Abstract
Background
Surgical repair of obstructed total anomalous pulmonary venous connection (TAPVC) is a high-risk surgical cohort. This study aimed to assess surgical risk factors and outcomes in infants with TAPVC treated at a single centre.
Methods
This was a prospective single-centre, observational study that included consecutive patients presenting with obstructed TAPVC. Patients with obstructed supra-cardiac, cardiac, and infra-cardiac TAPVC were included in the study. In-hospital mortality was the primary outcome. Multivariable logistic regression was carried out to identify risk factors for in-hospital mortality.
Results
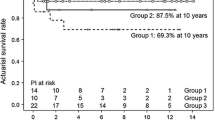
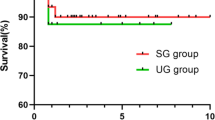
Of the 41 patients, 31 (75.6%) were males. Ages were distributed as follows: 20 (48.8%) between 1 and 3 months, 11 (26.88%) between >3 months, and 10 (24.4%) neonates. The in-hospital mortality was 19.5% (n=8). Of the remaining 33 patients, there were no deaths during the follow-up. Short-term follow-up was achieved for 100% of cases (up to 6 months post-operatively). The mean duration of follow-up was 43.6± 3.6 months. One (3%) early and 2 (6%) late pulmonary vein obstructions were observed during follow-up. Age less than 30 days and pre-operative ventilation were associated with significantly increased risk of in-hospital mortality.
Conclusions
Despite logistical challenges, reasonable surgical outcomes are attainable in obstructed TAPVC cases. Age less than 30 days and need for pre-operative ventilation were independent predictors of in-hospital mortality, while pulmonary venous obstruction in the post-operative period contributed to re-interventions.


Similar content being viewed by others
Data availability
Data is available from the corresponding author on a reasonable request.
References
Seale AN, Uemura H, Webber SA, Partridge J, Roughton M, Ho SY, et al. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Circulation. 2010;122:2718–26.
Shi G, Zhu Z, Chen J, Ou Y, Hong H, Nie Z, et al. Total anomalous pulmonary venous connection: the current management strategies in a pediatric cohort of 768 patients. Circulation. 2017;135:48–58.
Palaparthi S, Jagannath BR, Shastri R, Jayanthi K, Rao NK, Vyas S, et al. Predictors of mortality and morbidity in total anomalous pulmonary venous connection with biventricular physiology: a 10-year Indian single centre experience of 492 patients. Ann Pediatr Cardiol. 2022;15:229–37.
Bayya PR, Varghese S, Jayashankar JP, Sudhakar A, Balachandran R, Kottayil BP, et al. Total anomalous pulmonary venous connection repair: single-center outcomes in a lower-middle income region. World J Pediatr Congenit Heart Surg. 2022;13:458–65.
Imai Y, Baba K, Otsuki S, Kondo M, Eitoku T, Shigemitsu Y, et al. Stepwise treatment for heterotaxy syndrome and functional single ventricle complicated by infra-cardiac total anomalous pulmonary venous connection with ductus venosus stent placement and subsequent occlusion. Pediatr Cardiol. 2022;43:756–63.
Chowdhury UK, Airan B, Malhotra A, Bisoi AK, Saxena A, Kothari SS, et al. Mixed total anomalous pulmonary venous connection: anatomic variations, surgical approach, techniques, and results. J Thorac Cardiovasc Surg. 2008;135:106–116.e5.
Weight-for-age [Internet]. [cited 2023 Nov 28]. Available from: https://www.who.int/tools/child-growth-standards/standards/weight-for-age
Tucker BL, Lindesmith GG, Stiles QR, Meyer BW. The superior approach for correction of the supracardiac type of total anomalous pulmonary venous return. Ann Thorac Surg. 1976;22:374–7.
Nag P, Chowdhury SR, Behera SK, Das M, Narayan P. Levosimendan or milrinone for ventricular septal defect repair with pulmonary arterial hypertension. J Cardiothorac Vasc Anesth. 2023;37:972–9.
Harada T, Nakano T, Oda S, Kado H. Surgical results of total anomalous pulmonary venous connection repair in 256 patients. Interact Cardiovasc Thorac Surg. 2019;28:421–6.
