Abstract
Chemokines are vital in post-cerebral ischemia inflammatory reactions. We investigate the possible relationship between plasma chemokines and short-term and long-term outcomes after stroke. This study included 235 patients (median age, 72 years; 49.8% female) suffering from ischemic stroke, or transient ischemic attack admitted to the hospital within 24 h of onset. We evaluated chemokines CCL2, CCL5, CXCL8, CXCL9, and CXCL10 in plasma samples collected upon admission. Further, we assessed functional outcomes at 3- and 12-months, all-cause fatality over 5 years, and episodes of delirium within the first 7 days of admission. Multivariate analysis revealed an association between higher CXCL10 levels and an increased risk of poor functional outcomes at 3 months (OR: 3.02, 95%CI: 1.22–7.46, p = 0.016) and 12 months (OR: 2.32, 95%CI: 1.03–5.26, p = 0.043), as well as an increased death risk (HR: 1.79, 95%CI: 1.04–3.07, p = 0.036). High CXCL8 levels independently predicted poor functional outcomes at 12 months (OR: 2.69, 95%CI: 1.39–6.31, p = 0.005) and a higher 5-year case fatality rate (HR: 1.90, 95%CI: 1.23–2.93, p = 0.004). Elevated CXCL9 levels also predicted unfavourable functional outcomes at 12 months (OR: 2.45, 95%CI: 1.07–5.61, p = 0.034). In univariate analysis, increased levels of CXCL8, CXCL9, and CXCL10 showed an association with delirium, although this link was not evident in the multivariate analysis. Plasma CXCL8 and CXCL10 show potential as prognostic biomarkers for stroke outcomes and as therapeutic targets suitable for reverse translation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemokines are a family of small proteins that are secreted and play essential roles in immune cell migration into inflammatory sites [1, 2]. They are classified into four families: C, CC, CXC, and CX3C, based on the number of amino acids between the initial two cysteines.
Postmortem studies on animals and humans have demonstrated that cerebral ischemia initiates the expression of various chemokine classes in the brain, such as CCL2, CCL3, CCL5, CXCL8, CXCL10, and CXCL12 [3, 4]. These molecules are primarily produced by microglia and infiltrating immune cells. They regulate numerous biological processes like cell recruitment, blood–brain barrier permeability, angiogenesis, and neurogenesis. Depending on the timing and pathological conditions, chemokines and their receptors can have both positive and negative effects after a stroke [3, 4]. CCL2 and CCL5 are amongst chemokines that have a dual function in the pathophysiology of cerebral ischemia. On one hand, early after an ischemic stroke, CCL2 and CCL5 can exacerbate cerebral injury by facilitating the breakdown of the blood–brain barrier and promoting leukocyte infiltration in the brain [5,6,7]. Conversely, CCL2 may aid stroke recovery by attracting neural progenitor cells to the brain’s damaged regions [8], whilst CCL5 can safeguard neurons in per-infarct regions through the production of neurotrophic factors [9].
Moreover, chemokines and their receptors could serve as potential therapeutic targets post-stroke. For instance, inhibiting CXCL8 [10] or CCR5 [11] signalling has been observed to decrease brain damage and stimulate neurological repair in animal models of ischemic stroke. Additionally, the intravenous injection of a chemokine-binding protein that interacts with a wide range of chemokines reduced plasma chemokine levels, brain inflammation, and infarct size in mice [12].
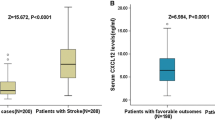
Chemokines are released into the blood during cerebral ischemia. Both brain and peripheral organs, including lymph nodes and adipose tissue, are potential sources of circulating chemokines after stroke [13]. Elevated blood levels of CCL2 [14], CCL5 [15, 16], CXCL1 [16], CXCL5 [16], CXCL8 [17, 18]CXCL9 [19], and CXCL12 [19] have been reported in patients with acute ischemic stroke. In addition, multiple studies have reported an association between circulating chemokines and outcomes after stroke. Higher blood levels of CXCL12 [20], CXCL16 [21], and CCL23 [22] and lower levels of CCL11 [23] were associated with poor functional outcome and/or death.
However, the prognostic value of other chemokines, such as CCL2, CCL5, or CXCL8, which have been studied in animal stroke models, remains unclear. Considering experimental studies hinting at a dual role for chemokines during brain ischemia, further inquiry into their prognostic value in clinical contexts is warranted. Additionally, exploring the relationship between chemokines in the bloodstream and outcomes in stroke patients can help identify potential therapeutic targets worth investigating in reverse translation studies.
