Abstract
Vascular graft/endograft infection (VGEI) is a constant in cardiovascular surgery with published rates between 1 and 5%. Every graft type and anatomical location is a potential target for infectious complications. These patients are sick patients with high frailty burden. Management of VGEI entails a multidisciplinary and multimodality approach. Here we review some aspects of the problem of VGEI including prevention, diagnosis, and surgical therapy with focus on recent developments in the field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is a known fact that any implant placed in the human body is susceptible to presenting complications immediately after the intervention, of whatever type, or during the follow-up of the patient, that is, during his/her lifespan. This is an old story and may eventually develop at any patient age and, as said, after any type of implant [1, 2]. Antibiotic prophylaxis before any implant is currently accepted as routine surgical practice. The goal of administering antibiotics before an operation is having the highest concentration in tissues at the time of the initiation and during surgery [3, 4] and thus reducing the risk of infections that may develop postoperatively.
Infection is a bad traveling companion for the surgeon regardless of the specialty. This is because of the high morbidity and mortality related to any infection starting with surgical site infection [5, 6]. There is mounting evidence supporting the routine preoperative antibiotic prophylaxis in surgery and especially when an implant is contemplated [7]. This, of course, also applies to cardiovascular surgery [8, 9]. In this contribution, we will address the significance and current approaches to vascular graft and endograft infection (VGEI) due to the potential catastrophic consequences of these aggressive infections.
Methods
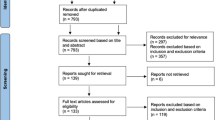
This is a narrative review in which concepts and articles related to VGEI that should be of interest for practising cardiovascular surgeons and allied professionals with experience and expertise are considered. Topics include current knowledge, prevention and diagnosis, and replacement materials used in vascular practice. Search terms included “vascular graft”, “infection”, “surgery”, and “antimicrobial therapy”. Historical and contemporary articles have been selected to understand developments in the field. For practical purposes, focus has been placed on intrathoracic prostheses.
The knowledge
VGEIs are uncommon, at an estimated 1–3% reported rate after open surgical implantation. Mortality is high, in the range of 20–30% [10, 11]. Although infection rates may change according to series, VGEI of any location is a potentially lethal entity. In addition to this high toll, it is associated with relevant health costs [12, 13].
The questions
There are two main questions when it comes to VGEI. The first question: when does the infection occur? There is evidence that VGEI starts preoperatively by inoculation with bacteria from the patient’s skin flora at the time of surgery. This has been well addressed by Hasse et al. [10] and Van Hemelrijck et al. [14]. This is particularly significant in the case of prosthetic vascular graft infection (VGI) in the groin due to surgical site infection [10] and continues to be a major issue in vascular surgery.
Well-known risk factors for VGEIs include groin incisions, wound infections, and comorbidities typical of patients with vascular disease. Modifiable predictors for VGEIs as targets for infection prevention strategies have been well addressed by Anagnostopoulos et al. in a recent seminal contribution [15]. In their prospective Swiss Vascular Graft Infection Cohort (VASGRA), they analyzed 438 predominantly male (83.1%) patients with a median age of 71 years totalling 554 person/years of follow-up. The authors identified incisional surgical site infections, hemorrhage, renal insufficiency, inadequate perioperative prophylaxis, and procedural time increases of 1-h intervals to be risk factors for VGEIs. These data confirm that several postsurgical infectious and non-infectious complications are modifiable predictive factors for VGEIs. This is relevant information [15].
The second question: What are VGIs? This has generated discussion over the past four decades. It is known that VGIs are biofilm-associated infections. Costerton et al. [16] confirmed the basic description of a biofilm which consists of single cells and microcolonies of sister cells embedded in a highly hydrated matrix including bacterial exopolymers and foreign macromolecules. The biofilm recruits bacteria resulting in further adherence [16].
VGEIs are then the result of a variety and diversity of factors of which intraoperative have a prominent role [14]. Biofilm has a fundamental role in the pathogenesis of VGEI and current research focus on how to prevent biofilm formation and how to chemically penetrate existing biofilms [17].
Characteristics of VGIs
VGEIs share some characteristics.
-
1.
