concentrations across the ten years for each pollutant (from 2002 to 2011 for NO2, SO2, PM10, PM2.5, from 2002 to 2010 for CO, and from 2003 to 2011 for ozone) at the local authority level were calculated. These average concentrations were then linked to our census data for each individual using the local authority variable and used as an indication of individuals’ long-term ambient air pollution exposure.
Given that the average 10-years air pollution data was linked to the census data at the local authority of residence for each individual, we cannot rule out exposure misclassification and stationarity bias by assuming that every individual within the same local authority is exposed to the same level of air pollution, that individuals spend most of their time in one local authority, and that individuals did not change their place of residence from one local authority to another during the 10-year time interval. Recent literature debates have been pointing toward the importance of considering non-stationarity and dynamic data sources (e.g. GPS data) when examining relationships between environmental exposures and health impacts as these relationships may vary over space (spatial non-stationarity) and time (temporal non-stationarity); and by assuming stationarity, we are at the risk of exposure misclassifications (Campbell et al., 2021; Kwan, 2021). However, this is a limitation that we had to accept when analysing the effect of air pollution on health using a large national representative sample of more than 2.5 million individuals from the 2011 UK micro-census without compromising individuals’ confidentiality. Nevertheless, we accounted partially for the stationarity and misclassification bias through a sensitivity analysis on individuals who did not change their local authority of residence in the year preceding the 2011 census date.
Ethnicity and Country of Birth
The 2011 UK census data included information on the individuals’ ethnic group and their respective country of birth. Consequently, we created a binary variable “country of birth” which is coded as 1 = born in UK or Ireland and 2 = not born in UK or Ireland to represent the migration effect. Ireland includes both Northern Ireland and Republic of Ireland. The variable “ethnicity” was classified in this study as follows: 1 = White; 2 = Pakistani/Bangladeshi; 3 = Indian; 4 = Black/African/Caribbean; and 5 = Other ethnicities. We kept the same classification as in the 2011 UK census except for Pakistani and Bangladeshi groups, which were merged into one category as they showed similar trends in health; and “Asian others” and “mixed ethnicity”, which were merged with the “other ethnicities” category as they did not represent a specific ethnic group.
Covariates
Socio-demographic covariates (Table 1) were selected based on the effect modifiers considered in relevant literature (Abed Al Ahad et al., 2020b). These included age, gender, marital status, education, type of work industry, and nation.
Data Analysis
Descriptive analysis was conducted to assess the sample’s socio-demographic characteristics, health outcomes, and air pollution concentrations using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Descriptive statistics were computed for the whole UK sample and separately for England, Wales, Scotland, and Northern Ireland. We also examined the correlation between the six pollutants (NO2, SO2, PM10, PM2.5, CO, and ozone) and population density using the Pearson’s correlation coefficient. Coefficients of 0.7 and more indicate the presence of a strong relationship (Schober et al., 2018).
To address the first objective of the study, we examined the association of each of ethnicity (White as the reference group) and country of birth (born in UK or Ireland as the reference group) with the ordinal self-reported general health outcome using ordinal logistic regression. And in a separate model, we examined the association of ethnicity and country of birth with the binary self-reported LLTI outcome using binary logistic regression. The two regression models were adjusted for the main socio-demographic covariates which were selected based on the effect modifiers considered relevant in the literature (Abed Al Ahad et al., 2020b). In a sensitivity analysis, we performed a combination of four simpler models to examine the association of ethnicity and country of birth with each of self-reported general health and LLTI outcomes (Online Resource Tables 1 and 2). Model 1 adjusted only for age, gender, and nation; model 2 adjusted for age, gender, nation, and marital status; model 3 adjusted for age, gender, nation, and education; and model 4 adjusted for age, gender, nation, and type of work industry (Online Resource Tables 1 and 2). Prior to the model building stage, correlation between the covariates was assessed using Cramer’s V coefficients. Given the absence of strong correlations (Online Resource Table 3), all the socio-demographic covariates were included in the final regression models. We also performed stratified analysis by age groups to examine whether age modifies the association between ethnicity, country of birth and each of the two self-reported health outcomes. A bar chart was used to visualize the age distribution by ethnicity and country of birth (Online Resource Figures 1 and 2).
To address the second objective of the study, we assessed the association between air pollution and self-reported health separately for each of the six pollutants with each of the general health and LLTI outcomes using mixed effects generalised linear models accounting for clustering of observations within local authority areas as a random intercept. Ordinal family/logit link were used in the general health mixed-effect models and binomial family/logit link were used in the LLTI mixed-effect models. To allow comparison between the six pollutants, standardised pollutant concentrations around the mean were used in these models. The models were also adjusted for the main socio-demographic covariates and for ethnicity and country of birth variables. To account for urbanization effect and given the absence of strong correlations between SO2, ozone, and population density (Table 2), SO2 and ozone pollutant models were additionally adjusted for population density. In a sensitivity analysis, we performed standardized mixed effects tri-pollutant models examining the association of three air pollutants with health in a single model (Online Resource Table 4). We only tested tri-pollutant models formed by SO2, ozone and each other pollutant due to the high correlation between PM10, PM2.5, NO2, and CO (Table 2).
