Abstract
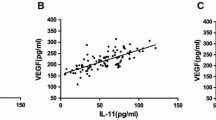
Both angiogenesis and inflammation contribute to activation of matrix metalloproeteinase-9 (MMP-9), which dissolves the extracellular matrix, disrupts the blood–brain barrier, and plays an important role in the pathogenesis of brain arteriovenous malformations (BAVMs). The key common cytokine in both angiogenesis and inflammation is interleukin 6 (IL-6). Previous studies have shown elevated systemic MMP-9 and decreased systemic vascular endothelial growth factor (VEGF) in BAVM patients. However, the clinical utility of plasma cytokines is unclear. The purpose of this study is to explore the relationship between plasma cytokines and the clinical presentations of BAVMs. Prospectively, we recruited naive BAVM patients without hemorrhage as the experimental group and unruptured intracranial aneurysm (UIA) patients as the control group. All patients received digital subtraction angiography, and plasma cytokines were collected from the lesional common carotid artery. Plasma cytokine levels were determined using a commercially available, monoclonal antibody–based enzyme-linked immunosorbent assay. Subgroup analysis based on hemorrhagic presentation and angiograchitecture was done for the BAVM group. Pearson correlations were calculated for the covariates. Means and differences for continuous and categorical variables were compared using Student’s t and χ2 tests respectively. Plasma MMP-9 levels were significantly higher in the BAVM group (42,945 ± 29,991 pg/mL) than in the UIA group (28,270 ± 17,119 pg/mL) (p < 0.001). Plasma MMP-9 levels in epileptic BAVMs (57,065 ± 35,732; n = 9) were higher than in non-epileptic BAVMs (35,032 ± 28,301; n = 19) (p = 0.049). Lower plasma MMP-9 levels were found in cases of BAVM with angiogenesis and with peudophlebitis. Plasma MMP-9 is a good biomarker reflecting ongoing vascular remodeling in BAVMs. Angiogenesis and pseudophlebitis are two angioarchitectural signs that reflect MMP-9 activities and can potentially serve as imaging biomarkers for epileptic BAVMs.






Similar content being viewed by others
Data availability
All patient characteristics and data are available upon requests to the correspondent author.
Code Availability
Not applicable.
Abbreviations
- BAVM:
-
Brain arteriovenous malformation
- IL-1b:
-
Interlukin 1b
- IL-6:
-
Interleukin-6
- MMP-9:
-
Matrix metalloproteinase-9
- TGFα:
-
Tumor growth factor α
- VEGF:
-
Vascular endothelial growth factor
References
Abecassis IJ, Xu DS, Batjer HH, Bendok BR (2014) Natural history of brain arteriovenous malformations: a systematic review. Neurosurg Focus 37:E7. https://doi.org/10.3171/2014.6.focus14250
Al-Shahi R (2001) A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain 124:1900–1926. https://doi.org/10.1093/brain/124.10.1900
Berman MF, Sciacca RR, Pile-Spellman J et al (2000) The epidemiology of brain arteriovenous malformations. Neurosurgery 47:389–397. https://doi.org/10.1097/00006123-200008000-00023
Bharatha A, Faughnan ME, Kim H et al (2012) Brain arteriovenous malformation multiplicity predicts the diagnosis of hereditary hemorrhagic telangiectasia: quantitative assessment. Stroke 43:72–78. https://doi.org/10.1161/strokeaha.111.629865
Dalton A, Dobson G, Prasad M, Mukerji N (2018) De novo intracerebral arteriovenous malformations and a review of the theories of their formation. Brit J Neurosurg 32:305–311. https://doi.org/10.1080/02688697.2018.1478060
Nikolaev SI, Vetiska S, Bonilla X et al (2018) Somatic activating KRAS mutations in arteriovenous malformations of the brain. New Engl J Med 378:250–261. https://doi.org/10.1056/nejmoa1709449
