Abstract
Extracorporeal membrane oxygenation (ECMO) has strikingly progressed over the last 20 years in the management of adult and pediatric severe respiratory and cardiac dysfunctions refractory to conventional management. In this review, we will discuss the weaning strategies of veno-venous and veno-arterial ECMO including the bridge to recovery and bridge to transplant along with post-ECMO care. We will also discuss the futility and the management of bridge to nowhere from Indian perspectives.
Similar content being viewed by others
Introduction
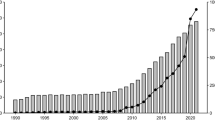
The use of extracorporeal membrane oxygenation (ECMO), both veno-venous and veno-arterial, is an established form of treatment in patients who are suffering from cardio-respiratory failure and are not responding to other conventional measures. The use of ECMO has increased over the past two decades and are still growing [1,2,3,4]. The pandemics such as H1N1 and COVID (coronavirus infection) have increased the significance of ECMO as a lifesaving rescue measure [5]. According to information gathered anonymously from ECMO equipment dealers and personal communication, at present, more than 50 centers are actively providing ECMO service in India and more than 1000 patients were given ECMO support last year. Study regarding implementation of new ECMO centers in SWAAC-ELSO (South Asia, West Asia, and Africa Chapter of Extra-corporeal Life Support Organization) had participation from 4 ECMO centers in India during the early stages of COVID pandemic. The patient survival from new centers, under the supervision of regional experts, was found to be 45% [1].
Although the indications to initiate the ECMO are extensively studied [6], literatures regarding weaning or discontinuation of ECMO are relatively sparse [2, 7, 8]. Ideally, as the primary underlying pathology recovers, ECMO is gradually weaned off. In cases where primary recovery is unlikely, ECMO may be discontinued on the basis of futility or bridge to transplant may be considered. Apart from being an advanced form of life support, ECMO is also a very resource demanding modality of treatment. So, decisions, whether to continue with ECMO or to stop, may be difficult to make at times. In this article, we try to review the factors which are to be taken into consideration while stopping ECMO support. Discontinuation of ECMO is done in following scenarios:
-
Most favorable, that is recovery of the primary organ pathology and weaning
-
Non-recovering organs: futility, bridge to transplant
Primary organ recovery and weaning
Veno-venous ECMO
-
The commonest indication of veno-venous ECMO (VV ECMO) is reversible, severely damaged lungs due to various diseased states, where gaseous exchanges are not maintained with adequate ventilatory support. VV ECMO is to be considered in conditions when there is > 50% chance of mortality due to hypoxia (PaO2:FiO2 < 150 with > 90% FiO2 for more than 6 h, with Murray score 2–3). In conditions where there is > 80% chance of mortality due to hypoxia (PO2:FiO2 < 100 with > 90% FiO2 for more than 6 h), ECMO is indicated [9]. Patients are taken off VVECMO when there is sufficient recovery of native lungs to support the physiological demands of the body with minimum risk of iatrogenic injury [10]. When the parameters are maintained with 40 to 50% of ECMO support with the rest settings of affected primary organ, weaning is considered [11]. In other words, ECMO discontinuation can be considered when 50–80% of total gas exchange is provided by native lungs [12]. Although most of the authors suggest weaning with recovery of lungs and patient maintaining blood gases at moderate ventilatory settings, clear thresholds are not available to direct the weaning. In most of the centers, the ventilatory settings are kept more or less in the following manner while considering ECMO weaning [11, 13]:
-
FiO2 50–40%
-
Positive end-expiratory pressure (PEEP) 8–10 cm H2O
-
Tidal volume 6–8 ml/kg
-
Peak pressure < 30 cm H2O
-
Plateau pressure < 25 cm H2O
Weaning is to be attempted when following parameters are met [11]:
-
Improving chest X-ray
-
Lung compliance improved: compliance > 0.5 ml/kg
-
Arterial blood gas (ABG) on rest ventilation settings with moderate ECMO settings:
-
PaO2 > 60 mm Hg
-
PCO2 < 50 mmHg
-
pH > 7.35
-
Successful 100% oxygen challenge test
-
(This test is done when ECMO support is at 50–60% in ECMO FiO2. Ventilatory FiO2 increased to 100% for 15–20 min and the rise in PO2 in ABG is observed. If it raises > 150 mmHg, then the test is successful.)
Technique for weaning in VV ECMO:
Weaning can be done in either of the following techniques:
-
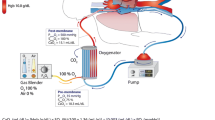
ECMO deoxy challenge test and ECMO CO2 challenge test [14]:
This is a widely used technique of VV weaning. First of all, ventilator FiO2 is increased to 60%. This is done to prevent hypoxia which might occur because of suppressed hypoxic pulmonary vasoconstrictive response of lungs. Hypoxic pulmonary vasoconstriction is suppressed during ECMO due to high mixed venous oxygen saturation. This response is restored slowly during the deoxy challenge test. In case the restoration of hypoxic vasoconstriction does not happen, ventilation-perfusion mismatch will occur and there will be inadequate CO2 removal response.
After the ventilator FiO2 is increased, ECMO FiO2 is reduced by 5% hourly (or may be faster) up to 21%, if patient is maintaining acceptable parameters without discomfort. If deoxy challenge test is successful, second step of the weaning, that is ECMO CO2 challenge test is done. In this, Sweep gas flow is reduced by 30% every 10 min [14]. If patient tolerates sweep reduction, sweep is reduced to zero.