To address the third objective of the study, we added into the mixed effect models an interaction term between ethnicity and the six air pollutants and between country of birth and the six air pollutants, each at a time. Coefficient plots were used to visualize the interaction analysis results. Equations 1 and 2 provide an example of the mixed-effect models with interaction terms between air pollution and each of ethnicity and country of birth respectively; where Yij can be either the general health or the LLTI outcome; β is the slope of fixed effects; γj is a vector of random clustering; εij are the model residuals; i represents the individual; j represents the local authority.
Due to the cross-sectional design of the study and the absence of residential history data from the 2011 UK census, one main assumption that was made is that individuals did not move their place of residence from one local authority into another during the 10-years of air pollution exposure assessment. To address this limitation, we carried out a sensitivity analysis only on the sample of individuals (N = 2,347,475; 91% of the original sample) who reported that they did not change their place of residence in the year preceding the 2011 census date (Online Resource Tables 5 and 6 and Online Resource Figures 3 and 4).
Data analysis was conducted using STATA15 software for statistical modelling and ArcGIS Pro for spatial pre-processing. Regression results were reported in terms of odd ratios (ORs) and 95% confidence intervals (CIs).
Results
Descriptive Statistics and Socio-Demographics
The total sample included 2,574,360 individuals aged 16 and above. Table 3 summarises the descriptive statistics for the total sample and for Scotland (n = 219,333), England (n = 2,157,611), Wales (n = 125,596), and Northern Ireland (n = 71,820). The majority of the individuals reported having very good (40%) and good (37%) general health as well as the absence of a LLTI (79%) (Table 3). There was equal distribution of males (49%) and females (51%). Most of the individuals (40%) aged between 40 and 64 years, were married (46%), had level 3/level 4 + educational qualification (39%), and were employed in the services industry (63%) (Table 3). The majority of the total sample belonged to the White ethnicity (89%) and were born in the UK or Ireland (86%). The share of ethnic minorities was as follows: Pakistani/Bangladeshi (2%), Indians (2%), Black/African/Caribbean (3%), and other ethnicities (4%). The annual mean long-term air pollution exposure in the study population was 17.6 µg/m3 for NO2; 2.8 µg/m3 for SO2; 16.2 µg/m3 for PM10; 10.9 µg/m3 for PM2.5; and 0.2 mg/m3 for CO. As for ozone, an average of 5.9 days per year involved a daily maximum 8-h mean concentrations exceeding 120 µg/m3 (Table 3).
A high correlation (Pearson’s coefficient ≥ 0.7) was observed between NO2, PM10, PM2.5, and CO pollutants, confirming the chemical transformations and reactions between particulate matter and NO2 pollutants in the atmosphere. This was not the case for SO2 and ozone showing low to moderate correlations with each other pollutant. Yet, a low negative correlation was noted between Ozone and each of NO2, SO2, and CO pollutants (Table 2). A high correlation was also observed between population density and each of NO2, PM10, PM2.5, and CO pollutants (Table 2). As expected, this indicates higher pollutants levels in more densely populated local authority districts and council areas.
Ethnicity, Self-Reported General Health and Limiting Long Term Illness
In comparison to the White ethnic group, higher odds of poor health were observed among all ethnic minorities including Pakistani/Bangladeshi (OR = 1.71, 95%CI = 1.69–1.74), Indians (OR = 1.33, 95%CI = 1.31–1.36), Black/African/Caribbean (OR = 1.06, 95%CI = 1.04–1.07) and other ethnicities (OR = 1.19, 95%CI = 1.17–1.20). Those born outside the UK or Ireland had lower odds (OR = 0.88, 95%CI = 0.87–0.89) of having poor health as compared to those born in the UK or Ireland (Table 4; Online Resource Table 1). Similar results were observed with respect to the LLTI outcome. Higher odds of having a LLTI were observed for all ethnic minorities as compared to White, while lower odds of having a LLTI were noted for foreign-born individuals (Table 4; Online Resource Table 2).
It is also worth noting that higher odds of poor health and LLTI were observed with increasing age and among never married persons. Individuals with no educational qualification had higher odds of poor health and LLTI in comparison to those with level 1 or level 2 educational qualification; while individuals with level 3 or level 4 + education reported a better general health status and had lower odds of LLTI (Table 4; Online Resource Tables 1 and 2).
Air Pollution, Self-Reported General Health and Limiting Long Term Illness
The multivariate mixed effects models showed the presence of positive associations between self-reported general health (ranging from 1 = very good health to 5 = very bad health) and each of NO2 (OR = 1.040, 95%CI = 1.021–1.059), SO2 (OR = 1.065, 95%CI = 1.049–1.081), and CO (OR = 1.040, 95%CI = 1.024–1.055) standardized pollutant concentrations. Similarly, a significant positive association was observed between LLTI and each of NO2 (OR = 1.031, 95%CI = 1.007–1.057), SO2 (OR = 1.077, 95%CI = 1.055–1.099), and CO (OR = 1.040, 95%CI = 1.019–1.061) standardized pollutants. Higher Ozone concentrations were associated with better self-reported general health (OR = 0.932, 95%CI = 0.916–0.948) and lower odds of LLTI (OR = 0.890, 95%CI = 0.871–0.909). However, PM10 and PM2.5 pollution showed no association with general health and a slightly negative association with LLTI (Table 5).