They are common to all graft positions.
-
2.
They have indolent pathogenic patterns with alternance of acute and quiescent periods.
-
3.
They have an initial good response to antibiotic therapy; however, relapses are frequent because bacteria in biofilms are protected from antibiotics. As these bacterial foci go uncontrolled, the graft or device must be removed.
-
4.
These infections are often polymicrobial, at least 30%. The predominant bacteria are autochthonous skin or bowel flora or common environmental microorganisms which are frequently pathogenic in immunocompromised patients [18].
-
5.
Bacteria may not be easy to recover from fluids/tissues adjacent to grafts/devices.
Evidence-based knowledge
Although there is substantial information accumulated in the literature, there still is no solid consensus on a number of aspects related to VGEI such as terminology, definition, classification, diagnostic criteria, and reporting standards. Complexity is a main issue in VGEI and it is frequently difficult to establish an accurate diagnosis and deciding which the best line of treatment is. In the case of intrathoracic VGEIs, the intrinsic risk of patients with VGI is usually the highest for the surgical patient. Due to the nature of the problem, there are no controlled studies and there is always mixed information coming from mixed territories. It is to be noticed that Clinical Practice Guidelines have not been issued until the last decade [11, 19, 20]. Part of the information is still being gathered from systematic reviews or Delphi Consensus documents [21, 22]. This once more highlights the difficulties of the clinicians when facing the problem of VGEI at any location. Furthermore, a large proportion of recommendations is of low level of evidence. Although useful information is being collected still at a low pace, the underlying message is that VGEI must include targeted antimicrobial therapy, radical debridement, and eventually prosthetic graft removal [10, 14]. The level of evidence is low as regards the best therapy and the replacement material.
Prevention
As of today, and as stated above, current knowledge contemplates debridement, negative pressure wound therapy (NPWT) with continuous irrigation of the infected field. Reconstructive therapy whenever possible and systemic therapy were the options for management of VGEIs [10, 14]. It seems that there is a relationship between infection of the surgical site and prosthetic graft infection. Multiple approaches to prevent surgical site and graft infection have been tested in the laboratory setting and in clinical practice aiming at avoiding severe surgical trauma in already sick patients. Ikeno et al. proposed NPWT until system and regional negative cultures are achieved followed by reconstruction of the chest wall [23]. Conservative therapy has also been advocated by others [24, 25] in this setting. A major issue here is always reduction of bacterial load [26].
Having said that, prevention should start before something occurs, which may sound a bit naive. A major issue is if the prosthetic graft is itself a risk factor for postoperative infection. There are a number of issues to consider; first, the use of topical antibiotics as it has been advocated in the past may lead to bacterial resistance. This is a very old controversy active for over four decades [27]. Even today and although there is more literature available on surgical access through the groin, heterogeneity as regards access is a problem and there is paucity of data to support routine topical administration in surgical accesses [28].
Second, there is lack of robust long-term follow-up data on infection-free survival. Some mid-term outcomes in small-sized cohorts suggest that specific hybrid options in selected patients may yield safe outcomes for the treatment of infected vascular reconstructions [29]. More information is required over long periods of time to understand the eventual value of preventive measures of any kind on VGEI.
Third, studies focused on the use of antibiotic-bonded grafts to reduce the risk of VGEIs in vitro and in vivo. In large animal models, antimicrobial-bonded vascular graft material outperformed standard vascular grafts as regards graft patency and infection [30]. This animal study showed that their specific antibiotic composition with minocycline and rifampin with chlorhexidine precoating resisted to Staphylococcus aureus and limited the growth of Pseudomonas aeruginosa. However, clinical experience is heterogenous and diverse surveys show mixed opinions about preventive usage of antibiotic-bonded grafts [31, 32]. Furthermore, S. aureus has been shown to colonize rifampin-bonded grafts 7 days after implantation [33].
