Abstract
Cryptococcus neoformans causes severe disseminated infection in immunocompromised individuals. We report a case of an immunocompetent adult male who presented with treatment-resistant central nervous system manifestations and significant pulmonary disease burden. Hematology and lumbar puncture were positive, aided by computerized tomography-guided histological confirmation. Despite medical therapy, there was inadequate resolution, and surgical resection was performed. On follow-up, investigations showed complete resolution, and the patient has remained disease-free at 5 years. This highlights the importance of looking for other sites in resistant cryptococcal meningitis and the value of cardiothoracic intervention for slowly resolving pulmonary cryptococcomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptococcus neoformans is an opportunistic encapsulated yeast commonly found in soil contaminated with bird excrement. C . neoformans infection can affect both immunosuppressed and immunocompetent individuals. It predominantly causes severe infection in immunocompromised individuals of which 80–90% occur with the advent of human immunodeficiency virus (HIV) infection [1,2,3,4,5].In immune competent hosts, the most commonly affected sites are the lungs and central nervous system, while the lymph nodes usually remain unaffected [6]. Pulmonary manifestations vary from asymptomatic nodular disease, to pneumonitis, pleural effusion, and acute respiratory distress syndrome [1]. Disseminated cryptococcal infection is uncommon and almost always occurs in HIV-infected patients.
The management of asymptomatic pulmonary disease remains controversial, and most cases are carefully observed and followed up [1, 2]. Treatment is only offered for those with extrapulmonary involvement, symptomatic pulmonary disease with positive sputum, evidence of cryptococcaemia, and positive serum cryptococcal antigen titer more than 1: 8. Surgical treatment is usually offered for patients with persistent and refractory pulmonary or bone disease [1].
Case report
We report a case of disseminated cryptococcosis with a large isolated pulmonary nodule and lymph node involvement presenting with symptoms of meningism as well as chest symptoms of cough and fever. A 52-year-old male with no known medical illness, presented with history of non-resolving fever of 2 weeks duration with cough, headache, restlessness, irritability, nausea, and vomiting. He had history of chronic exposure to pigeons in view of his neighbor having an outdoor aviary. On admission, he was febrile with a temperature of 38 °C, restless, tachycardiac but normotensive. His Glasgow Coma Scale was full though he exhibited irritability. He had neck stiffness and bilateral papilloedema but no other focal neurological deficits were noted. Systemic examination was unremarkable.
Hematological investigations including full blood counts, random blood sugar, renal, and liver function tests were within normal limits. Blood culture and sensitivity did not show any evidence of fungaemia. Retroviral disease screen done twice by fourth generation ELISA (enzyme-linked immunosorbent assay) method was negative. However, he was positive for serum cryptococcal antigen with a titer of >1: 512.
Computerized tomography (CT scan of the brain was normal. Therefore, diagnostic lumbar puncture was performed, and cerebrospinal fluid studies revealed raised opening pressure of more than 50 cm of H2O. Typical CSF (cerebrospinal fluid) features of cryptococcal infection were present in this patient including lymphocytosis, low sugars, and high proteins with identification of yeast cells on India ink examination. Cerebrospinal fluid cryptococcal antigen titer was also high with a ratio of more than 1: 512. Fungal culture from cerebrospinal fluid grew C. neoformans species.
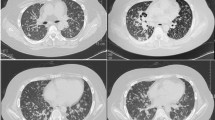
At this point, the Chest X-ray showed evidence of a large mass over the left lower lobe with a size of 5.5 × 6 cm. Computerized tomography of the thorax showed a clearly delineated soft tissue mass of 6.5 cm × 4.0 cm involving the left lower lobe of the lung. Diagnostic Computerized tomography guided biopsy of the lesion was done, and histopathological examination was consistent with pulmonary cryptococcoma. (Figs. 1, 2, and 3).