Whether the patient is tolerating weaning is assessed by the following parameters [10]:
-
Mean arterial pressure > 70 mmHg
-
Heart rate between 60 and 110/min (should be maintained similar to pre weaning status)
-
SPO2 > 88% PO2 > 60 mm Hg
-
PCO2 < 50 mmHg
-
pH > 7.35
-
Lactate < 4 mmol/l [10]
-
Urine output ≥ 1 ml/kg/h
-
Lung compliance > 0.5 ml/kg
-
Respiratory rate < 30/min
SPO2 < 88%, respiratory rate > 35/min, P0.1 > 10 cm H2O, hemodynamic worsening, rising lactate, drop in urine output warrants postponing of ECMO weaning. The rate of reduction of ECMO FiO2 and sweep gas flow are to be individualized based upon patient’s response. Higher PCO2 may be acceptable, if patient is comfortable and maintaining other parameters. Some centers prefer to continue zero sweep ECMO run for some duration (24 h) before de-cannulation. There are some centers, where sweep reduction is done after patient remains stable on 21% ECMO FiO2 for 24–48 h [13].
-
b.
Sweep off trial
In this method, after adjusting the ventilator support, sweep is turned off. The venous oxygen saturation of the extracorporeal circuit will indicate when excess oxygen of the circuit has been used up. Usually, the residual oxygen in the ECMO circuit is consumed within half an hour. Sweep is kept off for at least 1–6 h or sometimes more. The ECMO flow is continued unchanged. If patient remains stable, decannulation is planned.
After weaning from ECMO, there are many complications which might happen such as:
-
Post-decannulation systemic inflammatory response syndrome: This complication occurs due to activation of innate immune system by exposure to non-endothelized surfaces of ECMO cannula and circuit. It is difficult to distinguish this condition from sepsis. It is treated with broad spectrum antibiotics unless culture reports are available. [15]
-
Deep vein thrombosis
-
Wound infection
-
Disseminated intravascular coagulation
-
Stroke, renal dysfunction, gastrointestinal bleeding
-
Delirium, post-traumatic stress disorder
Weaning from ECMO does not always mean recovery for the patient, in fact many patients need prolong ventilatory support post ECMO weaning. Post weaning mortality is not uncommon and re-institution of ECMO and/or mechanical ventilation, although infrequent, is associated with poor outcome [7]. A substantial number of patients need additional hospitalization and hospital services even after being discharged [16]. Some of our post-COVID ECMO survivors have been discharged with very limited ability to move around and with home oxygen therapy. Strategies to fasten the weaning from VV ECMO have been studied upon. Uses of levosimendan to increase the power and strength of diaphragm, supplementation of T3 to enhance diaphragm contractile function, and high-dose supplementation of selenium are some of the literatures in this matter [7]. Studies have also shown that proning enhances faster recovery from VV ECMO [7]; this is a strategy which has been frequently tried in severe COVID patients.
Veno-arterial ECMO
Veno-arterial ECMO (VA ECMO) is indicated in refractory cardiogenic shock because of various disease states. The indication includes medical cardiogenic shock resulting from acute myocardial infarction, myocarditis, acute on chronic systolic, diastolic heart failure, drug intoxication, hypothermia [17], and intractable arrhythmias. It is also used in post cardiotomy cardiac failure, bridge to cardiac transplant, and bridge to ventricular assist device (VAD). It has also been used in conditions such as pulmonary embolism; sepsis induced cardiomyopathy. The percentage of patients who are successfully weaned from VA ECMO implantation, done as a rescue measure of refractory cardiogenic shock, varies from 36 to 76% depending upon the primary pathology and definition of successful weaning [18,19,20].
Parameters that are taken into consideration while weaning VA ECMO are similar to that of VV ECMO; however, some special points are to be kept in mind while VA weaning:
-
Timings
It is better not to try any weaning attempt in VA ECMO post cardiogenic shock, within the first 72 h, as this time is needed for organs to recover from the effects of shock. In some conditions, however, VA ECMO weaning may be tried earlier, such as drug toxicity [21]. However, on an average, the duration of the support needed varies from 3.3 ± 2.9 to 8 ± 6.9 days [22].
-
Factors indicating cardiac recovery [23]
-
Increase in blood pressure (systolic blood pressure > 100 mmHg), mean arterial pressure > 60 mmHg [18] with minimal inotropic support and return of pulsatility in arterial waveform. Pulse pressure improvement (> 50 mmHg) [18] has been found to be a predictor of successful weaning [19].
-
Heart rate: < 120/min [10], central venous pressure < 12 mmHg.
-
Mean arterial pressure > 60 mmHg in the absence or with very low vasoactive agent support (inotropic equivalent < 10).
-
Pulsatile arterial waveform should be maintained for > 24 h.
-
If right heart catheterization is done, pulmonary capillary wedge pressure < 24 mmHg, mean pulmonary artery pressure < 25 mmHg, transpulmonary pressure gradient < 10, and pulmonary vascular resistance < 1 wood unit are recommended parameters to achieve prior weaning trial [24].
-
Ideally in pump off condition: cardiac index should be > 2.4L/min/m2, mean arterial pressure > 60 mmHg, pulmonary capillary wedge pressure < 18, central venous pressure (CVP) < 18 should be parameters to consider weaning.