To further investigate the eventual role of the type of prosthesis and as part of previous work, an in vitro study was organized at the University Hospital Zurich, Switzerland, to compare the susceptibility of two thoracic vascular woven polyester grafts with different coatings to biofilm formation [34]. Implanted grafts are usually coated with proteinaceous solutions only, for quick integration into the host tissue. A collagen and a gelatin graft were compared. The collagen graft was coated with a highly purified form of cross-linked bovine type I collagen and the gelatin graft coated with a modified mammalian gelatin. The resorption time for collagen is 4–8 weeks and for gelatin, 14 days. In these in vitro experiments, grafts were dissected into small square pieces and were inoculated with bacterial strains representing pathogens implicated in thoracic VGEI from a patient cohort. Biofilm grown on collagen graft patches displayed increased total biofilm mass volume and maximal biofilm height, those finding supporting the potential of Gram-positive bacteria to adhere to collagen. Only minor affinity was observed for gelatin [34].
The in vivo study included 412 patients from the VASGRA cohort [10, 15]. Out of them, 28 developed intrathoracic VGI. The calculated percentage of intracavitary VGI was higher for patients in the collagen graft group [34]. Although there were some limitations intrinsic to the laboratory methodology, biofilm formation was increased on collagen-coated grafts in comparison with gelatin-coated. This may entail that graft material may be associated with a given VGI rate.
Diagnosis
Over the past five decades, there has been abundant though heterogeneous literature on the topic of VGEI although as said earlier, recommendations and practice guidelines have been published in recent years due to the difficulties in organized controlled studies due to the complexity of the topic. The difficulties in diagnosis are multiple, from the protean manifestations of vascular infection to the various imaging methods available over time [35].
The diagnosis of VGEI is still a challenge for the practitioners as there are not clearly agreed standards. The diagnosis is established on some clinical and radiological criteria [36] and frequently the diagnosis is delayed which takes a toll on outcomes. Due to the lack of pre-established and validated criteria for VGI, some attempts have been made to extrapolate knowledge from other areas such as prosthetic valve endocarditis to VGEI [14, 37]. Very recently, a new case definition considering also major and minor criteria was proposed by the Management of Aortic Graft Infection Collaboration (MAGIC) [38]. The MAGIC criteria are meant to be a diagnostic standard for VGEI and have been well received by the community. Anagnostopoulos et al. [39] validated the MAGIC criteria by retrospectively evaluating the adjudicated VASGRA infection status [10]. Assuming the intrinsic limitations of a retrospective evaluation, it was found that the current MAGIC criteria offer good sensitivity and specificity in the context of infections; however, there was a slightly poorer sensitivity in VGEI than in other locations. The MAGIC criteria will in any case be a good tool for comparison of different management strategies [38].
Although the first-choice imaging modality is computed tomography [36], nuclear medicine methods such as positron emission tomography with 2-deoxy-2-[fluorine-18] fluoro-d-glucose, positron emission tomography, computed tomography (18F-FDG-PET/CT) are reliable non-invasive imaging modality for the diagnosis of primary vascular infection and VGEI [40] (Fig. 1). This has been confirmed over the years as PET/CT has added accuracy to the diagnosis of suspected vascular infection [41] and produced altering information in the therapy control of infective aneurysms [42] or established VGEIs [43]. Apparently, the diagnostic accuracy of 18F-FDG-PET/CT is higher than the accuracy of contrast-enhanced computed tomography (CE-CT) and demonstrates excellent sensitivity. The capacities of 18F-FDG-PET/CT beyond the actual body of a potentially infected graft are currently being explored and the role of abnormal locoregional lymph nodes in the diagnosis considered. According to van Rijsewijk et al., detection of abnormal nodes has a high specificity and positive predictive value for VGEI thus producing additional relevant information that might be incorporated as part of diagnostic criteria in the future [44].
Antibiotic therapy
Antibiotic therapy is a major component of the management scheme in any major infection such as VGEI. Although guidelines provide strong recommendations in the case of infective endocarditis, a major bloodborne infection [45], unfortunately this is not the case in VGEI. One can then say that there are no universal recommendations on the usage of specific antibiotics for a given case of infection [14]. In our own experience [18], around one-third of VGI is polybacterial, meaning that both Gram-positive and Gram-negative pathogens should be tackled through a broad-spectrum combination of intravenous antibiotics until an accurate microbiological diagnosis is made; quite frequently this is not possible as all cultures may yield negative results. In the case of intrathoracic VGEI as we mostly refer here to, the combination of a beta-lactam (e.g., ampicillin-cloxacillin)/glycopeptide (e.g., vancomycin) and an aminoglycoside (e.g., gentamicin) [14]. The European and North American clinical practice guidelines produce slightly different recommendations according to the extent of resection and debridement as regards duration of antibiotic therapy [11, 19].