Du R, Hashimoto T, Tihan T et al (2007) Growth and regression of arteriovenous malformations in a patient with hereditary hemorrhagic telangiectasia: Case report. J Neurosurg 106:470–477. https://doi.org/10.3171/jns.2007.106.3.470
Kiliç T, Pamir MN, Küllü S et al (2000) Expression of structural proteins and angiogenic factors in cerebrovascular anomalies. Neurosurgery 46:1179–1192. https://doi.org/10.1097/00006123-200005000-00032
Komiyama M (2016) Pathogenesis of brain arteriovenous malformations. Neurol Med-chir 56:317–325. https://doi.org/10.2176/nmc.ra.2016-0051
Leblanc GG, Golanov E, Awad IA et al (2009) Biology of vascular malformations of the brain. Stroke 40:e694–e702. https://doi.org/10.1161/strokeaha.109.563692
Mouchtouris N, Jabbour PM, Starke RM et al (2014) Biology of cerebral arteriovenous malformations with a focus on inflammation. J Cereb Blood Flow Metabolism Official J Int Soc Cereb Blood Flow Metabolism 35:167–175. https://doi.org/10.1038/jcbfm.2014.179
Chen Y (2006) MMP-9 expression is associated with leukocytic but not endothelial markers in brain arteriovenous malformations. Front Biosci 11:3121. https://doi.org/10.2741/2037
Hashimoto T, Mesa-Tejada R, Quick CM et al (2001) Evidence of increased endothelial cell turnover in brain arteriovenous malformations. Neurosurgery 49:124. https://doi.org/10.1097/00006123-200107000-00019
Starke RM, Komotar RJ, Hwang BY et al (2010) Systemic expression of matrix metalloproteinase-9 in patients with cerebral arteriovenous malformations. Neurosurgery 66:343–8-discussion 348. https://doi.org/10.1227/01.neu.0000363599.72318.ba
Dvorak HF, Brown LF, Detmar M, Dvorak AM (1995) Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathology 146:1029–1039
Ferrara N, Houck KA, Jakeman LB et al (1991) The vascular endothelial growth factor family of polypeptides. J Cell Biochem 47:211–218. https://doi.org/10.1002/jcb.240470305
Hoeben A, Landuyt B, Highley MS et al (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580. https://doi.org/10.1124/pr.56.4.3
Hashimoto T, Wu Y, Lawton MT et al (2005) Coexpression of angiogenic factors in brain arteriovenous malformations. Neurosurgery 56:1058–65; discussion 1058–65. https://doi.org/10.1227/01.neu.0000157925.19676.c3
Kim GH, Hahn DK, Kellner CP et al (2008) Plasma levels of vascular endothelial growth factor after treatment for cerebral arteriovenous malformations. Stroke 39:2274–2279. https://doi.org/10.1161/strokeaha.107.512442
Sandalcioglu IE, Wende D, Eggert A et al (2006) Vascular endothelial growth factor plasma levels are significantly elevated in patients with cerebral arteriovenous malformations. Cerebrovasc Dis 21:154–158. https://doi.org/10.1159/000090526
da Costa L, Wallace MC, ter Brugge KG et al (2009) The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke 40:100–105. https://doi.org/10.1161/strokeaha.108.524678
Benson JC, Chiu S, Flemming K et al (2019) MR characteristics of unruptured intracranial arteriovenous malformations associated with seizure as initial clinical presentation. J Neurointerv Surg 12:186–191. https://doi.org/10.1136/neurintsurg-2019-015021
Shankar JJS, Menezes RJ, Pohlmann-Eden B et al (2012) Angioarchitecture of brain AVM determines the presentation with seizures: proposed scoring system. Am J Neuroradiol 34:1028–1034. https://doi.org/10.3174/ajnr.a3361
Chen Y, Zhu W, Bollen AW et al (2008) Evidence of inflammatory cell involvement in brain arteriovenous malformations. Neurosurgery 62:1340. https://doi.org/10.1227/01.neu.0000312339.62339.fc
Guo WY, Nordell B, Karlsson B et al (1993) Target delineation in radiosurgery for cerebral arteriovenous malformations. Assessment of the value of stereotaxic MR imaging and MR angiography. Acta Radiologica Stock Swed 34:457–63