-
Renal issues
Urine output > 0.5 ml/kg/h is criteria for weaning from VA ECMO in patients without renal issues. However, acute kidney injury from shock takes around 4 weeks to recover after improvement of cardiac output; until then, patient can be maintained on renal replacement therapy. So, regarding weaning, it is not necessary to wait for renal function recovery. However, elevated serum creatinine level of > 1.4 mg/dl has been found to be associated with fourfold risk of death [25].
-
Hepatic issues
Shock liver state should get corrected before weaning is considered [26].
-
Tissue perfusion parameters
ABG lactate < 3 mmol/L and mixed venous saturation of < 65% are criteria for weaning from VA ECMO [10]. According to studies, the only biomarker which is suitable and practical to use as a tool for weaning suitability and overall prognosis is lactate and lactate clearance [27, 28]. In one study, Loforte et al., 72 h post ECMO implantation lactate of > 3 mmol/L was a predictor of 50% probability of 30-day mortality [26]. In another study, Li et al. showed that early lactate behaviors, particularly lactate clearance after ECMO support, are highly associated with in hospital mortality. They also showed that early lactate behavior has predictive value in successful weaning from ECMO [27].
-
Echocardiographic assessment
Studies have shown that echocardiography is an important tool to determine both the recovery of left ventricle (LV) function and the readiness of patients for weaning from ECMO support [29,30,31].
High values of parameters assessing left ventricular systolic function: aortic velocity time integral, left ventricular ejection fraction (LVEF), and lateral mitral annulus peak systolic velocity (LVEF ≥ 20–25%, an aortic velocity–time integral of ≥ 12 cm and a lateral mitral annulus peak systolic velocity of ≥ 6 cm/s) are predictors of successful weaning.
Precise right ventricular (RV) assessment is not frequently done except where RV dilatation is present. Recent study has shown that smaller RV dimension, better right ventricular ejection fraction, higher RV area change, and higher magnitudes of RV strain are associated with successful ECMO weaning. In one study [32], right ventricle/pulmonary artery coupling has been measured by tissue Doppler and tricuspid lateral annular peak systolic velocity (S′) divided RV systolic pressure (RVSP), and it was concluded that S′/RVSP cutoff > 0.33, at full ECMO support, was better to predict successful weaning in comparison to LV parameters.
-
Patients needing veno-arterial ECMO support are usually volume overloaded with high inotropic requirements. Before weaning is planned, volume overload should be taken care of by diuresis or, if needed, hemodialysis. Inotropic requirement should get reduced to moderate level [31].
Method of weaning
Weaning trials are done to assess the behavior of ventricles during increases in preload and to determine whether the ECMO can be safely removed [33]. When the ECMO flow is decreased, the left ventricular preload is increased while the afterload is decreased. With increase of the preload and decrease of the afterload, a load-dependent contractile reserve of the LV (Frank-Starling reserve) can be assessed [34]. Presence of this contractility is associated with successful weaning [34]. A reduction in ECMO flow also increases the right ventricular preload and enables its function to be assessed. Two echocardiographic strategies for carrying out the weaning have been described in the literature [34].
Transthoracic echocardiography study [33].
It was conducted when patient was hemodynamically stable (mean arterial pressure > 60 mmHg, pulsatile arterial wave form maintained for 24 h), without or with very low doses of vasoactive agents and pulmonary oxygenation of the blood was not compromised.
ECMO flow was decreased to 66% of the initial flow rate for 10–15 min followed by decreasing to 33% for 10–15 min and then to 1–1.5L/min for another 10–15 min.
The trial was stopped and full ECMO support was returned if there was drop in arterial blood pressure. The ECMO removal was considered if there was no end-stage cardiac disease or partially/fully recovered cardiac dysfunction with left ventricular ejection fraction > 25%, and velocity time integral (VTI) > 10 with minimum ECMO support.
Transesophageal echocardiography study [35].
Four-stage weaning trial:
-
Stage 1—assessment of baseline RV and LV volume and function on full ECMO support
-
Stage 2—gradual reduction of ECMO flow to increments of 0.5 L/min to half of the original flow. Trial stopped and returned to full ECMO support if there is hypotension or LV or RV distension
-
Stage 3—volume challenge with 5% albumin@ 10 ml/kg and reduction of ECMO flow to 1.2 to 1.5 L/min
-
Stage 4—LV and RV function was assessed during the infusion of inodilators.
-
for 4–6 h. These drugs are used to assess RV function in patients with LV dysfunction, who are being evaluated for left ventricular assist device (LVAD) placement
In our institution:
Wean the pump flow by 10 ml/kg/h, until idle flow is reached, which is 10 ml/kg/min. Sweep gas flow is adjusted according to the blood flow.
Once the patient is on minimum support, ventilator settings are adjusted to a moderate level.
Keep the patient on idle flow for 2 h. Patient’s response to each change in flow is observed for 15 min to up to an hour or even more. Activated clotting time (ACT) should be maintained ≥ 200 s as pump flow is weaned.
Trial off:
In 2 h idle flow, if patient is maintaining:
-
Mean arterial pressure > 70 mmHg, pulse pressure > 30 mmHg
-
Mixed venous saturation > 70%, lactate < 2 mmol/L, urine output 1–2 ml/kg/h
-
Echo: VTI > 10, lateral mitral annulus peak systolic velocity (TDSa) > 6 cm/s
Trial off is conducted. While conducting the trial off:
-
Keep moderate ventilator settings and continue low-dose inotropes.
-
Clamp the arterial cannula, release the clamp from the bridge, and then clamp the venous cannula.