Regarding timing for surgery, the same problems as with which type and duration of therapy exist. The condition of the patient will dictate if a patient is eventually fit for surgery although clinical presentation will guide the treating team towards the most appropriate time to indicate a reoperative procedure of any kind. The case of, for instance, an aortoenteric fistula is clearly a surgical indication and the patient should be treated without major delay, unless specific contraindication is present.
Replacement material
There have been different opinion streams as regards the value and role of a diversity of graft materials in vascular surgery and especially in the field of VGEIs. Currently, commercially available prosthetic grafts and vascular devices are mainly made of two different materials such as polymers, polyethylene terephthalate (PET) (Fig. 2) and expanded polytetrafluoroethylene (ePTFE), and different alloys, nitinol being the most used worldwide [19]. Little has been investigated as regards potential infectability of these materials, which are chosen because of their chemical and mechanical properties [17, 34, 46]. Comparative studies in graft infections yielded conflictive results as different models have been used. Rowe et al. created a porcine model of thoracic aortic graft infection [47] to compare the ability of cryopreserved arterial allografts (CAA) to resist infection in comparison with collagen-impregnated Dacron grafts (CIDG). Animals received S. aureus boluses and were euthanized after 8 weeks. Interestingly, in this animal model, CIDG has an infection rate of 16.7% and cryopreserved allografts 57.2%, although there were no statistically significant differences. On the other hand, Vogt et al. in a series of 72 patients suffering from different types of vascular infection compared the outcomes of CAA with conventional vascular prostheses [48]. The use of CAA was more effective in the treatment of mycotic aneurysms and infected vascular prostheses in terms of disease-related survival, disease-related survival free of reoperation, hospitalization, duration of antibiotic therapy, and elimination of infection at 5 years postoperatively. The use of CAA offers a promising solution in thoracic and thoracoabdominal infection due to their apparently superior resistance to infection although they are not free from late complications [18, 49,50,51]. However, it is still unclear if there is a superior replacement option on the long-term [52].
Intraoperative view after second reoperation for infection of an ascending aorta prosthetic graft. In a complex procedure, the patient underwent aortic root re-replacement with a prosthetic valved conduit requiring coronary management with separate 10-mm prosthetic grafts to the left and the right coronary arteries (1). Distal to the prosthetic graft, a self-made xenopericardial tube was used to reach the aortic arch (2). The patient had a previous Cabrol fistula to the right atrium (fine arrow) from an explanted mediastinal patch (3)
A newer surgical concept was introduced and discussed for the treatment of thoracic and abdominal graft infections. Czerny et al. evaluated the use of self-made xenopericardial tube grafts constructed from a patch [52] in an initial series of 15 patients with VGEI. Two years postoperatively, freedom from reinfection and reoperation was 100%. The authors concluded that these xenopericardial tube grafts as neoaortic segments produced good results and represented an alternative to CAA. Additional information was released in 2018 by Kreibich et al. [53] and confirmed the same initial results. Perioperative mortality in all these series is still high considering the frail state of patients with VGEI; the concept has been validated across different series with focus on the thoracic and thoracoabdominal aorta with proven promising data in the short-term [54,55,56] regarding freedom from reinfection and graft durability. Additional data with focus on follow-up structural issues are mandatory.
Adjunctive procedures in the case of VGI
The role of adjunctive procedures is still unclear and controversial as of today. Some of them have been advocated in the literature for long time; however, no consensus has been reached with this regard. The greater omentum is a highly vascularized tissue, being directly supplied from the right and left gastroepiploic arteries and has been used in a number of different procedures in the abdomen and in the chest. The greater omentum has been reported as a major and useful barrier against infection in abdominal and thoracic aneurysm surgery. In line with this assumption, wrapping of grafts has been advocated to prevent infection [57]. In any case, the greater omentum is a versatile biological material that can be used in complex thoracic and abdominal conditions including VGI [58].