Jinghao Z, Botao G, Zhiwei X, Jinfeng L. The research on operation of obstructed total anomalous pulmonary venous connection in neonates. Sci World J. 2014;2014:576569.
Kelle AM, Backer CL, Gossett JG, Kaushal S, Mavroudis C. Total anomalous pulmonary venous connection: results of surgical repair of 100 patients at a single institution. J Thorac Cardiovasc Surg. 2010;139:1387-1394.e3.
Zhao K, Wang H, Wang Z, Zhu H, Fang M, Zhu X, et al. Early- and intermediate-term results of surgical correction in 122 patients with total anomalous pulmonary venous connection and biventricular physiology. J Cardiothorac Surg. 2015;10:172.
Karaci AR, Harmandar B, Aydemir NA, Sasmazel A, Balci AY, Saritas T, et al. Early and intermediate term results for surgical correction of total anomalous pulmonary venous connection. J Card Surg. 2012;27:376–80.
DeLeon MM, DeLeon SY, Roughneen PT, Bell TJ, Vitullo DA, Cetta F, et al. Recognition and management of obstructed pulmonary veins draining to the coronary sinus. Ann Thorac Surg. 1997;63:741–4.
Hote MP, Garg S, Choudhury M, Raghu MG. Open vertical vein in non-obstructed supracardiac TAPVC: merits and fate. Asian Cardiovasc Thorac Ann. 2012;20:114–9.
Caspi J, Pettitt TW, Fontenot EE, Stopa AR, Heck HA, Munfakh NA, et al. The beneficial hemodynamic effects of selective patent vertical vein following repair of obstructed total anomalous pulmonary venous drainage in infants. Eur J Cardiothorac Surg. 2001;20:830–4.
Shah MJ, Shah S, Shankargowda S, Krishnan U, Cherian KM. L–>R shunt: a serious consequence of TAPVC repair without ligation of vertical vein. Ann Thorac Surg. 2000;70:971–3.
Cheung YF, Lun KS, Chau AKT, Chiu CSW. Fate of the unligated vertical vein after repair of supracardiac anomalous pulmonary venous connection. J Paediatr Child Health. 2005;41:361–4.
Devendran V, Wilson N, Jesudian V. Percutaneous closure of a large unligated vertical vein using the Amplatzer Vascular Plug II after supracardiac total anomalous pulmonary venous connection (TAPVC) repair. Pediatr Cardiol. 2013;34:1976–8.
Azakie A, Lavrsen MJ, Johnson NC, Sapru A. Early outcomes of primary sutureless repair of the pulmonary veins. Ann Thorac Surg. 2011;92:666–71.
Wu Y, Xin L, Zhou Y, Kuang H, Jin X, Li Y, et al. Is sutureless technique beneficial in the primary repair of total anomalous pulmonary venous connection? A systematic review and meta-analysis. Pediatr Cardiol. 2019;40:881–91.
Hung DQ, Huy DX, Vo HL, Hien NS. Factors associated with early postoperative results of total anomalous pulmonary venous connection repair: findings from retrospective single-institution data in Vietnam. Integr Blood Press Control. 2021;14:77–86.
Funding
None.
Author information
Authors and Affiliations
Contributions
AS: contributed towards data acquisition, revising the manuscript, and approval of the final version.
BP: contributed towards data acquisition, illustrations, data analysis, writing and revising the manuscript, and approval of the final version.
MD: contributed towards modification of the draft and approval of the final version.
SKB: contributed towards the conception of the study, revising the manuscript, and approval of the final version.
AC: contributed towards modification of the draft and approval of the final version.
PN: contributed towards the conception of the study, writing and revising the manuscript, analysing the data, and approval of the final version.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained (-EC/AP/48-2014). The study was carried out in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Obtained.
Conflict of interest
The author declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Samaddar, A., Purkayastha, B., Das, M. et al. Risk factors and outcomes for surgical repair of obstructed total anomalous pulmonary venous connection. Indian J Thorac Cardiovasc Surg 40, 318–326 (2024). https://doi.org/10.1007/s12055-024-01690-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-024-01690-0