-
Disconnect gas from oxygenator, stop ultrafiltration.
-
ABG is done 10 min after starting the trial off and repeated after 1 h and then 2 h of trial off.
-
Do ACT of the patient and circuit separately every 30 min as both are not connected now.
-
Flush cannula every 10 min for 15 s: release the vein first, clamp the bridge, then release the artery. Wait for 15 s then clamp in previous order.
-
Time to undertake trial off is 2–3 h.
-
If trial off is successful, decannulation will be done.
-
Pump-controlled retrograde trial off:
This is a method of trial off in which arterio-venous bridge is not needed and trial off can be continued for longer duration without circuit clot formation or significant hemodynamic compromise. To do this, sweep gas is disconnected and trial off is commenced. At the start of trial off, flow probe is reversed and revolutions per minute is reduced. As the pressure generated by the pump falls below the systemic arterial pressure, retrograde flow is established. The pump itself acts as a control to prevent excessive retrograde flow and systemic steal. ACT is maintained between 200 and 220 s.
Aids for successful weaning:
Inodilators and intra-aortic balloon pump have been shown to facilitate weaning from VA ECMO; however, evidences are sparse [36, 37].
De-cannulation
Once weaning is successful, ECMO de-cannulation is to be considered. The process of decannulation may vary from institution to institution. One has to be absolutely sure before de-cannulation as re-cannulation of the major vessels (if needed) may be difficult. Process of de-cannulation differs according to the type of ECMO, site of cannulation, cannulation techniques, and size of cannula. Percutaneously placed venous cannula can be removed percutaneously while large diameter arterial cannula or surgically placed cannulas are removed surgically. While decannulation is being done, a team should be ready for resuscitation without delay in case of a problem.
In our place, arterial cannula is generally taken out by surgical de-cannulation and or patch repair, but percutaneously placed small femoral arterial cannula may be removed directly by mattress suture and direct compression. Carotid artery de-cannulation can be done by either repair, reconstruction, or direct tie-off. Risk of embolism and dissection is there when reconstruction is tried.
In an awake and cooperative patient, venous cannula can be removed without sedation. The area around the venous cannula should be infiltrated with local anesthetic and a horizontal mattress suture placed in the cannulation wound. The risk of air embolism has to be kept in mind and a positive pressure needs to be applied when the cannula is withdrawn.
A conscious patient is then asked to perform a valsalva maneuver to prevent air embolism, the tubing is clamped, the cannula is smartly withdrawn by an assistant, and the suture is tied. Direct and continuous pressure for 30 min is required for percutaneously removed cannula. If the patient is sedated and fully ventilated, positive-pressure ventilation will prevent an air embolism.
Post decannulation patient must be kept flat for 6 h and not allowed to bend knee of the affected side for 6 h in case of femoral cannulation. Monitor sites every 30 min for 4 h post decannulation for any signs of hematoma or any bleeding. If bleeding is present, direct pressure is to be applied.
ECMO as bridge to transplant
In patients in whom primary organ recovery does not happen, and who are suitable to undergo transplant, ECMO has been used as a bridge. ECMO has been used to temporarily support the patients who are candidates for lung transplant, heart transplant, or both heart and lung transplant.
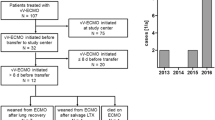
Lung transplant
Patients with end-stage lung disease, who present with acute exacerbations, require aggressive noninvasive or invasive ventilation strategies. When these patients do not improve or worsen on ventilation, the ECMO is considered a bridge to transplant. The indication for ECMO is determined by the patient’s candidacy for lung transplantation [38]. If the patient is already on the waitlist and irreversible end-organ damage or other conditions that would preclude him or her from remaining on the list have not developed, then ECMO is certainly indicated [39]. For patients who are still not cleared for transplant or it is still not cleared whether their disease process is irreversible, ECMO can be used as bridge to decision. ECMO can be used for pre-transplant, intraoperative, and post-transplant support. Both VV and VA ECMO are used to support lung transplant patients. While VV ECMO is preferred for bridge to transplant, bridging to recovery post-transplant severe graft dysfunction, VA ECMO is used to bridge patients with prevalent cardiocirculatory failure [40].
Management of pretransplant ECMO is done according to standard ECMO practices. Lungs are periodically examined for recovery. It is preferable to extubate the patients or, if not feasible, go for early tracheostomy; the idea is to make the patient ready for conditioning programs as physical deconditioning is common in ECMO [35]. Ambulatory ECMO has been found to be very helpful in this regard. It also helps to assess patient’s recovery post-transplant [41]. Studies have shown improvement in outcomes of ECMO bridging for transplant in last decade [38]. Careful patient selection, awake ECMO, center transplant volume, and experience have been suggested as the reason behind this improvement [41].
Apart from patients who are already on ECMO pre-transplant, presence of a secondary pulmonary arterial hypertension, dilated hypertrophied RV, and small thoracic cavity are conditions which are high risk for intraoperative ECMO requirement [41]. Hypercapnia, arterial saturation < 90%, cardiac index < 2L/min/m2, and supra–systemic pulmonary artery pressure are conditions where intraoperatively ECMO is used as rescue. At the end of transplant, before closing the thoracotomies, possibility of ECMO explantation is considered, and if parameters are satisfactory, ECMO is explanted. If parameters are not suitable for ECMO explantation, or in certain condition such as idiopathic pulmonary hypertension, ECMO (VA) is continued post operatively. Studies have shown that factors such as increase donor age, donor PaO2, and increased operating time are risk factors for intra-operative ECMO weaning failure [42].