Here, we examine the potential correlation between specific plasma chemokines measured during the acute phase of an ischemic stroke and various short-term and long-term outcomes.
Materials and Methods
This study’s participants were chosen from the patients involved in the Prospective Observational Polish Study on Delirium (PROPOLIS). PROPOLIS was a single-centre, prospective study conducted at the Department of Neurology, University Hospital, in Kraków, Poland [24]. Its main goal was to identify the incidence, predictors, and consequences of post-stroke delirium. The study included adults (18 years or older) who were admitted to the hospital within 48 h of having an acute stroke. Patients in a coma, experiencing alcohol withdrawal syndrome, affected by cerebral venous thrombosis or vasculitis, or those with a life expectancy less than 1 year were excluded. The study protocol (KBET/63/B/2014) was approved by the Bioethics Committee of Jagiellonian University, and each participant or their legal guardian provided informed consent. Patients who agreed to participate in PROPOLIS could opt out of blood sampling.
In this sub-study, we included patients who met specific criteria: (1) diagnosis of ischemic stroke or transient ischemic attack (TIA); (2) hospital admission within 24 h of symptom onset; and (3) consent given by the informed patient.
This study’s outcomes included unfavourable functional outcomes at both 3- and 12-month post-stroke, as defined by a modified Rankin Scale score exceeding 2. The study also looked at the 5-year all-cause fatality rate and the occurrence of delirium within the first week of hospital admission. Delirium was selected as a surrogate for short-term cognitive outcomes; this is justified by an increasing body of evidence suggesting chemokines are crucially involved in the pathogenesis of cognitive impairment [25, 26].
During the initial 7 days following admission, we conducted daily examinations for delirium symptoms. We employed the Brief Confusion Assessment Method (bCAM) [27] or the Confusion Assessment Method for Intensive Care Unit Patients (CAM-ICU) [28] and sourced additional information from the patient behaviour and cognitive fluctuation questionnaires completed by nurses. The final diagnosis of delirium was based on the criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
On admission, we evaluated neurological deficits using the National Institute of Health Stroke Scale (NIHSS). Pre-stroke dependency was determined by a score of 3–5 on the mRS scale. Five-year all-cause fatality data were procured from a government-maintained database.
Upon admission, venous blood was collected in heparinised tubes (Sarstedt, Germany), left at room temperature for 30 min, centrifuged, and then stored at -80 °C. We used a cytometric bead array immunoassay to measure CCL2, CCL5, CXCL8, CXCL9, and CXCL10 (Human Chemokine Kit, BD Bioscience, San Diego, CA, USA). Of the patients, 26.0% (61 patients) had CXCL-8 levels below the detection limit. In these instances, we substituted CXCL-8 concentrations with half of the lower limit of quantification.
We compared baseline characteristics and chemokine levels between groups using the χ2 test for proportions and the Mann–Whitney U test for continuous variables. Univariate logistic regression helped assess the associations between chemokines, functional outcomes, and delirium. Cox’s proportional hazard models were applied to analyse the death risk. For each chemokine, multivariate analyses adjusted for clinical predictors with a p-value less than 0.10 in the univariate models. We utilised receiver operating characteristic (ROC) curves and the Youden Index to identify chemokines’ optimal cut-off points to predict functional outcomes or delirium, balancing sensitivity and specificity. For survival analysis, the optimal cut-off points of chemokines were calculated using maximally selected rank statistics. All statistical tests were two-sided. A p-value of 0.05 was the threshold for statistical significance. The “Survminer” package (version 0.4.9) in the R statistical software was used for maximally selected rank statistics, whilst all other statistical analyses were carried out using STATA version 16.
Results
A total of 574 patients met the inclusion criteria, with a median age of 73.5 years (interquartile range [IQR]: 64–82), median NIHSS score of 6 (IQR: 3–15), and 53.1% were female. Amongst these, blood samples were available for 235 patients, with a median age of 72 years (IQR: 63–82), a median NIHSS score of 5 (IQR: 2–11), and 49.8% were female. Out of these, 211 patients (89.8%) had suffered a stroke, and 24 (10.2%) had TIA. No blood samples were available from the remaining 339 patients (median age: 74 years, IQR: 64–82; median NIHSS: 8, IQR: 3–16; 55.8% female), either because they declined blood sampling or because their blood was used in other experiments. Compared to the patients included in the study, those for whom blood samples were not available had a higher admission NIHSS score (p < 0.001), but their ages (p = 0.364) and genders (p = 0.159) were similar.