Muscle flaps have been used in a variety of reconstructive procedures and also to treat VGI being this an old story [59]. Muscle flaps have been transferred mainly to the inguinal regions to cover wounds and/or vascular grafts with excellent results in terms of graft salvage [60, 61].
Limitations
This is just a narrative review of the literature with no systematic search. This may have influence on opinions.
Conclusions
VGI is a serious condition that entails high morbidity and mortality. Despite advancements in the field, there is still lack of consensus as regards the type of replacement material. Prevention of VGEI is complex as several pre- and intraoperative factors play a role in the pathogenesis of prosthetic infection. Advances in diagnosis that include nuclear medicine techniques seem to help in the diagnosis of VGEI and have gained momentum in the past decade. There is a need to collect larger series with prolonged follow-up.
References
Dietz J, Zeidler A, Wienke A, Zeh A, Delank KS, Wohlrab D. Periprosthetic infection after total hip replacement: risk factors for an early infection after primary implantation. Orthopadie (Heidelb). 2022;51:969–75.
Vaghela HM, Capper R, Gibbin KP. Infections following cochlear implantation. Cochlear Implants Int. 2003;4:148–55.
W-Dahl A, Robertsson O, Stefánsdóttir A, Gustafson P, Lidgren L. Timing of preoperative antibiotics for knee arthroplasties. Improving the routines in Sweden. Patient Saf Surg. 2011;5:22. https://doi.org/10.1186/1754-9493-5-22.
Tarchini G, Liau KH, Solomkin JS. Antimicrobial stewardship in surgery: challenges and opportunities. Clin Infect Dis. 2017;64:S112–4.
Zukowska A, Zukowski M. Surgical site infection in cardiac surgery. J Clin Med. 2022;11:6991. https://doi.org/10.3390/jcm11236991.
Sorour AA, Kirksey L, Ambur V, Bena J. Surgical site complications after complex iliofemoral reconstruction and the role of negative pressure wound therapy: a retrospective, single-center study. Wounds. 2022;34:E22–8.
AlBuhairan B, Hind D, Hurtchison A. Antibiotic prophylaxis for wound infections in total joint arthroplasty: a systematic review. J Bone Joint Surg Br. 2008;90:915–9.
de Tymowski C, Sahnoun T, Provenchere S, Para M, Derre N, Mutuon P, et al. Impact of antibiotic prophylaxis on surgical site infections in cardiac surgery. Antibiotics (Basel). 2023;12:85.
Burzyńska J, Jaworski R, Maruszewski B, Kansy A, Dzierżanowska-Fangrat K. Perioperative antibiotic prophylaxis in pediatric cardiac surgery-simple is better. Antibiotics (Basel). 2022;12:66.
Hasse B, Husmann L, Zinkernagel A, Weber R, Lachat M, Mayer D. Vascular graft infections. Swiss Med Wkly. 2013;143: w13754. https://doi.org/10.4414/smw.2013.13754.
Wilson WR, Bower TC, Creager MA Amin-Hanjani S, O’Gara PT, Lockhart PB et al; American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Surgery and Anesthesia; Council on Peripheral Vascular Disease; and Stroke Council. Vascular graft infections, mycotic aneurysms, and endovascular infections: a scientific statement from the American Heart Association. Circulation. 2016;134:e412–e460.
Bandyk DF. Vascular surgical site infection: risk factors and preventive measures. Semin Vasc Surg. 2008;21:119–23.
Mponponsuo K, Chew D, Lu S, Somayaji R, Rennert-May E. Differences in outcomes for hospitalizations of systemic and non-systemic infections associated with vascular and cardiac grafts and devices: a population-based study. J Hosp Infect. 2020;106:828–34.
Van Hemelrijck M, Sromicki J, Husmann L, Rancic Z, Hasse B, Carrel TP. Vascular graft infections. Vessel Plus. 2022;6:47.