The association between general health and each of SO2 and Ozone pollutants remained unchanged after further adjustment for population density (Table 5).
In a sensitivity analysis of tri-pollutant models formed by SO2, Ozone and each other pollutant, results remained unchanged except for NO2 and CO, which showed no association with general health and a negative association with LLTI (Online Resource Table 4). This might be related to the presence of moderate (0.5) correlation between SO2 and each of NO2 and CO pollutants (Table 2).
The Effect of Ethnicity and Country of Birth on the Association of Air Pollution with Self-Reported General Health and Limiting Long Term Illness
Table 6 summarizes the mean of air pollution by ethnicity and country of birth. Ethnic minorities and immigrants were exposed to higher levels of NO2, SO2, PM10, and PM2.5 pollution as compared to White and native-born population, while Ozone and CO exposures were constant across all ethnic groups and irrespective of the country of birth (Table 6).
The inclusion of interaction terms into the multivariate mixed effect models showed that all ethnic minorities were more likely to report poor health and LLTI than the White group with increasing concentrations of NO2, PM10, PM2.5 and CO pollutants. The highest odds of poor self-reported health and LLTI were observed among the Black/African/Caribbean group followed by the other ethnicities group. Similarly, higher odds of poor self-reported health and LLTI with increasing concentrations of NO2, PM10, PM2.5 and CO pollutants were observed among foreign-born in comparison to the UK/Ireland-born individuals (Figs. 2 and 3).
Mixed effects generalised linear models showing the interaction of standardized air pollution concentrations with each of ethnicity and country of birth in relation to self-reported general health (N = 2,574,360). The dashed line is placed at OR = 1 as a cut-off for statistically insignificant results; The solid line separates ethnicity interaction models and country of birth interaction models; The ethnicity (White as the reference group) interaction models are adjusted for country of birth, age, gender, marital status, education qualification, type of work industry, and nation (categorical variable: England, Wales, Scotland and Northern Ireland); The country of birth interaction models (Born in UK or Ireland as the reference group) are adjusted for ethnicity, age, gender, marital status, education qualification, type of work industry, and nation (categorical variable: England, Wales, Scotland and Northern Ireland)
Mixed effects generalised linear models showing the interaction of standardized air pollution concentrations with each of ethnicity and country of birth in relation to self-reported LLTI (N = 2,574,360). The dashed line is placed at OR = 1 as a cut-off for statistically insignificant results; The solid line separates ethnicity interaction models and country of birth interaction models; The ethnicity (White as the reference group) interaction models are adjusted for country of birth, age, gender, marital status, education qualification, type of work industry, and nation (categorical variable: England, Wales, Scotland and Northern Ireland); The country of birth interaction models (Born in UK or Ireland as the reference group) are adjusted for ethnicity, age, gender, marital status, education qualification, type of work industry, and nation (categorical variable: England, Wales, Scotland and Northern Ireland)
In contrast, Ozone and SO2 pollution did not show consistent associations with the general health and LLTI outcomes among ethnic minorities compared to the White group. All ethnic minorities and immigrants reported better general health with higher concentrations of SO2 as compared to White ethnicity and those born in the UK or Ireland, respectively. Similarly, lower odd ratios of limiting long-term illness were observed with higher levels of SO2 pollution among Pakistani/Bangladeshi and Black/African/Caribbean ethnicities in comparison to the White group and among immigrants in comparison to UK/Ireland born individuals. Ozone was associated with better self-reported health and lower odds of LLTI among Black/African/Caribbean versus White, yet with poor general health and higher odds of LLTI among Indians versus White (Figs. 2 and 3).
Discussion
All ethnic minorities, especially Pakistani,Bangladeshi and Indains, reported poorer general health and higher odds of LLTI in comparison to the White group. These results are concordant with the literature whereby the poorest health in the UK is often reported by people of Bangladeshi and Pakistani origin, followed by those with Caribbean and Indian descent (Nazroo, 2003). The observed health inequality could be explained by the fact that ethnic minorities often live in more disadvantaged communities, and have lower socio-economic status, lower healthcare coverage and higher job/income instability (Cézard et al., 2020; Egede, 2006; Pearce et al., 2006; Su et al., 2011). Additionally, our study showed that migrants had better health and lower odds of LLTI which is corroborated by relevant literature (Wallace & Kulu, 2015). This can be explained by the “healthy migrant effect” manifested in the influx of immigrants who have better health, higher educational levels, more wealth, and better chances to be involved in the job market (Popham, 2006; Wallace & Kulu, 2014). Migrants might also have lower risk of cardiovascular and other non-communicable diseases due to a healthier low-fat diet style, which is richer in vegatables, fruits and pulse consumption (Landman & Cruickshank, 2001).