The patient was diagnosed with disseminated cryptococcus, and intravenous amphotericin was commenced at 1 mg/kg/day in an escalating fashion beginning with a test dose of 1 mg. Intravenous fluconazole was subsequently added at 400 mg/day. Serial lumbar punctures showed normalization of pressures but persistently high proteins, low sugar with lymphocytes thus indicating a possible significant pulmonary foci producing a persistent source of cryptococcaemia. His repeat chest X-ray showed a persistent mass over the left lower lobe. This despite the fact that he had completed 1.5 g of IV amphotericin B after 2 months (i.e., 30 to 50 mg amphotericin per day depending on renal and liver function tests) with fluconazole. In view of the slow resolution of the pulmonary lesion, persistently active CSF (cerebrospinal fluid) findings, ongoing chest symptoms of cough, which had been under-recognized initially and reduced effort tolerance, it was thought that the lung nodule was probably contributing to the slow improvement of his central nervous system pathology. He was referred to the cardiothoracic team for a surgical resection and IV amphotericin was also continued to 2 g cumulative dose post resection over a month.
Surgical resection was carried out, and the lesion was removed en masse and sent for histopathological examination. Intraoperatively, the left lower lobe of the lung was excised. The lesion weighed 139 g, measuring 130 × 7 × 25 mm, nodular in character with a size of about 45 mm in diameter close to the hilar region and partly involving the pleura. Histopathological examination revealed a lung mass consistent with C. neoformans infection. Inflammation was seen to extend close to the hilar lymph nodes showing destruction of normal architecture due to the presence of yeasts. The lymph node sample from the left side of the lungs also showed destruction of normal architecture with secondary histiocytic reaction at the periphery and encapsulated C. neoformans and yeast cells on Hematoxylin and Eosin stains. Intravenous Amphotericin was continued till a total cumulative dose of 2 g/day. (Figs. 2 and 3).
On follow-up, the lung lesion on repeat chest X-rays and CT (Computerized tomography) thorax had completely resolved. Post excision, CSF (cerebrospinal fluid) findings on two subsequent lumbar punctures showed resolution of the cryptococcal infection. He subsequently completed oral fluconazole 400 mg daily which was then reduced to 200 mg daily for a year. At 2 and 5 years post treatment, the patient has remained disease free.
This interesting case highlights the importance of looking for extra-CNS (central nervous system) lesions in slowly resolving cryptococcal meningitis to expedite recovery and the value of cardiothoracic intervention for pulmonary cryptococcomas which are slow to resolve.
Discussion
Several cases of cryptococcal infections in an immunocompetent host have been reported before. Males tend to be more frequently infected than females; our patient was also a male [7]. Pulmonary cryptococcosis has a widely varied presentation from non-specific to even totally silent; therefore it is likely to be misdiagnosed. So a high index of suspicion is warranted [8].The central nervous system is the most common site of dissemination as seen in our patient [9]. Pulmonary cryptococcosis has unpredictable radiological presentations from solitary or multiple subpleural nodules or masses with/without halo signs on CT (computed tomography) scans [10] to consolidations, pleural effusions, and occasional mediastinal lymph node enlargement. Lesions are mainly located in middle and lower lung fields; our patient also had the lesion in the left lower lobe. The main methods of confirmation are lung tissue biopsies and pathological examinations.
It is important to recognize that untreated cryptococcal infection has resulted in severe infections with systemic dissemination even in immune competent hosts [5]. Treatment of systemic manifestations of cryptococcal infections remain debated and non-standardized.
Based on the Clinical Practice Guidelines for the Management of Cryptococcal Disease: 2010 Update by the Infectious Diseases Society of America, Amphotericin B (0.7–1.0 mg/kg per day IV) plus flucytosine (100 mg/kg per day orally in 4 divided doses) are suggested for at least 4 to 6 weeks for induction therapy in immune competent patients. Then, they are commenced on consolidation treatment with fluconazole (400 mg per day) for 8 weeks [1].After induction and consolidation therapy, maintenance therapy with fluconazole (200 mg [3 mg/kg] per day orally) should be continued for 6–12 months. A prompt lumbar puncture is strongly recommended to ascertain baseline CSF (cerebrospinal fluid) pressure provided there is no contraindication to do so [1]. If the CSF (cerebrospinal fluid) pressure is more than 25 cm H20 with symptoms of increased intracranial pressure during induction therapy, relief of CSF (cerebrospinal fluid) pressure by lumbar puncture is suggested to reduce the opening pressure by 50% or to a normal pressure of less than 20 cm H20 [1]. Surgery should also be considered for diagnostic purposes, persistent radiographic abnormalities or symptoms not responding to antifungal therapy [1].