We had data on delirium and all-cause fatality over 5 years for all patients included in the study. However, we had missing data on functional outcomes at 3 and 12 months for 19 (8.1%) and 16 (6.8%) patients, respectively.
3-Month Functional Outcome
The baseline characteristics of the patients are displayed in Table 1. Of these, 99 patients (accounting for 45.8%) experienced poor functional outcomes 3 months post-stroke.
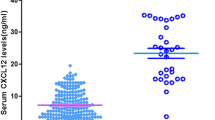
Patients with worse outcomes exhibited heightened levels of CXCL10 (median: 1826 vs 1284.4 pg/ml, p < 0.001), CXCL9 (2346.9 vs 1258.7 pg/ml, p < 0.001), CCL5 (2864.4 vs 2165.2 pg/ml, p = 0.033), and CXCL8 (12.4 vs 6.1 pg/ml, p < 0.001) (Fig. 1). These elevated cytokine levels were associated with negative outcomes in the univariate analysis. However, when adjusting for factors like age, atrial fibrillation, NIHSS score on admission, and pre-stroke dependency in the multivariate analysis, only CXCL10 remained as an independent outcome predictor (Fig. 2).
Chemokine levels stratified by outcomes. Each panel displays a scatter plot of the respective chemokine levels grouped by outcomes: A CXCL10, B CCL2, C CXCL9, D CCL5, E CXCL8. Error bars represent median levels with interquartile ranges. In panel E, data points below the dotted line correspond to CXCL8 values that fell below the quantification limit and were arbitrarily imputed as half of the lower limit of quantification
12-Month Functional Outcome
One hundred and one patients (accounted for 46.1%) demonstrated a poor functional outcome 12 months post-stroke. They were characterised by elevated plasma levels of CXCL10 (1853 vs 1235.9 pg/ml), CXCL9 (2677.2 vs 1038.5 pg/ml), and CXCL8 (13.9 vs 4.5 pg/ml), all with a p-value of less than 0.001. In a univariate analysis, poor outcomes were associated with elevated levels of CXCL10, CXCL9, CCL5, and CXCL8. However, after adjusting for age, hypertension, atrial fibrillation, NIHSS admission score, right-sided lesion, and pre-stroke dependency in a multivariate analysis, only higher levels of CXCL10, CXCL9, and CXCL8 remained independent predictors of outcome.
All-Cause 5-Year Case Fatality
Over 5 years following a stroke, 104 patients (44.3%) passed away. These patients exhibited higher levels of CXCL10 (1841.9 vs 1198.5 pg/ml, p < 0.001), CXCL9 (2683.7 vs 1095.7 pg/ml, p < 0.001), and CXCL8 (13.9 vs 4.5 pg/ml, p < 0.001). Univariate analysis revealed an association between elevated chemokine levels and an increased risk of death. In a multivariate analysis adjusted for age, atrial fibrillation, pre-stroke dependency, NIHSS on admission and right-sided lesion, CXCL10 and CXCL8 still remained independent predictors of death (Table 2).
Delirium
Delirium was observed in 34 patients, comprising 14.5% of the total. These patients showed higher levels of CXCL10 (1868.3 vs 1465.3 pg/ml, p = 0.031) and CXCL8 (15.1 vs 8.0 pg/ml, p = 0.002). Univariate analysis revealed that elevated levels of CXCL10, CXCL9, and CXCL8 were linked to an increased delirium risk. However, a multivariate analysis adjusting for age, diabetes mellitus, atrial fibrillation, pre-stroke dependency, NIHSS admission score, the presence of a right-sided lesion, and reperfusion therapy found that these chemokines could not predict delirium occurrence.
Discussion
We found that higher CXCL10 plasma levels correlate with unfavourable immediate and long-term functional outcomes and a higher fatality rate within 5 years of an ischemic stroke. Additionally, an elevation in CXCL8 blood levels is associated with a greater risk of poor functional outcomes after a year and a higher likelihood of death within 5 years of experiencing a stroke. Furthermore, higher levels of CXCL9 in plasma have been found to predict a poor functional outcome after 1 year.
