Abstract
Background
The Trifecta valve has been reported to have excellent hemodynamics. Controversy exists on occurrence of patient-prosthesis mismatch (PPM) and data on mid-term outcome is sparse. Health-related quality of life (HRQoL) assessment for the Trifecta valve has not been reported before. The aim of this study was to report the mid-term clinical and HRQoL outcomes in patients undergoing Trifecta valve implantation at our institution.
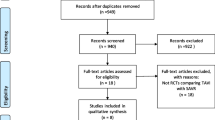
Methods
In this prospective, observational study, patients undergoing an aortic valve replacement (AVR) using the Trifecta valve were included. Data collection was retrospective from prospectively collected institutional database. Clinical and echocardiographic data were collected prospectively during follow-up. Quality of life was assessed using the Short Form-36 (SF-36) questionnaire.
Results
Forty-seven patients were included in the study of which 9 (19%) were women. Isolated AVR was carried out in 33 (70%) patients. In-hospital mortality and 30-day mortality were 1 (2.1%) and 2 (4.2%), respectively. With a mean indexed effective orifice area (iEOA) 0.96 ± 0.1, none of the patients had severe PPM. Moderate PPM was seen in 19%. The mean follow-up was 3 ± 1.7 years. The 5-year survival estimate was 83.2% in the overall cohort, 81.4% in the isolated and 87.5% in the concomitant procedure group. Freedom from re-operation and structural valve degeneration at 5 years was 95.7% and 97.8%. The mean physical health composite was 69.24 ± 2 and the mean mental health composite was 69.7 ± 25, indicating excellent mental and physical well-being among patients.
Conclusion
The Trifecta valve provides satisfactory hemodynamics, survival and freedom from re-operation and excellent HRQoL at mid-term follow-up.





Similar content being viewed by others
References
Dell’Aquila AM, Schlarb D, Schneider SRB, et al. Clinical and echocardiographic outcomes after implantation of the Trifecta aortic bioprosthesis: an initial single-centre experience. Interact Cardiovasc Thorac Surg. 2013;16:112–5.
Kilic A. Structural valve deterioration with the Trifecta: is it the valve or is it implant technique? Ann Thorac Surg. 2020;110:888–9.
Biancari F, Valtola A, Juvonen T, et al. Trifecta versus Perimount Magna Ease aortic valve prostheses. Ann Thorac Surg. 2020;110:879–88.
Kaneyuki D, Nakajima H, Asakura T, et al. Early first-generation Trifecta valve failure: a case series and a review of the literature. Ann Thorac Surg. 2020;109:86–92.
Piñón M, Durán D, Pazos P, Pradas G. Leaflet tear in a Trifecta aortic bioprosthesis 34 months after implantation. Interact Cardiovasc Thorac Surg. 2015;20:281–2.
Hamamoto M, Kobayashi T, Ozawa M, Yoshimura K. Pure cusp tear of Trifecta bioprosthesis 2 years after aortic valve replacement. Ann Thorac Cardiovasc Surg. 2017;23:157–60.
Phan K, Ha H, Phan S, Misfeld M, Di Eusanio M, Yan TD. Early hemodynamic performance of the third generation St Jude Trifecta aortic prosthesis: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2015;149:1567–1575.e1–2.
Bavaria JE, Desai ND, Cheung A, et al. The St Jude Medical Trifecta aortic pericardial valve: results from a global, multicenter, prospective clinical study. J Thorac Cardiovasc Surg. 2014;147:590–7.
Mariscalco G, Mariani S, Bichi S, et al. St Jude Medical Trifecta aortic valve: results from a prospective regional multicentre registry. J Cardiothorac Surg. 2015;10:169.
Yadlapati A, Diep J, Barnes MJ, Grogan T, Bethencourt DM, Vorobiof G. Comprehensive hemodynamic comparison and frequency of patient-prosthesis mismatch between the St. Jude Medical Trifecta and Epic Bioprosthetic aortic valves. J Am Soc Echocardiogr. 2014;27:581–9.
Mannam G, Mishra Y, Modi R, et al. Early hemodynamic performance of the TrifectaTM surgical bioprosthesis aortic valve in Indian patient population: 12 month outcomes of the EVEREST post-market study. J Cardiothorac Surg. 2018;13:96.