Anagnostopoulos A, Ledergerber B, Kuster SP, Scherrer AU, Näf B, Greiner MA; VASGRA Cohort Study. Inadequate perioperative prophylaxis and postsurgical complications after graft implantation are important risk factors for subsequent vascular graft infections: prospective results from the Vascular Graft Infection Cohort Study. Clin Infect Dis. 2019;69:621–630.
Costerton JW, Cheng KJ, Geesey GG, Ladd TI, Nickel JC, Dasgupta M, et al. Bacterial biofilms in nature and disease. Annu Rev Microbiol. 1987;41:435–64.
Lejay A, Chakfe N. Biofilm is the target: commentary on: “a narrative review of experimental assessment to study vascular biomaterials infection and infectability.” EJVES Vasc Forum. 2023;59:22–3.
Mestres CA, Quintana E, Kopjar T, Ambrosioni J. Almela M, Fuster D et al. Hospital Clinic Infective Endocarditis Investigators. Twenty-year experience with cryopreserved arterial allografts for vascular infections. Eur J Cardiothorac Surg. 2019;55:358–365.
Chakfé N, Diener H, Lejay A, Assadian O, Berard X, Caillon J et al. ESVS Guidelines Committee. Editor’s choice - European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur J Vasc Endovasc Surg. 2020;59:339–384.
Lauri C, Signore A, Glaudemans AWJM, Treglia G, Gheysens O, Slart RHJA, et al. Evidence-based guideline of the European Association of Nuclear Medicine (EANM) on imaging infection in vascular grafts. Eur J Nucl Med Mol Imaging. 2022;49:3430–51.
Kahlberg A, Grandi A, Loschi D, Vermassen F, Moreels N, Chakfé N, et al. A systematic review of infected descending thoracic aortic grafts and endografts. J Vasc Surg. 2019;69:1941–51.
Sörelius K, Wyss TR; Academic Research Consortium of Infective Native Aortic Aneurysm (ARC of INAA). Editor’s choice - Infective native aortic aneurysms: a Delphi Consensus document on terminology, definition, classification, diagnosis, and reporting standards. Eur J Vasc Endovasc Surg. 2023;65:323–329.
Ikeno Y, Sakakibara S, Yokawa K, Kitani K, Nakai H, Yamanaka K, et al. Post-sternotomy deep wound infection following aortic surgery: wound care strategies to prevent prosthetic graft replacement†. Eur J Cardiothorac Surg. 2019;55:975–83.
Kouijzer IJE, Baranelli CT, Maat I, van den Heuvel FMA, Aarntzen EHJG, Smith T, et al. Thoracic aortic vascular graft infection: outcome after conservative treatment without graft removal. Eur J Cardiothorac Surg. 2022;63:ezac551. https://doi.org/10.1093/ejcts/ezac551.
Cole SH, Wagner RD, Volk AS, Nemec MK, Preventza OA, de la Cruz K, et al. Thoracic aortic graft salvage after sternal wound infection with antibiotic beads and flap coverage. Plast Reconstr Surg Glob Open. 2022;10: e4371. https://doi.org/10.1097/GOX.0000000000004371.
Okita Y. Let us make a reduction of bacteria. Eur J Cardiothorac Surg. 2022;63:ezad012. https://doi.org/10.1093/ejcts/ezad012.
Pitt HA, Postier RG, MacGowan AW, Frank LW, Surmak AJ, Sitzman JV, et al. Prophylactic antibiotics in vascular surgery. Topical, systemic, or both? Ann Surg. 1980;192:356–64.
Robbins JM, Courtney J, Hingorani A. Systematic review of groin incision surgical site infection preventative measures in vascular surgery. J Vasc Surg. 2023;77:1835–50.
Thorbjørnsen K, DjavaniGidlund K, Björck M, Kragsterman B, Wanhainen A. Editor’s choice - Long-term outcome after EndoVAC hybrid repair of infected vascular reconstructions. Eur J Vasc Endovasc Surg. 2016;51:724–32.
Clemens MS, Stull MC, Hata KW, Heafner TA, Watson DB, Arthurs ZM, et al. Antimicrobial-bonded graft patency in the setting of a polymicrobial infection in swine (Sus scrofa). J Vasc Surg. 2017;66:1210–6.