CXCL10, also known as interferon gamma-induced protein 10, functions as a chemoattractant for monocytes, macrophages, T cells, and natural killer (NK) cells [29]. Animal studies have demonstrated an increased expression of CXCL10 and its receptor, CXCR3, in the ischemic brain [30,31,32]. This is supported by human postmortem analyses, revealing up-regulation of CXCL10 in the brains of ischemic stroke patients [33]. It has also been observed that CXCL10 might exacerbate blood–brain barrier damage caused by NK cells during cerebral ischemia [32]. Interestingly, patients with higher blood levels of CXCL10 have been associated with a worse prognosis following intracerebral haemorrhage [34].
Our study found that plasma CXCL8 (interleukin-8) is linked with long-term outcomes post-stroke. In rabbits exposed to transient cerebral ischemia, CXCL8 levels increased 6 h after reperfusion [10]. CXCL8 is a strong neutrophil chemoattractant, which has an important role in the post-ischemic brain [35]. The reduction of infarct size was observed after either silencing the CXCL8 gene or applying a neutralising anti-CXCL8 antibody [10, 36]. Similarly, using reparixin, a CXCL8 receptor blocker, improved long-term neurological recovery in a cerebral ischemia rat model [37]. In acute ischemic stroke patients, a correlation was found between serum CXCL8, infarct volume, and mRS assessed at 90 days [38].
We discovered that elevated blood levels of CXCL9 indicated a potentially unfavourable functional outcome after 12 months. CXCL9, a chemoattractant for T lymphocytes and NK cells triggered by interferon-gamma [1], is still not clearly understood in the context of cerebral ischemia. However, one study found a correlation between higher serum CXCL9 levels and increased neurological deficits and infarct volume [19].
Delirium is a serious neuropsychiatric syndrome that causes sudden changes in awareness, attention, and cognition [39]. Increased blood levels of CXCL8 have been noted in elderly patients with delirium [40]. However, studies involving critically ill patients have yielded inconsistent results regarding blood CXCL8 levels in delirious patients [41, 42]. Some research has indicated a potential connection between blood CCL2 and delirium [42, 43]. The link between circulating chemokines and post-stroke delirium has not yet been studied. In our research, we found higher levels of CXCL8, CXCL9, and CXCL10 to be associated with delirium in univariate analysis. However, this association disappeared when adjusted for clinical predictors. We must acknowledge the possibility that our sample size was insufficient to confirm a relationship between chemokines and delirium in multivariate analysis.
Our study has several limitations. Firstly, our limited sample size may impact the reliability of our findings. Secondly, selection bias may have occurred as patients without available blood samples were excluded. Thirdly, with 26% of patients having CXCL8 below the quantifiable limit, the precision of CXCL8 measurements and the rigour of statistical analyses might be compromised. Also, we only measured chemokine levels once. More reliable data about the relationship between chemokine kinetics and prognosis could be obtained with multiple measurements of blood chemokines. Lastly, our observation-based approach prevents us from establishing a causal link between chemokines and stroke outcomes.
In conclusion, plasma CXCL8 and CXCL10 show potential as both prognostic biomarkers for stroke outcomes and therapeutic targets. Further research on this topic, specifically using animal models, is warranted.