Kilic A, Sultan I, Navid F, et al. Trifecta aortic bioprosthesis: midterm results in 1,953 patients from a single center. Ann Thorac Surg. 2019;107:1356–62.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Jansen Klomp WW, Nierich AP, Peelen LM, et al. Survival and quality of life after surgical aortic valve replacement in octogenarians. J Cardiothorac Surg. 2016;11:38.
Al-Ruzzeh S, Mazrani W, Wray J, et al. The clinical outcome and quality of life following minimally invasive direct coronary artery bypass surgery. J Card Surg. 2004;19:12–6.
Lindsay GM, Hanlon P, Smith LN, Wheatley DJ. Assessment of changes in general health status using the short-form 36 questionnaire 1 year following coronary artery bypass grafting. Eur J Cardiothorac Surg. 2000;18:557–64.
Laucis NC, Hays RD, Bhattacharyya T. Scoring the SF-36 in orthopaedics: a brief guide. J Bone Joint Surg Am. 2015;97:1628–34.
Blais C, Dumesnil JG, Baillot R, Simard S, Doyle D, Pibarot P. Impact of valve prosthesis-patient mismatch on short-term mortality after aortic valve replacement. Circulation. 2003;108:983–8.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e35–71.
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Hernandez-Vaquero D, Diaz R, Pascual I, et al. The prevalence of patient-prosthesis mismatch can be reduced using the Trifecta aortic prosthesis. Ann Thorac Surg. 2018;105:144–51.
Manabe S, Koinoshita R, Hirayama D, Yuge N, Hirooka K. Hemodynamic performance and incidence of patient–prosthesis mismatch of small-sized Trifecta pericardial aortic valves. Gen Thorac Cardiovasc Surg. 2020;68:938–42.
Mohty D, Malouf JF, Girard SE, et al. Impact of prosthesis-patient mismatch on long-term survival in patients with small St Jude Medical mechanical prostheses in the aortic position. Circulation. 2006;113:420–6.
Del Rizzo DF, Abdoh A, Cartier P, Doty D, Westaby S. Factors affecting left ventricular mass regression after aortic valve replacement with stentless valves. Semin Thorac Cardiovasc Surg. 1999;11:114–20.
Bakhtiary F, Schiemann M, Dzemali O, et al. Impact of patient-prosthesis mismatch and aortic valve design on coronary flow reserve after aortic valve replacement. J Am Coll Cardiol. 2007;49:790–6.
Moon MR, Pasque MK, Munfakh NA, et al. Prosthesis-patient mismatch after aortic valve replacement: impact of age and body size on late survival. Ann Thorac Surg. 2006;81:481–8.
Permanyer E, Estigarribia A-J, Ysasi A, Herrero E, Semper O, Llorens R. St. Jude Medical TrifectaTM aortic valve perioperative performance in 200 patients. Interact Cardiovasc Thorac Surg. 2013;17:669–72.
Kalra A, Rehman H, Ramchandani M, et al. Early Trifecta valve failure: report of a cluster of cases from a tertiary care referral center. J Thorac Cardiovasc Surg. 2017;154:1235–40.
Anselmi A, Ruggieri VG, Lelong B, et al. Mid-term durability of the Trifecta bioprosthesis for aortic valve replacement. J Thorac Cardiovasc Surg. 2017;153:21–28.e1.
Dvir D, Leipsic J, Blanke P, et al. Coronary obstruction in transcatheter aortic valve-in-valve implantation: preprocedural evaluation, device selection, protection, and treatment. Circ Cardiovasc Interv. 2015;8:e002079.
Valvo R, Costa G, Barbanti M. How to avoid coronary occlusion during TAVR valve-in-valve procedures. Front Cardiovasc Med. 2019;6:168.
Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87:235–41.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was obtained from the institutional ethics committee (EC approval no.: NH-RTIICS/AP/031/2019) on 25 September, 2019.
Informed consent
Obtained from all participants in writing.
Statement of Human and animal rights
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Purkayastha, B., Khan, M.W., Saha, A. et al. Mid-term clinical and health-related quality of life outcomes for the Trifecta bioprosthesis. Indian J Thorac Cardiovasc Surg 37, 496–505 (2021). https://doi.org/10.1007/s12055-021-01166-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01166-5