Post-transplant graft dysfunction is another condition where ECMO has its role when conservative therapy fails. Graft function and survival are worse in patients who need secondary ECMO, but early ECMO support has shown relatively better outcome [43]. In patients with idiopathic pulmonary hypertension, and post-transplant, there occurs pulmonary edema due to LV diastolic failure. In these patients, VA ECMO is continued until pulmonary arterial and left atrial pressures normalize. Following that ECMO is weaned [41].
Heart transplant
Refractory cardiogenic shock can occur following myocardial infarction, open heart surgery, cardiomyopathy, and decompensated heart failure. ECMO in these situations can act as bridge to decision, bridge to recovery, bridge to implant of a longer lasting mechanical circulatory support, or bridge to heart transplant. Although case reports and retrospective studies have shown higher post-transplant mortality rate when VA ECMO is used as direct bridge to transplant measure, it still remains useful rescue therapy for INTERMACS class 1 and 2 patients who would otherwise fail to survive [44,45,46,47]. VA ECMO is also indicated in patients with advanced stages of heart failure in whom LVAD implantation is not feasible (e.g., anatomical contraindication), to buy time in patients with uncertain decision, and to transport patients to a specialist center for surgical insertion of mechanical support.
Apart from acting as a bridge to transplant or bridge to bridge (LVAD implantation) [48], VA ECMO has crucial role in managing post-transplant primary graft dysfunction by:
-
reducing venous return which results in reduced LV end diastolic volume and pressure, leading to reduced LV transmural stress and myocardial recovery;
-
minimizing cardiac work during recovery and reducing inotropic requirement; and
-
maintaining organ perfusion.
Following transplant, VA ECMO is discontinued when there is evidence of improved graft function (LVEF > 25%, aortic VTI > 12 cm, stable hemodynamics, continuous pulsatile waveform, minimum inotropic requirements). Weaning procedure is the same as discussed before.
Discontinuation on the basis of futility
Some case scenarios
Case 1
A one-year-old baby, suffering from septic myocarditis with pneumonia, could not be weaned off ECMO until 21 days. The baby was diagnosed to be having cystic fibrosis. The family did not want to continue further on ECMO, so oxygenator change was withheld to render futility.
Case 2
A 64-year-old gentleman after 140 days of COVID ECMO support had gross fibrotic changes in lungs in computed tomography (CT) scan. The family did not give consent for lung transplant and hence ECMO was discontinued considering long-term futility.
Case 3
A 40-year-old patient suffering from COVID acute respiratory distress syndrome (ARDS) was supported with VV ECMO. CT scan, however, showed massive hemorrhage with bilateral infarcts. The family wanted to continue ECMO until cardiovascular death.
Both VA ECMO and VV ECMO are very advanced forms of cardio-respiratory support but these are not curative measures. Situations do arise where in spite of proper ECMO management and organ support, primary pathology does not recover. In these patients, if organ transplant is not feasible, ECMO discontinuation is to be considered on the basis of futility [49]. Futile treatment is against the three key principles of ethics: beneficence, non-maleficence, and distributive justice. In most of the time, autonomy is no longer applicable as most of the patients are not capable of deciding. This is often a very difficult decision to take, both for the treating team and for patient relatives.
Continuing ECMO support is considered to be futile when there is:
-
extensive central nervous system damage such as in hypoxic-ischemic brain injury, massive intracranial hemorrhage, and massive cerebral infarct—conditions which make neurological recovery unlikely;
-
irreversible lung or heart pathology with non-feasible surgical intervention, and other mechanical circulatory support implantation or transplantation. Thorough clinical documentation of irreversibility is important (multiple weaning failure, worsening radiological findings of lungs, non-improving or worsening echocardiography finding etc.); and
-
severe sepsis with multiorgan dysfunction: although this should not be the lone factor to consider futility.
Decision of futility should always be taken as a cumulative decision involving all the team members and all the clinical data should be considered [50]. Patient relatives should be included in the discussions, and their doubts should be cleared to prevent any future miscommunications. Final decision is to be taken by the physician-in-charge acting in the best of patient’s interest [50]. Patient’s relatives should be provided with frequent updates about patient’s condition and prognosis; there should not be any disparity of information among the members of the treating team. Once the futility is explained and decided, the next plan of action may be:
-
no resuscitation if cardio respiratory arrest occurs or
-
no new interventions (like dialysis, continuous renal replacement therapy, increasing vasoactive supports) are to be done, but present treatment is continued or
-
all treatment and life supports are withdrawn, maintaining deep sedation to keep the patient comfortable.
After the decision of futility is made, proper palliative care is a must and patient should have a dignified and comfortable death, and should never be neglected or left out.