Data Availability
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Epstein FH, Luster AD (1998) Chemokines — chemotactic cytokines that mediate inflammation. N Engl J Med 338:436–445. https://doi.org/10.1056/nejm199802123380706
Chen K, Bao Z, Tang P, Gong W, Yoshimura T, Wang JM (2018) Chemokines in homeostasis and diseases. Cell Mol Immunol 15:324–334. https://doi.org/10.1038/cmi.2017.134
Lin Y, Chen H, Ai Q, Yang Y, Zhang Z, Chu S, Chen N (2023) Characteristics and pathogenesis of chemokines in the post-stroke stage. Int Immunopharmacol 116:109781. https://doi.org/10.1016/j.intimp.2023.109781
Chen C, Chu S-F, Liu D-D, Zhang Z, Kong L-L, Zhou X, Chen N-H (2018) Chemokines play complex roles in cerebral ischemia. Neurochem Int 112:146–158. https://doi.org/10.1016/j.neuint.2017.06.008
Strecker J-K, Minnerup J, Schütte-Nütgen K, Gess B, Schäbitz W-R, Schilling M (2013) Monocyte chemoattractant protein-1–deficiency results in altered blood–brain barrier breakdown after experimental stroke. Stroke 44:2536–2544. https://doi.org/10.1161/strokeaha.111.000528
Chen Y, Hallenbeck JM, Ruetzler C, Bol D, Thomas K, Berman NEJ, Vogel SN (2003) Overexpression of monocyte chemoattractant protein 1 in the brain exacerbates ischemic brain injury and is associated with recruitment of inflammatory cells. J Cereb Blood Flow Metab 23:748–755. https://doi.org/10.1097/01.wcb.0000071885.63724.20
Terao S, Yilmaz G, Stokes KY, Russell J, Ishikawa M, Kawase T, Granger DN (2008) Blood cell-derived RANTES mediates cerebral microvascular dysfunction, inflammation, and tissue injury after focal ischemia–reperfusion. Stroke 39:2560–2570. https://doi.org/10.1161/strokeaha.107.513150
Yan Y-P, Sailor KA, Lang BT, Park S-W, Vemuganti R, Dempsey RJ (2006) Monocyte chemoattractant protein-1 plays a critical role in neuroblast migration after focal cerebral ischemia. J Cereb Blood Flow Metab 27:1213–1224. https://doi.org/10.1038/sj.jcbfm.9600432
Tokami H, Ago T, Sugimori H, Kuroda J, Awano H, Suzuki K, Kiyohara Y, Kamouchi M et al (2013) RANTES has a potential to play a neuroprotective role in an autocrine/paracrine manner after ischemic stroke. Brain Res 1517:122–132. https://doi.org/10.1016/j.brainres.2013.04.022
Matsumoto T, Ikeda K, Mukaida N, Harada A, Matsumoto Y, Yamashita J, Matsushima K (1997) Prevention of cerebral edema and infarct in cerebral reperfusion injury by an antibody to interleukin-8. Lab Invest 77:119–125
Joy MT, Assayag EB, Shabashov-Stone D, Liraz-Zaltsman S, Mazzitelli J, Arenas M, Abduljawad N, Kliper E et al (2019) CCR5 is a therapeutic target for recovery after stroke and traumatic brain injury. Cell 176:1143-1157.e13. https://doi.org/10.1016/j.cell.2019.01.044
Lee S, Chu HX, Kim HA, Real NC, Sharif S, Fleming SB, Mercer AA, Wise LM et al (2015) Effect of a broad-specificity chemokine-binding protein on brain leukocyte infiltration and infarct development. Stroke 46:537–544. https://doi.org/10.1161/strokeaha.114.007298
Shi J, Li W, Zhang F, Park JH, An H, Guo S, Duan Y, Wu D et al (2021) CCL2 (C-C Motif Chemokine Ligand 2) Biomarker responses in central versus peripheral compartments after focal cerebral ischemia. Stroke 52:3670–3679. https://doi.org/10.1161/strokeaha.120.032782
Bonifačić D, Toplak A, Benjak I, Tokmadžić VS, Lekić A, Kučić N (2016) Monocytes and monocyte chemoattractant protein 1 (MCP-1) as early predictors of disease outcome in patients with cerebral ischemic stroke. Wien Klin Wochenschr 128:20–27. https://doi.org/10.1007/s00508-015-0878-4
Pawluk H, Kołodziejska R, Grześk G, Woźniak A, Kozakiewicz M, Kosinska A, Pawluk M, Grześk-Kaczyńska M et al (2023) The potential role of RANTES in post-stroke therapy. Cells 12:2217. https://doi.org/10.3390/cells12182217
Hazelwood HS, Frank JA, Maglinger B, McLouth CJ, Trout AL, Turchan-Cholewo J, Stowe AM, Pahwa S et al (2022) Plasma protein alterations during human large vessel stroke: a controlled comparison study. Neurochem Int 160:105421. https://doi.org/10.1016/j.neuint.2022.105421