Analysis also revealed the negative effect of long term (10-years) NO2, SO2 and CO air pollution exposure on health and LLTI, which is corroborated by the literature (Fischer et al., 2015; Hvidtfeldt et al., 2019; Miller & Xu, 2018; Renzi et al., 2017; Sanyal et al., 2018; Stafoggia et al., 2016). In contrast, Ozone pollution was associated with better self-reported health and lower odds of LLTI. This inconsistancy could be related to the high reactivity of ozone with other pollutants in the atmosphere (eg. with NO2, SO2, CO) and its seasonality (higher Ozone concentrations in the summer), which cannot be captured in yearly air pollution measurements (Hvidtfeldt et al., 2019).
Finally, our study revealed the more pronounced long-term effect of NO2, CO, PM10 and PM2.5 air pollution exposure on self-reported health and LLTI among ethnic minorities especially for the Black/African/Caribbean group and among people born outside UK/Ireland. Based on the mechanisms underlying ethnic inequalities in health discussed at the beginning of this article, the observed health differences in relation to air pollution between the ethnic groups could be attributed either to the socio-economic differences, to the individual’s living environment, or to their genetic composition. The socio-economic differences were captured in our analysis by adjusting for several important socio-economic and demographic factors including age, gender, marital status, education, and type of work industry. But ethnic health inequalities still persisted. Therefore, the place of residence may have played a role. This hypothesis was supported by the fact that migrants tended to report poorer health with increased concentrations of NO2, PM10, PM2.5 and CO pollution in comparison to the native population despite the observed “healthy migrant effect”. Additionally, our analysis showed that unlike NO2, CO, PM10, and PM2.5 pollutants, exposure to increasing concentrations of SO2 resulted in slightly better general health and lower odds of LLTI among ethnic minorities and immigrants, as compared to White and natives, respectively. This could be explained by the composition and source of air pollution emissions which is related to the residential contexts of ethnic minorities. In the UK, people from ethnic minorities such as Pakistani, Bangladeshi, Indians, and Africans often reside in urban areas, near major roads (Lucas et al., 2019), increasing their exposure to traffic-congestion pollution that involves a combination of NO2, CO, PM10, and PM2.5 emissions (Samet & Jaakkola, 1999). In contrast, SO2 comes mainly from industrial processes and power plants that involve burning of fossil fuel and that are often situated in remote areas, far from densely populated regions (Samet & Jaakkola, 1999). This was also confirmed by our descriptive analysis in Table 6, which showed a noticeable elevated exposure to NO2, PM10 and PM2.5 air pollutants among ethnic minorities and immigrants. This in turn provides further evidence that the observed ethnic inequalities in health in relation to air pollution in the UK could be mostly related to the place where ethnic minorities live besides other factors (such as lifestyle patterns and genetics). Nevertheless, further research is needed, given that the present study did not attempt to account for specific residential contexts (e.g. postcode of residence or living in rural/urban areas) of ethnic minorities and immigrants or for the individual’s genetic factors and lifestyle patterns due to the unavailability of such data.
The more pronounced effect of air pollution exposure on health among ethnic minorities is also supported by similar research from the U.S. whereby non-Hispanic blacks were on average 2 times more likely to self-report asthma and non-Hispanic Whites showed 10% higher odds of self-reported hypertension for every 10 µg/m3 increase in PM2.5 pollution (Johnson & Parker, 2009; Nachman & Parker, 2012).
Limitations of the study are as follows. First, the study design involved linking individual-level data from the 2011 UK micro-census to 10-years annual air pollution data at the local authority level. This can lead to exposure misclassifications and stationarity bias assuming that every individual within the same local authority is exposed to the same level of air pollution and assuming that individuals did not change their place of residence from one local authority to another during the 10-year time interval. This is a limitation created by the format of the 2011 micro-census data which only allows for linkages at the local authority level instead of at the postcode level and lacks information on the residential history of individuals. However, results remained unchanged in a sensitivity analysis performed on a 91% of the original sample, for individuals who reported that they did not change their place of residence in the year preceding the 2011 census date (Online Resource Tables 5 and 6 and Online Resource Figures 3 and 4). For future research, it may be preferable to use another non-stationarity dataset that offers the possibility of air pollution linkages at a higher resolution (e.g. the postcode) and that offers residential histories over a prolonged period of time.
Second, this was a cross-sectional study using a large-scale national representative census data of more than 2.5 million individuals in the UK, which was useful to visualise associations at a snapshot of time. The cross-sectional approach allowed for a high statistical power guaranteed by the huge sample of 2.5 million adult individuals (~ 5% of the UK adult population) to reveal the effect of air pollution on self-reported health and LLTI from a spatial perspective rather than a temporal perspective and to allow better generalizability of the results. Given the dynamicity and seasonality of air pollution, it would also be interesting to examine the association of air pollution with health over time using a longitudinal dataset, which we attempt to investigate in future research beyond the scope of the UK micro-census data. Longitudinal datasets that are available in the UK are either survey data (e.g. the Understanding Society: UK Household Longitudinal Survey) or cohort data based on a 1% sample of the England and Wales census (e.g. ONS data). These longitudinal datasets can reveal strong temporal patterns but sparse spatial patterns.