The decision of whether to discontinue ECMO on the basis of futility is always difficult, and it has many gray areas with multiple legal and ethical issues. However, if the outcome of the patient is not going to change, continuation of ECMO seems to prolong patient’s sufferings and the natural course of death. It also causes undue wastage of resources which might be very significant in limited resource situations like COVID pandemic in our country. That being said, it should always be kept in mind that prolong duration of ECMO should not be considered futile as there are multiple instances from various centers where recovery has happened after long term extra-corporeal life support (ECLS). In our center in the COVID pandemic time, we have seen people recovering after 4–5 months of ECMO support. Recovery after 600 days on ECMO has also been reported [51]. Financial constraints have been a major problem in continuation of long-term ECMO support in our country. The longer ECMO run does not always mean the higher use of consumables, but concurrent sepsis and use of other organ support increases the cost exponentially. Early referral can partly solve the problems. However, discontinuation of ECMO should not be done, only upon financial issues. The high cost of ECMO can be brought down by manufacturing cannula, circuits, and oxygenators locally by “Make in India” initiatives [52]. Effective utilization of the funds with prior intimation to healthcare insurance schemes has made ECMO affordable to majority of population by increasing awareness. Private healthcare schemes provided by the corporate sector, various crowd funding, corporate social responsibilities, and, to some extent, personal funding made ECMO affordable to various income group families during COVID-19 times. It has been noticed that government-funded/autonomous apical institutions adopted this technology in a cost-effective way as they have the resources and trained manpower available at lower cost [52].
The indications for ECMO have been varying in India, starting from myocarditis due to scorpion stings, snake bites, supporting patients of toxic myocarditis from Celphos poisoning. ARDS secondary to malaria, tuberculosis, typhus, dengue, and other tropical diseases offer exciting opportunities for application of this life-saving modality. ECMO practice in India has numerous challenges including knowledge and awareness of the efficacy and indications, timing of referral from the referring centers, choosing the right equipment, travel delays during transport, cost factors, and availability of financial resources [52]. Though COVID-19 has created a need and awareness for ECMO nationwide, it has warranted the judicious use also, especially for prolonged ECMO. Many a times the request for referral comes from the relatives of keen due to increasing mass awareness about ECMO.
Hospital-acquired infection is one of the major problems contributing to reduction in the survival rate in our country as well as resulting in long ECMO run, intensive care unit stay, and the comorbid complications [52]. Universal aseptic precautions, staff education, minimizing usage of broad-spectrum antibiotics, and early de-escalation of antibiotics are extremely important steps in improving overall outcome. Even after coming off ECMO and getting discharged, the physical and psychological after-effects can give rise to difficulties in healthy lifestyle. We have seen many of our survivors transiently lost their jobs or could not perform strenuous activities in post-recovery period, especially after long COVID. They need to be followed up regarding requirements of anticoagulation, improvement of heart and lung function, and psychological counseling until they resume professional activities.
Case scenario
A 29-year-old female was kept on ECMO support for 81 days. The family was not able to pay but the patient was improving. Crowd funding was organized by the treating doctors and the hospital. She was eventually, successfully weaned off ECMO and was discharged.
Conclusion
Plan for weaning should be started from the very first day of starting ECMO as an exit strategy either by primary organ recovery or by organ transplant. Weaning from VA ECMO is to be planned when patients have mean arterial pressure (MAP) > 60 mmHg, left ventricular ejection fraction (LVEF) ≥ 25%, left ventricular outflow tract velocity time integral (LVOT VTI) > 0.12 m/s, or tissue Doppler lateral mitral annulus peak systolic velocity ≥ 6 cm/s. Once weaning criteria are met, trial off is to be conducted by creating a bridge and clamping the arterial and venous cannulas [53]. Weaning from VV ECMO is to be planned when patients have stable hemodynamics and acceptable ABG parameters (pH > 7.35, PaO2 > 70 mmHg, PaCO2 < 50 mmHg) at ventilator settings of FiO2 < 60%, plateau pressure ≤ 28 mmHg, respiratory rate ≤ 28/min, tidal volume ≤ 6 ml/kg, and PEEP ≤ 10 cm H2O [54].
Many longer ECMO runs can be affected by clinical conditions or by surrounding socio-economic situations. Patients getting weaned off ECMO need thorough post-ECMO care and rehabilitation to ensure discharge and ultimate recovery.
References
Rabie AA, Azzam MH, Al-Fares AA, et al. Implementation of new ECMO centers during the COVID-19 pandemic: experience and results from the Middle East and India. Intensive Care Med. 2021;47:887–95. https://doi.org/10.1007/s00134-021-06451-w.
Al-Fares AA, Ferguson ND, Ma J, et al. Achieving safe liberation during weaning from VV-ECMO in patients with severe ARDS: the role of tidal volume and inspiratory effort. Chest. 2021;160:1704–13. https://doi.org/10.1016/j.chest.2021.05.068.
Enciso JS, Hong KN. ECMO weaning strategies to optimize outcomes. In: Firstenberg MS, editor. Advances in extracorporeal membrane oxygenation - volume 3 [Internet]. London: IntechOpen; 2019 [cited 2022 Apr 09]. Available from: https://www.intechopen.com/chapters/66576https://doi.org/10.5772/intechopen.85614.
Lüsebrink E, Stremmel C, Stark K, et al. Update on weaning from veno-arterial extracorporeal membrane oxygenation. J Clin Med. 2020;9:992. https://doi.org/10.3390/jcm9040992.
Brodie D, Abrams D, MacLaren G, et al. ECMO during respiratory pandemics: past, present, and future. Am J Respir Crit Care Med. 2022 Feb 25. https://doi.org/10.1164/rccm.202111-2661CP.
Malfertheiner MV, Broman LM, Belliato M, et al. Management strategies in venovenous extracorporeal membrane oxygenation: a retrospective comparison from five European centres. Crit Care Resusc. 2017;19:76–81.
Broman LM, Malfertheiner MV, Montisci A, Pappalardo F. Weaning from veno-venous extracorporeal membrane oxygenation: how I do it. J Thorac Dis. 2018;10:S692–7.