In our patient, after surgical resection of the pulmonary mass and completion of intravenous antifungals, repeated cerebrospinal fluid examination twice revealed negative fungal cultures with biochemistry returning to normal. Post-operative chest X-ray and CT (computed tomography) Thorax showed minimal residual pleural effusion with resolution of fungal mass. Serial serum cryptococcal antigen titers were also on downward trend. At 4 months post-resection, the patient was asymptomatic for pulmonary or central nervous system symptoms and continued to remain well on maintenance Fluconazole for 1 year.
These microorganisms tend to be localized without dissemination in the immune competent, and pulmonary lesions mainly present as solitary or multiple nodules. Though rare in the immunocompetent individuals, disseminated cryptococcocis with pulmonary and CNS involvement needs to be aggressively treated to prevent incomplete resolution. It appears that early removal of a pulmonary cryptococcal focus combined with antifungal agents may give a favorable outcome for meningitis. Combined surgical and antifungal therapy can produce faster clinical improvement and prevent further dissemination and complications. Inoue et al. also reported a favorable outcome for meningitis when early removal of a pulmonary cryptococcal focus is combined with antifungal agents [4].
To conclude, we are in agreement with previous case reports published that combination of surgical and antifungal therapy can produce better outcomes in immunocompetent patients with cryptococcosis infection and more importantly, prevent further dissemination of disease.
References
Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322.
Aberg JA, Mundy LM, Powederly WG. Pulmonary cryptococcosis in patients without HIV infection. Chest. 1999;115:734–40.
Doi SA, Tan CT , Liam CK, Naganathan K. Crypiococcocis at the University Hosital Kuala Lumpur. Trop Doct.1998;28:34–9.
Inoue N, Uozumi T, Yamamoto T, et al. Treatment of cryptococcal meningitis with pulmonary granuloma. J Neurology. 1984;231:109–11.
Núñez M, Peacock JE, Chin R. Pulmonary cryptococcosis in the immunocompetent host: therapy with oral fluconazole—a report of four cases and a review of the literature. Chest. 2000;118:527–34.
Murakami Y, Oki M, Saka H, Kajikawa S, Murakami A, Ishida A. Disseminated cryptococcosis presenting as mediastinal and hilar lymphadenopathy in an immunecompetent patient. Respirol Case Rep. 2016;4:e00167.
Severo CB, Gazzoni AF, Severo LC. Pulmonary cryptococcosis. J Bras Pneumol. 2009;35:1136–44.
Kishi K, Homma S, Kurosaki A, Kohno T. MotoiN. Yoshimura K. Clinical features and high-resolution CT findings of pulmonary cryptococcosis in non-AIDS patients. Respir Med. 2006;100:807–12.
Chang WC, Tzao C, Hsu HH, et al. Pulmonary cryptococcosis: comparison of clinical and radiographic characteristics in immunocompetent and immunocompromised patients. Chest. 2006;129:333–40.
Song KD, Lee KS, Chung MP, et al. Pulmonarycryptococcosis: imaging findings in 23 non-AIDS patients. Korean J Radiol. 2010;11:407–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
Nil
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Viswanathan Shanthakumar, S., Tai, S.M.L., Rais Sanusi, A. et al. Significant pulmonary disease burden in treatment resistant disseminated cryptococcal infection: A case report. Indian J Thorac Cardiovasc Surg 33, 355–358 (2017). https://doi.org/10.1007/s12055-017-0545-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-017-0545-7