Third, our study assessed self-reported health, which could be overestimated when people are worried about their health status. Yet, our study used another less subjective outcome, limiting long term illness, which is more likely to be reported following a medical diagnosis. Also, the literature has shown high correlations between self-reported and objective health measures including mortality and hospital admission (Myint et al., 2006; Ul-Haq et al., 2014; Williams et al., 2017).
Lastly, we could not account in our analysis for some important lifestyle covariates considered by relevant literature such as smoking status, pre-existing co-morbidities, body-mass index, physical activity, alcohol consumption and income level due to the unavailability of these data in the 2011 UK census.
Conclusion
This study examined the association of 10-years air pollution exposure to six pollutants (NO2, SO2, PM10, PM2.5, CO, and Ozone) with self-reported general health and LLTI. Unlike other studies, we factored in the ethnicity and migration dimensions in the association of air pollution with self-reported health. Using large-scale individual-level data, this study provides evidence supporting the negative long-term effect of air pollution exposure on individuals’ self-reported health and long-term illness, with this effect being more evident among ethnic minorities and migrants, especially for people from the Black/African/Caribbean origin. Our results support the importance of the ethnic dimension in the policy making process related to air pollution and health interventions. For future research, longitudinal data are needed to further investigate how the impact of air pollution on individuals’ health varies by their ethnic origin over time.
Data Availability
The 2011 UK census microdata is publicly available by the UK Data Archive Service under the terms of the Safeguarded Open Government Licence available to registered users who have agreed to the licence conditions. For overseas users, data are only available to researchers based within the European Economic Area with data depositors’ permission.
Code Availability
Analysis code can be shared by the corresponding author upon request.
References
Ab Manan, N., Noor Aizuddin, A., & Hod, R. (2018). Effect of air pollution and hospital admission: A systematic review. Annals of Global Health, 84(4), 670–678. https://doi.org/10.9204/aogh.2376
AbedAlAhad, M., Chalak, A., Fares, S., Mardigian, P., & Habib, R. R. (2020a). Decentralization of solid waste management services in rural Lebanon: Barriers and opportunities. Waste Management & Research, 38(6), 639–648. https://doi.org/10.1177/0734242X20905115
AbedAlAhad, M., Sullivan, F., Demšar, U., Melhem, M., & Kulu, H. (2020b). The effect of air-pollution and weather exposure on mortality and hospital admission and implications for further research: A systematic scoping review. PLoS One, 15(10), e0241415. https://doi.org/10.1371/journal.pone.0241415
Abraído-Lanza, A. F., Chao, M. T., & Flórez, K. R. (2005). Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine (1982), 61(6), 1243–1255. https://doi.org/10.1016/j.socscimed.2005.01.016
Almendra, R., Santana, P., Freire, E., & Vasconcelos, J. (2016). Seasonal mortality patterns and regional contrasts in Portugal. Bulletin of Geography-Socio-Economic Series, 32(32), 7–18. https://doi.org/10.1515/bog-2016-0011
Assari, S. (2017). Race, sense of control over life, and short-term risk of mortality among older adults in the United States. Archives of Medical Science: AMS, 13(5), 1233–1240. https://doi.org/10.5114/aoms.2016.59740
Astell-Burt, T., Maynard, M. J., Lenguerrand, E., Whitrow, M. J., Molaodi, O. R., & Harding, S. (2013). Effect of air pollution and racism on ethnic differences in respiratory health among adolescents living in an urban environment. Health & Place, 23, 171–178. https://doi.org/10.1016/j.healthplace.2013.07.004
Atkinson, R. W., Carey, I. M., Kent, A. J., van Staa, T. P., Anderson, H. R., & Cook, D. G. (2015). Long-term exposure to outdoor air pollution and the incidence of chronic obstructive pulmonary disease in a national English cohort. Occupational and Environmental Medicine, 72(1), 42–48. https://doi.org/10.1136/oemed-2014-102266
Beelen, R., Stafoggia, M., Raaschou-Nielsen, O., Andersen, Z. J., Xun, W. W., Katsouyanni, K., Dimakopoulou, K., Brunekreef, B., Weinmayr, G., Hoffmann, B., Wolf, K., Samoli, E., Houthuijs, D., Nieuwenhuijsen, M., Oudin, A., Forsberg, B., Olsson, D., Salomaa, V., Lanki, T., … Hoek, G. (2014). Long-term Exposure to Air Pollution and Cardiovascular Mortality An Analysis of 22 European Cohorts. Epidemiology, 25(3), 368–378. https://doi.org/10.1097/ede.0000000000000076
Campbell, M., Marek, L., & Hobbs, M. (2021). Reconsidering movement and exposure: Towards a more dynamic health geography. Geogr Compass, 15(6), e12566. https://doi.org/10.1111/gec3.12566
Capraz, O., Efe, B., & Deniz, A. (2016). Study on the association between air pollution and mortality in Istanbul, 2007–2012. Atmospheric Pollution Research, 7(1), 147–154. https://doi.org/10.1016/j.apr.2015.08.006