Joint Writing Group of the Technology Assessment Committee American Society of Interventional and Therapeutic Neuroradiology; Joint Section on Cerebrovascular Neurosurgery a Section of the American Association of Neurological Surgeons and Congress of Neurological Surgeons; Section of Stroke and the Section of Interventional Neurology of the American Academy of Neurology, Atkinson P, Awad I, Batjer H, Dowd C, Furlan A, Giannotta S et al (2001) Reporting terminology for brain arteriovenous malformation clinical and radiographic features for use in clinical trials. Stroke 32:1430–1442. https://doi.org/10.1161/01.STR.32.6.1430
Taeshineetanakul P, Krings T, Geibprasert S et al (2012) Angioarchitecture determines obliteration rate after radiosurgery in brain arteriovenous malformations. Neurosurgery 71:1071–8-discussion 1079. https://doi.org/10.1227/neu.0b013e31826f79ec
Chalouhi N, Ali MS, Jabbour PM et al (2012) Biology of intracranial aneurysms: role of inflammation. J Cereb Blood Flow Metabolism 32:1659–1676. https://doi.org/10.1038/jcbfm.2012.84
Intengan HD, Schiffrin EL (2001) Vascular remodeling in hypertension. Hypertension 38:581–587. https://doi.org/10.1161/hy09t1.096249
Turner RJ, Sharp FR (2016) Implications of MMP9 for blood brain barrier disruption and hemorrhagic transformation following ischemic stroke. Front Cell Neurosci 10:56. https://doi.org/10.3389/fncel.2016.00056
Li X, Wang R, Wang X et al (2013) Relevance of IL-6 and MMP-9 to cerebral arteriovenous malformation and hemorrhage. Mol Med Rep 7:1261–1266. https://doi.org/10.3892/mmr.2013.1332
Wei T, Zhang H, Cetin N et al (2016) Elevated expression of matrix metalloproteinase-9 not matrix metalloproteinase-2 contributes to progression of extracranial arteriovenous malformation. Sci Rep-uk 6:24378. https://doi.org/10.1038/srep24378
Xu Z, Rui Y-N, Hagan JP, Kim DH (2019) Intracranial aneurysms: pathology, genetics, and molecular mechanisms. Neuromol Med 21:325–343. https://doi.org/10.1007/s12017-019-08537-7
Wetzel-Strong SE, Weinsheimer S, Nelson J et al (2021) Pilot investigation of circulating angiogenic and inflammatory biomarkers associated with vascular malformations. Orphanet J Rare Dis 16:372. https://doi.org/10.1186/s13023-021-02009-7
Wang K, Zhao S, Liu B et al (2018) Perturbations of BMP/TGF-β and VEGF/VEGFR signalling pathways in non-syndromic sporadic brain arteriovenous malformations (BAVM). J Med Genet 55:675. https://doi.org/10.1136/jmedgenet-2017-105224
Zhang H-F, Zhao M-G, Liang G-B et al (2013) Expression of pro-inflammatory cytokines and the risk of intracranial aneurysm. Inflammation 36:1195–1200. https://doi.org/10.1007/s10753-013-9655-6
Achrol AS, Pawlikowska L, McCulloch CE et al (2006) Tumor necrosis factor-alpha-238G>A promoter polymorphism is associated with increased risk of new hemorrhage in the natural course of patients with brain arteriovenous malformations. Stroke 37:231–234. https://doi.org/10.1161/01.str.0000195133.98378.4b
Chen Y, Pawlikowska L, Yao JS et al (2006) Interleukin-6 involvement in brain arteriovenous malformations. Ann Neurol 59:72–80. https://doi.org/10.1002/ana.20697
Lin CJ, Yang HC, Chien AC et al (2018) In-room assessment of intravascular velocity from time-resolved rotational angiography in patients with arteriovenous malformation: a pilot study. J Neurointerv Surg 10:580. https://doi.org/10.1136/neurintsurg-2017-013387
Wu C, Ansari SA, Honarmand AR et al (2015) Evaluation of 4D vascular flow and tissue perfusion in cerebral arteriovenous malformations: influence of Spetzler-Martin grade, clinical presentation, and AVM risk factors. Am J Neuroradiol 36:1142–1149. https://doi.org/10.3174/ajnr.a4259