Grau AJ, Reis A, Buggle F, Al-Khalaf A, Werle E, Valois N, Bertram M, Becher H et al (2001) Monocyte function and plasma levels of interleukin-8 in acute ischemic stroke. J Neurol Sci 192:41–47. https://doi.org/10.1016/s0022-510x(01)00590-1
Kostulas N, Pelidou SH, Kivisäkk P, Kostulas V, Link H (1999) Increased IL-1beta, IL-8, and IL-17 mRNA expression in blood mononuclear cells observed in a prospective ischemic stroke study. Stroke 30:2174–2179. https://doi.org/10.1161/01.str.30.10.2174
Han M, Ma B, She R, Xing Y, Li X (2023) Correlations between serum CXCL9/12 and the severity of acute ischemic stroke, a retrospective observational study. Neuropsychiatr Dis Treat 19:283–292. https://doi.org/10.2147/ndt.s391578
Duan X-X, Zhang G-P, Wang X-B, Yu H, Wu J-L, Liu K-Z, Wang L, Long X (2015) The diagnostic and prognostic value of serum CXCL12 levels in patients with ischemic stroke. Neurol Sci 36:2227–2234. https://doi.org/10.1007/s10072-015-2341-8
Ueland T, Smedbakken LM, Hallén J, Atar D, Januzzi JL, Halvorsen B, Jensen JK, Aukrust P (2012) Soluble CXCL16 and long-term outcome in acute ischemic stroke. Atherosclerosis 220:244–249. https://doi.org/10.1016/j.atherosclerosis.2011.10.004
Simats A, García-Berrocoso T, Penalba A, Giralt D, Llovera G, Jiang Y, Ramiro L, Bustamante A et al (2018) CCL23: a new CC chemokine involved in human brain damage. J Intern Med 283:461–475. https://doi.org/10.1111/joim.12738
Roy-O’Reilly M, Ritzel RM, Conway SE, Staff I, Fortunato G, McCullough LD (2017) CCL11 (Eotaxin-1) levels predict long-term functional outcomes in patients following ischemic stroke. Transl Stroke Res 8:578–584. https://doi.org/10.1007/s12975-017-0545-3
Klimiec E, Dziedzic T, Kowalska K, Szyper A, Pera J, Potoczek P, Slowik A, Klimkowicz-Mrowiec A (2015) PRospective Observational POLIsh Study on post-stroke delirium (PROPOLIS): methodology of hospital-based cohort study on delirium prevalence, predictors and diagnostic tools. BMC Neurol 15:94. https://doi.org/10.1186/s12883-015-0351-z
Jorda A, Campos-Campos J, Iradi A, Aldasoro M, Aldasoro C, Vila JM, Valles SL (2019) The role of chemokines in Alzheimer’s disease. Endocr, Metab Immune Disord - Drug Targets 20:1383–1390. https://doi.org/10.2174/1871530320666200131110744
Zhou F, Sun Y, Xie X, Zhao Y (2023) Blood and CSF chemokines in Alzheimer’s disease and mild cognitive impairment: a systematic review and meta-analysis. Alzheimer’s Res Ther 15:107. https://doi.org/10.1186/s13195-023-01254-1
Han JH, Wilson A, Vasilevskis EE, Shintani A, Schnelle JF, Dittus RS, Graves AJ, Storrow AB et al (2013) Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med 62:457–465. https://doi.org/10.1016/j.annemergmed.2013.05.003
Ely EWE, Inouye SKS, Bernard GRG, Gordon SS, Francis JJ, May LL, Truman BB, Speroff TT et al (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA, J Am Med Assoc 286:2703–2710. https://doi.org/10.1001/jama.286.21.2703
Neville LF, Mathiak G, Bagasra O (1997) The immunobiology of interferon-gamma inducible protein 10 kD (IP-10): a novel, pleiotropic member of the C-X-C chemokine superfamily. Cytokine Growth Factor Rev 8:207–219. https://doi.org/10.1016/s1359-6101(97)00015-4
Wang X, Li X, Schmidt DB, Foley JJ, Barone FC, Ames RS, Sarau HM (2000) Identification and molecular characterization of rat CXCR3: receptor expression and interferon-inducible protein-10 binding are increased in focal stroke. Mol Pharmacol 57:1190–1198
Seifert HA, Collier LA, Chapman CB, Benkovic SA, Willing AE, Pennypacker KR (2014) Pro-inflammatory interferon gamma signaling is directly associated with stroke induced neurodegeneration. J Neuroimmune Pharmacol 9:679–689. https://doi.org/10.1007/s11481-014-9560-2
Zhang Y, Gao Z, Wang D, Zhang T, Sun B, Mu L, Wang J, Liu Y et al (2014) Accumulation of natural killer cells in ischemic brain tissues and the chemotactic effect of IP-10. J Neuroinflammation 11:79. https://doi.org/10.1186/1742-2094-11-79