Cézard, G., Finney, N., Kulu, H., & Marshall, A. (2020). Ethnic differences in self-assessed health in Scotland: The role of socio-economic status and migrant generation. Population, Space and Place, n/a(n/a), e2403. https://doi.org/10.1002/psp.2403
Charafeddine, R., & Boden, L. I. (2008). Does income inequality modify the association between air pollution and health? Environmental Research, 106(1), 81–88. https://doi.org/10.1016/j.envres.2007.09.005
Chaturvedi, N. (2001). Ethnicity as an epidemiological determinant—crudely racist or crucially important? International Journal of Epidemiology, 30(5), 925–927. https://doi.org/10.1093/ije/30.5.925
Colais, P., Faustini, A., Stafoggia, M., Berti, G., Bisanti, L., Cadum, E., Cernigliaro, A., Mallone, S., Pacelli, B., Serinelli, M., Simonato, L., Vigotti, M. A., & Forastiere, F. (2012). Particulate air pollution and hospital admissions for cardiac diseases in potentially sensitive subgroups. Epidemiology, 23(3), 473–481. https://doi.org/10.1097/EDE.0b013e31824d5a85
De Sario, M., Katsouyanni, K., & Michelozzi, P. (2013). Climate change, extreme weather events, air pollution and respiratory health in Europe. European Respiratory Journal, 42(3), 826–843. https://doi.org/10.1183/09031936.00074712
Department-for-Environment-Food-and-Rural-Affairs. (2020). Modelled background pollution data. https://uk-air.defra.gov.uk/data/pcm-data. Accessed May 2020.
Egede, L. E. (2006). Race, ethnicity, culture, and disparities in health care. Journal of General Internal Medicine, 21(6), 667–669. https://doi.org/10.1111/j.1525-1497.2006.0512.x
Evandrou, M., Falkingham, J., Feng, Z., & Vlachantoni, A. (2016). Ethnic inequalities in limiting health and self-reported health in later life revisited. Journal of Epidemiology and Community Health, 70(7), 653–662. https://doi.org/10.1136/jech-2015-206074
Faustini, A., Stafoggia, M., Renzi, M., Cesaroni, G., Alessandrini, E., Davoli, M., & Forastiere, F. (2016). Does chronic exposure to high levels of nitrogen dioxide exacerbate the short-term effects of airborne particles? Occupational and Environmental Medicine, 73(11), 772–778. https://doi.org/10.1136/oemed-2016-103666
Fischbacher, C. M., Cezard, G., Bhopal, R. S., Pearce, J., & Bansal, N. (2014). Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: Methods from the Scottish Health and Ethnicity Linkage Study (SHELS). International Journal of Epidemiology, 43(1), 129–139. https://doi.org/10.1093/ije/dyt237
Fischer, P. H., Marra, M., Ameling, C. B., Hoek, G., Beelen, R., de Hoogh, K., Breugelmans, O., Kruize, H., Janssen, N. A. H., & Houthuijs, D. (2015). Air pollution and mortality in seven million adults: The Dutch Environmental Longitudinal Study (DUELS). Environmental Health Perspectives, 123(7), 697–704. https://doi.org/10.1289/ehp.1408254
Fleury-Bahi, G., Préau, M., Annabi-Attia, T., Marcouyeux, A., & Wittenberg, I. (2015). Perceived health and quality of life: The effect of exposure to atmospheric pollution. Journal of Risk Research, 18(2), 127–138. https://doi.org/10.1080/13669877.2013.841728
Goldberg, M. S., Wheeler, A. J., Burnett, R. T., Mayo, N. E., Valois, M.-F., Brophy, J. M., & Giannetti, N. (2015). Physiological and perceived health effects from daily changes in air pollution and weather among persons with heart failure: A panel study. Journal of Exposure Science & Environmental Epidemiology, 25(2), 187–199. https://doi.org/10.1038/jes.2014.43
Hvidtfeldt, U. A., Sorensen, M., Geels, C., Ketzel, M., Khan, J., Tjonneland, A., Overvad, K., Brandt, J., & Raaschou-Nielsen, O. (2019). Long-term residential exposure to PM2.5, PM10, black carbon, NO2, and ozone and mortality in a Danish cohort. Environment International, 123, 265–272. https://doi.org/10.1016/j.envint.2018.12.010
Jiao, K., Xu, M., & Liu, M. (2018). Health status and air pollution related socioeconomic concerns in urban China. International Journal for Equity in Health, 17(1), 18. https://doi.org/10.1186/s12939-018-0719-y
Johnson, D., & Parker, J. D. (2009). Air pollution exposure and self-reported cardiovascular disease. Environmental Research, 109(5), 582–589. https://doi.org/10.1016/j.envres.2009.01.001
Kwan, M.-P. (2021). The stationarity bias in research on the environmental determinants of health. Health & Place, 70, 102609. https://doi.org/10.1016/j.healthplace.2021.102609
Landman, J., & Cruickshank, J. K. (2001). A review of ethnicity, health and nutrition-related diseases in relation to migration in the United Kingdom. Public Health Nutrition, 4(2b), 647–657. https://doi.org/10.1079/PHN2001148
Lanting, L. C., Joung, I. M. A., Mackenbach, J. P., Lamberts, S. W. J., & Bootsma, A. H. (2005). Ethnic Differences in Mortality, End-Stage Complications, and Quality of Care Among Diabetic Patients. A review. 28(9), 2280-2288. https://doi.org/10.2337/diacare.28.9.2280
Lucas, K., Stokes, G., Bastiaanssen, J., & Burkinshaw, J. (2019). Inequalities in mobility and access in the UK transport system. Future of Mobility: Evidence Review, Government Office for Science. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/784685/future_of_mobility_access.pdf. Accessed May 2020.