Sho E, Sho M, Singh TM et al (2002) Arterial enlargement in response to high flow requires early expression of matrix metalloproteinases to degrade extracellular matrix. Exp Mol Pathol 73:142–153. https://doi.org/10.1006/exmp.2002.2457
Corti P, Young S, Chen C-Y et al (2011) Interaction between alk1 and blood flow in the development of arteriovenous malformations. Development 138:1573–1582. https://doi.org/10.1242/dev.060467
Hashimoto T, Wen G, Lawton MT et al (2003) Abnormal expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in brain arteriovenous malformations. Stroke 34:925–931. https://doi.org/10.1161/01.str.0000061888.71524.df
Woodside KJ, Hu M, Burke A et al (2003) Morphologic characteristics of varicose veins: possible role of metalloproteinases. J Vasc Surg 38:162–169. https://doi.org/10.1016/s0741-5214(03)00134-4
Bouquier N, Girard B, Arias JA et al (2020) Gelatinase biosensor reports cellular remodeling during epileptogenesis. Frontiers Synaptic Neurosci 12:15. https://doi.org/10.3389/fnsyn.2020.00015
Nagy V, Bozdagi O, Matynia A et al (2006) Matrix metalloproteinase-9 is required for hippocampal late-phase long-term potentiation and memory. J Neurosci 26:1923–1934. https://doi.org/10.1523/jneurosci.4359-05.2006
Szepesi Z, Bijata M, Ruszczycki B et al (2013) Matrix metalloproteinases regulate the formation of dendritic spine head protrusions during chemically induced long-term potentiation. PLoS ONE 8:e63314. https://doi.org/10.1371/journal.pone.0063314
Gore SV, James EJ, Huang L et al (2021) Role of matrix metalloproteinase-9 in neurodevelopmental deficits and experience-dependent plasticity in Xenopus laevis. Elife 10:e62147. https://doi.org/10.7554/elife.62147
Broekaart DWM, Bertran A, Jia S et al (2020) The matrix metalloproteinase inhibitor IPR-179 has antiseizure and antiepileptogenic effects. J Clin Invest 131.https://doi.org/10.1172/jci138332
Zwanenburg A, Vallières M, Abdalah MA et al (2020) The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology 295:328–338. https://doi.org/10.1148/radiol.2020191145
Acknowledgements
We would like to thank Joseph Lavallee for English editing and Miss Hsin-Yi Huang for statistical assistance.
Funding
This work was supported by the Taipei Veterans General Hospital (grant number: V110-C- 056, V110C-080), Taiwan’s Ministry of Science and Technology (grant number: MOST-106–2314-B-010 -015 –MY2, MOST 108–2321-B-010–012-MY2, MOST 109–2314-B-075–055), and the Brain Research Center, National Yang Ming Chiao Tung University from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (grant number: MOE 109BRC-B408) in Taiwan.
Author information
Authors and Affiliations
Contributions
Concept of study design: C.-J. Lin, Y.-T. Liu, H.-M. Wu, and H.-C. Yang. Data collection and statistics: C.-J. Lin, Y.-T. Liu, F.-C. Chang, H.-C. Yang, and K.-D. Liou. Manuscript draft: C.-J. Lin, Y.-S. Hu, C.-C. Lee, and Y.-T. Liu. Integration of the manuscript: C.-J. Lin, W.-Y. Guo, H.-M. Wu, K.-D. Liou, and Y.-T. Liu.
Corresponding author
Ethics declarations
Ethics Approval
All the participants have given their signed informed consent. This study was approved by the local ethnic committee (IRB number: 2020–06-005C).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests. MMP-9 regardless hemorrhage or not.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yo-Tsen Liu and Cheng-Chia Lee contribute equally as first authors.
Rights and permissions
About this article
Cite this article
Liu, YT., Lee, CC., Lin, CF. et al. Plasma Matrix Metalloproeteinase-9 Is Associated with Seizure and Angioarchitecture Changes in Brain Arteriovenous Malformations. Mol Neurobiol 59, 5925–5934 (2022). https://doi.org/10.1007/s12035-022-02958-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02958-5