Chaitanya GV, Eeka P, Munker R, Alexander JS, Babu PP (2011) Role of cytotoxic protease granzyme-b in neuronal degeneration during human stroke. Brain Pathol 21:16–30. https://doi.org/10.1111/j.1750-3639.2010.00426.x
Landreneau MJ, Mullen MT, Messé SR, Cucchiara B, Sheth KN, McCullough LD, Kasner SE, Sansing LH, Investigators the SMASCH (SMASCH) (2018) CCL2 and CXCL10 are associated with poor outcome after intracerebral hemorrhage. Ann Clin Transl Neurol 5:962–970. https://doi.org/10.1002/acn3.595
Jickling GC, Liu D, Ander BP, Stamova B, Zhan X, Sharp FR (2015) Targeting neutrophils in ischemic stroke: translational insights from experimental studies. J Cereb Blood Flow Metab 35:888–901. https://doi.org/10.1038/jcbfm.2015.45
Lv H, Li J, Che Y (2019) CXCL8 gene silencing promotes neuroglial cells activation while inhibiting neuroinflammation through the PI3K/Akt/NF-κB-signaling pathway in mice with ischemic stroke. J Cell Physiol 234:7341–7355. https://doi.org/10.1002/jcp.27493
Villa P, Triulzi S, Cavalieri B, Bitondo RD, Bertini R, Barbera S, Bigini P, Mennini T et al (2007) The interleukin-8 (IL-8/CXCL8) receptor inhibitor reparixin improves neurological deficits and reduces long-term inflammation in permanent and transient cerebral ischemia in rats. Mol Med 13:125–133. https://doi.org/10.2119/2007-00008.villa
He Q, Shi X, Zhou B, Teng J, Zhang C, Liu S, Lian J, Luo B et al (2018) Interleukin 8 (CXCL8)-CXC chemokine receptor 2 (CXCR2) axis contributes to MiR-4437-associated recruitment of granulocytes and natural killer cells in ischemic stroke. Mol Immunol 101:440–449. https://doi.org/10.1016/j.molimm.2018.08.002
Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, Slooter AJC, Ely EW (2020) Delirium Nat Rev Dis Primers 6:90. https://doi.org/10.1038/s41572-020-00223-4
de Rooij SE, van Munster BC, Korevaar JC, Levi M (2007) Cytokines and acute phase response in delirium. J Psychosom Res 62:521–525. https://doi.org/10.1016/j.jpsychores.2006.11.013
van den Boogaard M, Kox M, Quinn KL, van Achterberg T, van der Hoeven JG, Schoonhoven L, Pickkers P (2011) Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit Care 15:R297–R297. https://doi.org/10.1186/cc10598
Smith RJ, Rabinstein AA, Cartin-Ceba R, Singh VP, Lachner C, Khatua B, Trivedi S, Gajic O (2022) Chemokines in ICU delirium: an exploratory study. Crit Care Explor 4:e0729. https://doi.org/10.1097/cce.0000000000000729
Kaźmierski J, Miler P, Pawlak A, Jerczyńska H, Woźniak J, Frankowska E, Brzezińska A, Woźniak K et al (2021) Elevated monocyte chemoattractant protein-1 as the independent risk factor of delirium after cardiac surgery. a prospective cohort study. J Clin Med 10:1587. https://doi.org/10.3390/jcm10081587
Author information
Authors and Affiliations
Contributions
Elzbieta Klimiec-Moskal prepared the study protocol; collected, analysed, and interpreted the data; and prepared the manuscript. Piotr Koceniak collected and interpreted the data. Kazimierz Weglarczyk performed the cytometric assay and analysed the data. Agnieszka Slowik and Maciej Siedlar revised the manuscript for intellectual content. Tomasz Dziedzic prepared the study protocol; analysed and interpreted the data; supervised the study; and prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by The Bioethics Committee of Jagiellonian University (KBET/63/B/2014).
Consent to Participate
Each patient or his/her legal guardian gave informed consent to participate in the study before data collection.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klimiec-Moskal, E., Koceniak, P., Weglarczyk, K. et al. Circulating Chemokines and Short- and Long-Term Outcomes After Ischemic Stroke. Mol Neurobiol (2024). https://doi.org/10.1007/s12035-024-04279-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-024-04279-1