Miller, L., & Xu, X. (2018). Ambient PM2. 5 human health effects—Findings in China and research directions. Atmosphere, 9(11), 424. https://doi.org/10.3390/atmos9110424
Myint, P. K., Luben, R. N., Surtees, P. G., Wainwright, N. W. J., Welch, A. A., Bingham, S. A., Day, N. E., Wareham, N. J., & Khaw, K.-T. (2006). Relation between self-reported physical functional health and chronic disease mortality in men and women in the European Prospective Investigation Into Cancer (EPIC–Norfolk): A prospective population study. Annals of Epidemiology, 16(6), 492–500. https://doi.org/10.1016/j.annepidem.2005.04.005
Nachman, K. E., & Parker, J. D. (2012). Exposures to fine particulate air pollution and respiratory outcomes in adults using two national datasets: A cross-sectional study. Environmental Health, 11, 25. https://doi.org/10.1186/1476-069x-11-25
National-Records-of-Scotland. (2011). Census Microdata Individual Safeguarded Sample (Local Authority): Scotland (SN: 7835).
Nazroo, J. Y. (1998). Genetic, cultural or socio-economic vulnerability? Explaining ethnic inequalities in health. Sociology of Health & Illness, 20(5), 710–730. https://doi.org/10.1111/1467-9566.00126
Nazroo, J. Y. (2003). The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. American Journal of Public Health, 93(2), 277–284. https://doi.org/10.2105/ajph.93.2.277
Northern-Ireland-Statistics-and-Research-Agency. (2011). Census Microdata Individual Safeguarded Sample (Local Authority): Northern Ireland (SN: 7770).
Office-for-National-Statistics. (2011). Census Microdata Individual Safeguarded Sample (Local Authority): England and Wales (SN: 7682).
Office-for-National-Statistics, National-Records-of-Scotland, & Northern-Ireland-Statistics-and-Research-Agency. (2011). 2011 Census: boundary data (United Kingdom) (SN:5819). https://census.ukdataservice.ac.uk/get-data/boundary-data.aspx. Accessed May 2020.
Parker, J. D., Kravets, N., & Vaidyanathan, A. (2018). Particulate matter air pollution exposure and heart disease mortality risks by race and ethnicity in the United States. Circulation, 137(16), 1688–1697. https://doi.org/10.1161/CIRCULATIONAHA.117.029376
Pearce, J., Kingham, S., & Zawar-Reza, P. (2006). Every breath you take? Environmental justice and air pollution in Christchurch, New Zealand. Environment and Planning A: Economy and Space, 38(5), 919–938. https://doi.org/10.1068/a37446
Popham, F. (2006). Is there a "Scottish effect" for self reports of health? Individual level analysis of the 2001 UK census. BMC Public Health, 6(1), 191. https://doi.org/10.1186/1471-2458-6-191
Renzi, M., Stafoggia, M., Faustini, A., Cesaroni, G., Cattani, G., & Forastiere, F. (2017). Analysis of temporal variability in the short-term effects of ambient air pollutants on nonaccidental mortality in Rome, Italy (1998–2014). Environmental Health Perspectives, 125(6), 067019. https://doi.org/10.1289/ehp19
Riedel, N., Loerbroks, A., Bolte, G., & Li, J. (2017). Do perceived job insecurity and annoyance due to air and noise pollution predict incident self-rated poor health? A prospective analysis of independent and joint associations using a German national representative cohort study. British Medical Journal Open, 7(1), e012815. https://doi.org/10.1136/bmjopen-2016-012815
Samet, J., & Jaakkola, J. (1999). The epidemiologic approach In S. T. Holgate, J. M. Samet, H. S., Koren, & R. L. Maynard (Eds.), Air pollution and health. Academic Press, London.