Berger P, De Borst GJ, Moll FL. Current opinions about diagnosis and treatment strategy for aortic graft infections in The Netherlands. J Cardiovasc Surg (Torino). 2015;56:867–76.
Kirkham AM, Candeliere J, McIsaac DI, Stelfox HT, Dubois L, Gill HL, et al. Efficacy of strategies intended to prevent surgical site infection after lower limb revascularization surgery: a systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2023. https://doi.org/10.1097/SLA.0000000000005867.
Schmacht D, Armstrong P, Johnson B, Pierre K, Back M, Honeyman A, et al. Graft infectivity of rifampin and silver-bonded polyester grafts to MRSA contamination. Vasc Endovascular Surg. 2005;39:411–20.
Schweizer TA, Shambat SM, Haunreiter VD, Mestres CA, Weber A, Maisano F, et al. Polyester vascular graft material and risk for intracavitary thoracic vascular graft infection. Emerg Infect Dis. 2020;26:2448–52.
O’Brien T, Collin J. Prosthetic vascular graft infection. Br J Surg. 1992;79:1262–7.
Arnon-Sheleg E, Keidar Z. Vascular graft infection imaging. Semin Nucl Med. 2023;53:70–7.
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–8.
Lyons OTA, Baguneid M, Barwick TD, Bell RE, Foster N, Homer-Vanniasnkam S, et al. Diagnosis of aortic graft infection: a case definition by the Management of Aortic Graft Infection Collaboration (MAGIC). Eur J Vasc Endovasc Surg. 2016;52:758–63.
Anagnostopoulos A, Mayer F, Ledergerber B, Bergadà-Pijuan J, Husmann L, Mestres CA et al. VASGRA Cohort Study. Editor’s choice - Validation of the Management of Aortic Graft Infection Collaboration (MAGIC) criteria for the diagnosis of vascular graft/endograft infection: results from the prospective Vascular Graft Cohort Study. Eur J Vasc Endovasc Surg. 2021;62:251–257.
Keidar Z, Engel A, Hoffman A, Israel O, Nitecki S. Prosthetic vascular graft infection: the role of 18F-FDG PET/CT. J Nucl Med. 2007;48:1230–6.
Husmann L, Huellner MW, Ledergerber B, Eberhard N, Kaelin MB, Anagnostopoulos A et al; Vasgra Cohort. Diagnostic accuracy of PET/CT and contrast enhanced CT in patients with suspected infected aortic aneurysms. Eur J Vasc Endovasc Surg. 2020;59:972–981.
Husmann L, Huellner MW, Eberhard N, Ledergerber B, Kaelin MB, Anagnostopoulos A, et al. PET/CT in therapy control of infective native aortic aneurysms. Sci Rep. 2021;11:5065. https://doi.org/10.1038/s41598-021-84658-z.
Husmann L, Eberhard N, Huellner MW, Ledergerber B, Mueller A, Gruenig H, et al. Impact of unknown incidental findings in PET/CT examinations of patients with proven or suspected vascular graft or endograft infections. Sci Rep. 2021;11:13747. https://doi.org/10.1038/s41598-021-93331-4.
van Rijsewijk ND, Helthuis JHG, Glaudemans AWJM, Wouthuyzen-Bakker M, Prakken NHJ, Liesker DJ, et al. Added value of abnormal lymph nodes detected with FDG-PET/CT in suspected vascular graft infection. Biology (Basel). 2023;12:251. https://doi.org/10.3390/biology12020251.
Delgado V, Ajmone Marsan N, de Waha S, Bonaros N, Brida M, Burri H et al; ESC Scientific Document Group. 2023 ESC guidelines for the management of endocarditis. Eur Heart J. 2023:ehad193. https://doi.org/10.1093/eurheartj/ehad193.
Puges M, M’Zali F, Pereyre S, Bébéar C, Cazanave C, Bérard X. A narrative review of experimental assessment to study vascular biomaterials infections and infectability. EJVES Vasc Forum. 2023;59:49–55.
Rowe NM, Impellizzeri P, Vaynblat M, Lawson NM, Kim YD, Sierra M, et al. Studies in thoracic aortic graft infections: the development of a porcine model and a comparison of collagen-impregnated dacron grafts and cryopreserved allografts. J Thorac Cardiovasc Surg. 1999;118:857–65.