Extracorporeal Life Support Organization (ELSO) Guidelines for Adult Respiratory Failure August, 2017
Shekar K, Buscher H, Brodie D. Protocol-driven daily optimisation of venovenous extracorporeal membrane oxygenation blood flows: an alternate paradigm? J Thorac Dis. 2020;12:6854–60. https://doi.org/10.21037/jtd-20-1515.
Goyal V, Oza P. Weaning and trial off. In: Goyal V, Oza P, editor. ECMO theoretical manual volume II;1st ed. Mumbai:2012; p. 227 to 229.
Extra corporeal life support Organization. ELSO guidelines for cardiopulmonary extracorporeal life support. Version 1.4. August 2017. Ann Arbor, MI. https://www.elso.org.
Grant AA, Hart VJ, Lineen EB, et al. A weaning protocol for veno-venous extracorporeal membrane oxygenation with a review of literature. Artif Organs. 2018;42:605–10.
Yeo HJ, Kim YS, Kim D, ELSO Registry Committee, Cho WH. Risk factors for complete recovery of adults after weaning from veno-venous extracorporeal membrane oxygenation for severe acute respiratory failure: an analysis from adult patients in the Extracorporeal Life Support Organization registry. J Intensive Care. 2020;8:64. https://doi.org/10.1186/s40560-020-00480-1.
Vasques F, Romitti F, Gattinoni L, Camporota L. How I wean patients from veno-venous extra-corporeal membrane oxygenation. Crit Care. 2019;23:316.
Thangappan K, Cavarocchi NC, Baram M, Thoma B, Hirose H. Systemic inflammatory response syndrome (SIRS) after extracorporeal membrane oxygenation (ECMO): incidence, risks, survivals. Heart Lung. 2016;45:449–53.
Aissaoui N, Luyt C-E, Leprince P, et al. predictors of successful extracorporeal membrane oxygenation (ECMO) weaning after assistance for refractory cardiogenic shock. Intensive Care Med. 2011;37:1738–45.
Chakraborty A, Chatterjee D, Sarkar K. Weaning and liberation from V-A ECMO. In: Maybauer MO, editor. Extracorporeal Membrane Oxygenation, An Interdisciplinary Problem-Based Learning Approach. 1st ed. New York: Oxford; 2022. p. 551–2.
Pappalardo F, Pieri M, Arnaez Corada B, et al. Timing and strategy for weaning from venoarterial ECMO are complex issues. J CardiothoracVascAnesth. 2015;29:906–11.
Aissaoui N, El-Banayosy A, Combes A. How to wean a patient from veno-arterial extracorporeal membrane oxygenation. Intensive Care Med. 2015;41:902–5.
Baud FJ, Megarbane B, Deye N, Leprince P. Clinical review: aggressive management and extracorporeal support for drug induced cardiotoxicity. Crit Care. 2007;11:207.
Durinka JB, Bojar LJ, Hirose H, et al. End-organ recovery is key to success for extracorporeal membrane oxygenation as a bridge to implantable left ventricular assist device. ASAIO J. 2014;60:189-192.
Abrams D, Garan AR, AbdelbaryA, et al. Position paper for the organization of ECMO programs for cardiac failiure in adults. Intensive Care Med. 2018;44:717–29.
Huang K-C, Lin L-Y, Chen Y-S, Lai C-H, Hwang J-J, Lin L-C. Threedimensional echocardiography-derived right ventricular ejection fraction correlates with success of decannulation and prognosis in patients stabilized by venoarterial extracorporeal life support. J Am Soc Echocardiogr. 2018;31:169–79.
Rousse N, Juthier F, Pincon C, et al. ECMO as a bridge to decision: recovery, VAD, or heart transplantation? Int J Cardiol. 2015;187:620–7.
Extracorporeal Life Support Organization. ELSO guidelines for cardiopulmonary extracorporeal life support. Version 1.3. Ann Arbor, MI. November 2013. http://www.elsonet.org.
Loforte A, Marinelli G, Musumeci F, et al. Extracorporeal membrane oxygenation support in refractory cardiogenic shock: treatment strategies and analysis of risk factors. Artif Organs. 2014;38:E129–41.
Li C-L, Wang H, Jia M, Ma N, Meng X, Nou X-T. The early dynamic behaviour of lactate is linked to mortality in post cardiotomy patients with extracorporeal membrane oxygenation support: a retrospective observational study. J Thorac Cardiovasc Surg. 2015;149:1445–50.
Platts DG, Sedgwick JF, Burstow DJ, Mullany DV, Fraser JF. The role of echocardiography in the management of patients supported by extracorporeal membrane oxygenation. J Am Soc Echocardiogr. 2012;25:131–41.
Aissaoui N, Guerot E, Combes A, et al. Two-dimensional strain rate and Doppler tissue myocardial velocities: analysis by echocardiography of hemodynamic and functional changes of the failed left ventricle during different degrees of extracorporeal life support. J Am Soc Echocardiogr. 2012;25:632–40.
Aissaoui N, Brehm C, El-Banayosy A, Alain Combes A. Weaning strategy from veno-arterial extracorporeal membrane oxygenation (ECMO). In: Firstenberg, M. S., editor. Extracorporeal Membrane Oxygenation - Advances in Therapy [Internet]. London: IntechOpen; 2016 [cited 2022 Apr 04]. Available from: https://www.intechopen.com/chapters/51568https://doi.org/10.5772/64013.