Sanyal, S., Rochereau, T., Maesano, C. N., Com-Ruelle, L., & Annesi-Maesano, I. (2018). Long-Term effect of outdoor air pollution on mortality and morbidity: A 12-year follow-up study for metropolitan France. International Journal of Environmental Research and Public Health, 15(11). https://doi.org/10.3390/ijerph15112487
Schober, P., Boer, C., & Schwarte, L. A. (2018). Correlation coefficients: Appropriate use and interpretation. Anesthesia and Analgesia, 126(5), 1763–1768. https://doi.org/10.1213/ane.0000000000002864
Shin, J., Park, J. Y., & Choi, J. (2018). Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE, 13(4), e0195607–e0195607. https://doi.org/10.1371/journal.pone.0195607
Solé-Auró, A., & Crimmins, E. M. (2008). Health of immigrants in European countries. International Migration Review, 42(4), 861–876. https://doi.org/10.1111/j.1747-7379.2008.00150.x
Stafoggia, M., Zauli-Sajani, S., Pey, J., Samoli, E., Alessandrini, E., Basagana, X., Cernigliaro, A., Chiusolo, M., Demaria, M., Diaz, J., Faustini, A., Katsouyanni, K., Kelessis, A. G., Linares, C., Marchesi, S., Medina, S., Pandolfi, P., Perez, N., Querol, X., … Grp, M.-P. S. (2016). Desert dust outbreaks in Southern Europe: Contribution to daily PM10 concentrations and short-term associations with mortality and hospital admissions. Environmental Health Perspectives, 124(4), 413–419. https://doi.org/10.1289/ehp.1409164
Stronks, K., Snijder, M. B., Peters, R. J. G., Prins, M., Schene, A. H., & Zwinderman, A. H. (2013). Unravelling the impact of ethnicity on health in Europe: The HELIUS study. BMC Public Health, 13(1), 402. https://doi.org/10.1186/1471-2458-13-402
Su, J. G., Jerrett, M., de Nazelle, A., & Wolch, J. (2011). Does exposure to air pollution in urban parks have socioeconomic, racial or ethnic gradients? Environmental Research, 111(3), 319–328. https://doi.org/10.1016/j.envres.2011.01.002
Ul-Haq, Z., Mackay, D. F., & Pell, J. P. (2014). Association between self-reported general and mental health and adverse outcomes: A retrospective cohort study of 19,625 Scottish adults. PLoS One, 9(4), e93857–e93857. https://doi.org/10.1371/journal.pone.0093857
van Ham, M., & Manley, D. (2009). Social housing allocation, choice and neighbourhood ethnic mix in England. Journal of Housing and the Built Environment, 24(4), 407–422. http://www.jstor.org/stable/41107480. Accessed May 2020.
Wallace, M., & Kulu, H. (2014). Migration and health in England and Scotland: A study of migrant selectivity and salmon bias. Population, Space and Place, 20(8), 694–708. https://doi.org/10.1002/psp.1804
Wallace, M., & Kulu, H. (2015). Mortality among immigrants in England and Wales by major causes of death, 1971–2012: A longitudinal analysis of register-based data. Social Science & Medicine, 147, 209–221. https://doi.org/10.1016/j.socscimed.2015.10.060
Webster, A. L. H., Yan, M.S.-C., & Marsden, P. A. (2013). Epigenetics and cardiovascular disease. Canadian Journal of Cardiology, 29(1), 46–57. https://doi.org/10.1016/j.cjca.2012.10.023
Wiking, E., Johansson, S. E., & Sundquist, J. (2004). Ethnicity, acculturation, and self reported health. A population based study among immigrants from Poland, Turkey, and Iran in Sweden. Journal of Epidemiology and Community Health, 58(7), 574–582. https://doi.org/10.1136/jech.2003.011387
Willers, S. M., Jonker, M. F., Klok, L., Keuken, M. P., Odink, J., van den Elshout, S., Sabel, C. E., Mackenbach, J. P., & Burdorf, A. (2016). High resolution exposure modelling of heat and air pollution and the impact on mortality. Environment International, 89–90, 102–109. https://doi.org/10.1016/j.envint.2016.01.013
Williams, G., Di Nardo, F., & Verma, A. (2017). The relationship between self-reported health status and signs of psychological distress within European urban contexts. European Journal of Public Health, 27(suppl_2), 68–73. https://doi.org/10.1093/eurpub/ckx008
Zhang, K., & Batterman, S. (2013). Air pollution and health risks due to vehicle traffic. The Science of the Total Environment, 450–451, 307–316. https://doi.org/10.1016/j.scitotenv.2013.01.074
Funding
This study is part of a PhD project that was supported by the St Leonard’s interdisciplinary PhD scholarship, University of St Andrews, Scotland, UK.
Author information
Authors and Affiliations
Contributions
Mary Abed Al Ahad: Conceptualization, Methodology, Formal Analysis, Writing-Original Draft, Writing-Review and Editing, Visualization, Project administration. Hill Kulu, Frank Sullivan, Urška Demšar: Conceptualization, Funding acquisition, Supervision, Writing-Review and Editing.
Corresponding author
Ethics declarations
Ethics Approval
This study is part of a PhD project that was granted ethical approval from the School of Geography and sustainable development ethics committee, University of St Andrews, on the 14th of May 2020.
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Ahad, M.A., Demšar, U., Sullivan, F. et al. Does Long-Term Air Pollution Exposure Affect Self-Reported Health and Limiting Long Term Illness Disproportionately for Ethnic Minorities in the UK? A Census-Based Individual Level Analysis. Appl. Spatial Analysis 15, 1557–1582 (2022). https://doi.org/10.1007/s12061-022-09471-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12061-022-09471-1