Vogt PR, Brunner-La Rocca HP, Carrel T, von Segesser LK, Ruef C, Debatin J, et al. Cryopreserved arterial allografts in the treatment of major vascular infection: a comparison with conventional surgical techniques. J Thorac Cardiovasc Surg. 1998;116:965–72.
MingaLowampa E, Holemans Ch, Stiennon L, Van Damme H, Defraigne JO. Late fate of cryopreserved arterial allografts. Eur J Vasc Endovasc Surg. 2016;52:696–702.
Heo SH, Kim YW, Woo SY, Park YJ, Kim DK, Chung DR. Recent results of in situ abdominal aortic reconstruction with cryopreserved arterial allograft. Eur J Vasc Endovasc Surg. 2017;53:158–67.
Couture T, Gaudric J, Davaine JM, Jayet J, Chiche L, Jarraya M, et al. Results of cryopreserved arterial allograft replacement for thoracic and thoracoabdominal aortic infections. J Vasc Surg. 2021;73:626–34.
Czerny M, von Allmen R, Opfermann P, Sodeck G, Dick F, Stellmes A, et al. Self-made pericardial tube graft: a new surgical concept for treatment of graft infections after thoracic and abdominal aortic procedures. Ann Thorac Surg. 2011;92:1657–62.
Kreibich M, Siepe M, Morlock J, Beyersdorf F, Kondov S, Scheumann J, et al. Surgical treatment of native and prosthetic aortic infection with xenopericardial tube grafts. Ann Thorac Surg. 2018;106:498–504.
Weiss S, Tobler EL, von Tengg-Kobligk H, Makaloski V, Becker D, Carrel TP, et al. Self made xeno-pericardial aortic tubes to treat native and aortic graft infections. Eur J Vasc Endovasc Surg. 2017;54:646–52.
Carrel T, Englberger L, Schmidli J. How to treat aortic graft infection? With a special emphasis on xeno-pericardial aortic tube grafts. Gen Thorac Cardiovasc Surg. 2019;67:44–52.
Alonso W, Ozdemir B, Chassin-Trubert L, Ziza V, Alric P, Canaud L. Early outcomes of native and graft-related abdominal aortic infection managed with orthotopic xenopericardial grafts. J Vasc Surg. 2021;73:222–31.
Yamashiro S, Arakaki R, Kise Y, Inafuku H, Kuniyoshi Y. Potential role of omental wrapping to prevent infection after treatment for infectious thoracic aortic aneurysms. Eur J Cardiothorac Surg. 2013;43:1177–82.
Kreutz-Rodrigues L, Gibreel W, Moran SL, Mardini S, Bite U, Stulak JM, et al. The utility of the omentum flap for complex intrathoracic problems. Plast Surg (Oakv). 2023;31:17–23.
Horch R, Stark GB. Prosthetic vascular graft infection–defect covering with delayed vertical rectus abdominis muscular flap (VRAM) and rectus femoris flap. Vasa. 1994;2:52–6.
Katsogridakis E, Pokusevski G, Perricone V. The role of sartorius muscle flaps in the management of complex groin wounds. Interact Cardiovasc Thorac Surg. 2019;28:635–7.
Rajput S, Kuruoglu D, Salinas CA, Sen I, Kalra M, Moran SL. Flap management of groin wounds following vascular procedures: a review of 270 flaps for vascular salvage. J Plast Reconstr Aesthet Surg. 2023;78:38–47.
Funding
Open access funding provided by University of the Free State.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study did not require Ethics Committee/Institutional Review Board approval as it did not represent human research.
Informed consent
Not applicable.
Statement of human and animal rights
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented in part at the 10th International Aortic Summit, Chennai, November 18–20, 2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mestres, C., Van Hemelrijck, M., Quintana, E. et al. Significance and current approaches to vascular graft infection. Indian J Thorac Cardiovasc Surg 39 (Suppl 2), 333–340 (2023). https://doi.org/10.1007/s12055-023-01638-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-023-01638-w