Kim D, Park Y, Choi KH, et al. Prognostic implication of RV coupling to pulmonary circulation for successful weaning from extracorporeal membrane oxygenation. JACC Cardiovasc Imaging. 2021;14:1523–31.
Ortuno S, Delmas C, Diehl JL, et al. Weaning from veno-arterial extra-corporeal membrane oxygenation: which strategy to use? Ann Cardiothorac Surg. 2019;8:E1–8. https://doi.org/10.21037/acs.2018.08.05.
Aissaoui N, Guerot E, Combes A, et al. Two-dimensional strain rate and Doppler tissue myocardial velocities: analysis by echocardiography of hemodynamic and functional changes of the failed left ventricle during different degrees of extracorporeal life support. J Am Soc Echocardiogr. 2012;25:632–40.
Cavarocchi NC, Pitcher HT, Yang Q, et al. Weaning of extracorporeal membrane oxygenation using continuous hemodynamic transesophageal echocardiography. J Thorac Cardiovasc Surg. 2013;146:1474–9.
Affronti A, di Bella I, Carino D, Ragni T. Levosimendan may improve weaning outcomes in venoarterial ECMO patients. ASAIO J. 2013;59:554–7.
Petroni T, Harrois A, Armour J, et al. Intra-aortic balloon pump effects on macrocirculation and microcirculation in cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation. Crit Care Med. 2014;42:2075–82.
Loor G, Simpson L, Parulekar A. Bridging to lung transplantation with extracorporeal circulatory support: when or when not? J Thorac Dis. 2017;9:3352–61. https://doi.org/10.21037/jtd.2017.08.117.
Rajagopal K, Hoeper MM. State of the art: bridging to lung transplantation using artificial organ support technologies. J Heart Lung Transplant. 2016;35:1385–98.
Mangi AA, Mason DP, Yun JJ, Murthy SC, Pettersson GB. Bridge to lung transplantation using short-term ambulatory extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2010;140:713–5.
Narm KS, Lee S, Suh JW, et al. Risk factor analysis for intraoperative extracorporeal membrane oxygenation weaning failure after lung transplantation. Ann Thorac Surg. 2018;105:242–8.
Ius F, Tudorache I, Warnecke G. Extracorporeal support, during and after lung transplantation: the history of an idea. J Thorac Dis. 2018;10:5131–48. https://doi.org/10.21037/jtd.2018.07.43.
Hartwig MG, Walczak R, Lin SS, Davis RD. Improved survival but marginal allograft function in patients treated with extracorporeal membrane oxygenation after lung transplantation. Ann Thorac Surg. 2012;93:366–71.
Urban M, Siddique A, Merritt-Genore H, Um J. What are the results of veno arterial extracorporeal membrane oxygenation bridging to heart transplantation? Interact Cardiovasc Thorac Surg. 2019;29:632–4. https://doi.org/10.1093/icvts/ivz096.
Zalawadiya S, Fudim M, Bhat G, Cotts W, Lindenfeld J. Extracorporeal membrane oxygenation support and post-heart transplant outcomes among United States adults. J Heart Lung Transplant. 2017;36:77–81. https://doi.org/10.1016/j.healun.2016.10.008.
Fukuhara S, Takeda K, Kurlansky PA, Naka Y, Takayama H. Extracorporeal membrane oxygenation as a direct bridge to heart transplantation in adults. J Thorac Cardiovasc Surg. 2018;155:1607-1618.e6. https://doi.org/10.1016/j.jtcvs.2017.10.152.
Jahanyar J, Liao JM, Zhang N, et al. Heart transplantation with ECMO bridging: survival differences in the era of the new heart allocation policy. J Heart Lung Transplant. 2019;38:S389–90. https://doi.org/10.1016/j.healun.2019.01.992.
Guha A, Hannawi B, Cruz-Solbes AS, et al. Implication of ventricular assist devices in extracorporeal membranous oxygenation patients listed for heart transplantation. J Clin Med. 2019;8:572. https://doi.org/10.3390/jcm8050572.
Mulaikal TA, Nakagawa S, Prager KM. Extracorporeal membrane oxygenation bridge to no recovery. Circulation. 2019;139:428–30.
MacLaren G. When to initiate ECMO with low likelihood of success. Crit Care. 2018;22:217.
Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. 2014;145:876–82.
Bein T, Brodie D. Understanding ethical decisions for patients on extracorporeal life support. Intensive Care Med. 2017;43:1510–1.
Pooboni S, Goyal V, Oza P, Kapoor PM. ECMO challenges and its future: indian scenario. J Card Crit Care TSS. 2017;01:89–94. https://doi.org/10.1055/s-0038-1626672.
Lorusso R, Shekar K, MacLaren G, et al. ELSO interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. ASAIO J. 2021;67:827–44. https://doi.org/10.1097/MAT.0000000000001510.
Tonna JE, Abrams D, Brodie D, et al. Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the Extracorporeal Life Support Organization (ELSO). ASAIO J. 2021;67:601–10. https://doi.org/10.1097/MAT.0000000000001432.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics committee approval
Not required being a review article.
Informed consent
Not required being a review article.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chakraborty, A., Majumdar, H.S., Das, W. et al. Discontinuation of ECMO—a review with a note on Indian scenario. Indian J Thorac Cardiovasc Surg 39 (Suppl 1), 134–142 (2023). https://doi.org/10.1007/s12055-022-01453-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-022-01453-9